Abstract
Background
The ductus arteriosus (DA) is critical in maintaining postnatal circulation in neonates with obstructed systemic circulation (OSC) and pulmonary circulation (OPC). We hypothesized that the size of the DA and aortic isthmus (AoI) undergoes adaptive growth in utero to counteract the hemodynamic challenges in these congenital heart diseases (CHD).
Methods
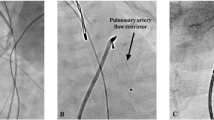
Postnatal echocardiograms of neonates diagnosed prenatally with ductal-dependent CHD who were started on prostaglandins within 24 h of birth were reviewed. We assessed the cross-sectional area of the aortic valve opening, pulmonary valve opening, AoI, and DA by calculating (diameter)2/body surface area. Neonates were classified into OSC or OPC then subgrouped depending upon the patency of semilunar valves: OSC with and without aortic atresia (OSC-AA and OSC-nAA, respectively) and OPC with and without pulmonary atresia (OPC-PA and OPC-nPA, respectively).
Results
Ninety-four cases were studied. The DA in OSC was significantly larger than OPC, and the DA in OSC-AA was significantly larger than OSC-nAA. The size of the AoI was significantly larger in OPC than OSC and larger in OSC-AA than OSC-nAA. Within the OSC-nAA group, there was no significant difference in the size of the DA, AoI, or pulmonary valve opening between those with retrograde flow (RF) at the AoI and without (nRF) except the aortic valve opening was significantly larger in nRF. All groups had comparable cross-sectional areas of systemic output.
Conclusions
Our findings suggest that DA and AoI show compensatory growth to maintain critical blood flow to vital organs against primary anatomical abnormalities in ductus-dependent CHD. (249 words)


Similar content being viewed by others
Abbreviations
- AA:
-
Aortic atresia
- AoI:
-
Aortic isthmus
- AS:
-
Aortic stenosis
- AVO:
-
Aortic valve opening
- BSA:
-
Body surface area
- CoA:
-
Coarctation of aorta
- CCAVC:
-
Complete common atrioventricular canal
- CHD:
-
Congenital heart disease
- DA:
-
Ductus arteriosus
- DAo:
-
Descending aorta
- DORV:
-
Double outlet right ventricle
- HLHS:
-
Hypoplastic left heart syndrome
- IVS:
-
Intact ventricular septum
- LV:
-
left ventricle/ventricular
- MA:
-
Mitral Atresia
- MS:
-
Mitral stenosis
- n:
-
Without
- OPC:
-
Obstructed pulmonary circulation
- OSC:
-
Obstructed systemic circulation
- PA:
-
Pulmonary atresia
- PDA:
-
Patent ductus arteriosus
- PGE1:
-
Prostaglandin E1
- PS:
-
Pulmonary stenosis
- PVO:
-
Pulmonary valve opening
- RF:
-
Retrograde flow
- TOF:
-
tetralogy of Fallot
References
Machii M, Becker AE (1997) Morphologic features of the normal aortic arch in neonates, infants, and children pertinent to growth. Ann Thorac Surg 64:511–515. https://doi.org/10.1016/S0003-4975(97)00445-1
Rudolph AM, Heymann MA, Spitznas U (1972) Hemodynamic considerations in the development of narrowing of the aorta. Am J Cardiol 30:514–525. https://doi.org/10.1016/0002-9149(72)90042-2
Tynan D, Alphonse J, Henry A, Welsh AW (2016) The aortic isthmus: a significant yet underexplored Watershed of the fetal circulation. Fetal Diagn Ther 40:81–93. https://doi.org/10.1159/000446942
Rudolph AM (2010) Congenital cardiovascular malformations and the fetal circulation. Arch Dis Child Fetal Neonatal Ed 95:F132–136. https://doi.org/10.1136/adc.2007.128777
Ruiz A, Cruz-Lemini M, Masoller N, Sanz-Cortes M, Ferrer Q, Ribera I, Martinez JM, Crispi F, Arevalo S, Gomez O, Perez-Hoyos S, Carreras E, Gratacos E, Llurba E (2017) Longitudinal changes in fetal biometry and cerebroplacental hemodynamics in fetuses with congenital heart disease. Ultrasound Obstet Gynecol 49:379–386. https://doi.org/10.1002/uog.15970
Hahn E, Szwast A, Cnota J 2nd, Levine JC, Fifer CG, Jaeggi E, Andrews H, Williams IA (2016) Association between fetal growth, cerebral blood flow and neurodevelopmental outcome in univentricular fetuses. Ultrasound Obstet Gynecol 47:460–465. https://doi.org/10.1002/uog.14881
Mebius MJ, Clur SAB, Vink AS, Pajkrt E, Kalteren WS, Kooi EMW, Bos AF, du Marchie Sarvaas GJ, Bilardo CM (2019) Growth patterns and cerebroplacental hemodynamics in fetuses with congenital heart disease. Ultrasound Obstet Gynecol 53:769–778. https://doi.org/10.1002/uog.19102
Kowalski WJ, Dur O, Wang Y, Patrick MJ, Tinney JP, Keller BB, Pekkan K (2013) Critical transitions in early embryonic aortic arch patterning and hemodynamics. PLoS ONE 8:e60271. https://doi.org/10.1371/journal.pone.0060271
Lindsey SE, Menon PG, Kowalski WJ, Shekhar A, Yalcin HC, Nishimura N, Schaffer CB, Butcher JT, Pekkan K (2015) Growth and hemodynamics after early embryonic aortic arch occlusion. Biomech Model Mechanobiol 14:735–751. https://doi.org/10.1007/s10237-014-0633-1
Rudolph AM, Heymann MA (1970) Circulatory changes during growth in the fetal lamb. Circ Res 26:289–299. https://doi.org/10.1161/01.res.26.3.289
Fouron JC (2003) The unrecognized physiological and clinical significance of the fetal aortic isthmus. Ultrasound Obstet Gynecol 22:441–447. https://doi.org/10.1002/uog.911
Kowalski WJ, Pekkan K, Tinney JP, Keller BB (2014) Investigating developmental cardiovascular biomechanics and the origins of congenital heart defects. Front Physiol 5:408. https://doi.org/10.3389/fphys.2014.00408
Kelly RG (2012) The second heart field. Curr Top Dev Biol 100:33–65. https://doi.org/10.1016/B978-0-12-387786-4.00002-6
Jiang X, Rowitch DH, Soriano P, McMahon AP, Sucov HM (2000) Fate of the mammalian cardiac neural crest. Development 127:1607–1616. https://doi.org/10.1242/dev.127.8.1607
Wang Y, Dur O, Patrick MJ, Tinney JP, Tobita K, Keller BB, Pekkan K (2009) Aortic arch morphogenesis and flow modeling in the chick embryo. Ann Biomed Eng 37:1069–1081. https://doi.org/10.1007/s10439-009-9682-5
Lindsey SE, Butcher JT, Yalcin HC (2014) Mechanical regulation of cardiac development. Front Physiol 5:318. https://doi.org/10.3389/fphys.2014.00318
De Mey JG, Schiffers PM, Hilgers RH, Sanders MM (2005) Toward functional genomics of flow-induced outward remodeling of resistance arteries. Am J Physiol Heart Circ Physiol 288:H1022–1027. https://doi.org/10.1152/ajpheart.00800.2004
Heymann MA, Rudolph AM (1972) Effects of congenital heart disease on fetal and neonatal circulations. Prog Cardiovasc Dis 15:115–143. https://doi.org/10.1016/0033-0620(72)90015-1
Yokoyama U, Ichikawa Y, Minamisawa S, Ishikawa Y (2017) Pathology and molecular mechanisms of coarctation of the aorta and its association with the ductus arteriosus. J Physiol Sci 67:259–270. https://doi.org/10.1007/s12576-016-0512-x
Bergwerff M, Verberne ME, DeRuiter MC, Poelmann RE, Gittenberger-de Groot AC (1998) Neural crest cell contribution to the developing circulatory system: implications for vascular morphology? Circ Res 82:221–231. https://doi.org/10.1161/01.res.82.2.221
Bergwerff M, DeRuiter MC, Hall S, Poelmann RE, Gittenberger-de Groot AC (1999) Unique vascular morphology of the fourth aortic arches: possible implications for pathogenesis of type-B aortic arch interruption and anomalous right subclavian artery. Cardiovasc Res 44:185–196. https://doi.org/10.1016/s0008-6363(99)00186-8
Friedman AH, Fahey JT (1993) The transition from fetal to neonatal circulation: normal responses and implications for infants with heart disease. Semin Perinatol 17:106–121
Kiserud T, Acharya G (2004) The fetal circulation. Prenat Diagn 24:1049–1059. https://doi.org/10.1002/pd.1062
Donofrio MT, Bremer YA, Schieken RM, Gennings C, Morton LD, Eidem BW, Cetta F, Falkensammer CB, Huhta JC, Kleinman CS (2003) Autoregulation of cerebral blood flow in fetuses with congenital heart disease: the brain sparing effect. Pediatr Cardiol 24:436–443. https://doi.org/10.1007/s00246-002-0404-0
Giussani DA (2016) The fetal brain sparing response to hypoxia: physiological mechanisms. J Physiol 594:1215–1230. https://doi.org/10.1113/JP271099
Giussani DA, Davidge ST (2013) Developmental programming of cardiovascular disease by prenatal hypoxia. J Dev Orig Health Dis 4:328–337. https://doi.org/10.1017/S204017441300010X
Cohn HE, Sacks EJ, Heymann MA, Rudolph AM (1974) Cardiovascular responses to hypoxemia and acidemia in fetal lambs. Am J Obstet Gynecol 120:817–824. https://doi.org/10.1016/0002-9378(74)90587-0
Modena A, Horan C, Visintine J, Chanthasenanont A, Wood D, Weiner S (2006) Fetuses with congenital heart disease demonstrate signs of decreased cerebral impedance. Am J Obstet Gynecol 195:706–710. https://doi.org/10.1016/j.ajog.2006.05.045
Kaltman JR, Di H, Tian Z, Rychik J (2005) Impact of congenital heart disease on cerebrovascular blood flow dynamics in the fetus. Ultrasound Obstet Gynecol 25:32–36. https://doi.org/10.1002/uog.1785
Arduini M, Rosati P, Caforio L, Guariglia L, Clerici G, Di Renzo GC, Scambia G (2011) Cerebral blood flow autoregulation and congenital heart disease: possible causes of abnormal prenatal neurologic development. J Matern Fetal Neonatal Med 24:1208–1211. https://doi.org/10.3109/14767058.2010.547961
Blanco P (2020) Rationale for using the velocity-time integral and the minute distance for assessing the stroke volume and cardiac output in point-of-care settings. Ultrasound J 12:21. https://doi.org/10.1186/s13089-020-00170-x
Acknowledgements
We thank Ms. Kimberley Eissmann for her editing of the manuscript text.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
TT conceptualized the study design. DV created an initial database of the study cohort. All authors participated in data collection. LH, AMB, and TT analyzed the collected data, and LH and TT summarized the data and created the Tables and Figures. LH wrote an original draft, which was repeatedly edited by TT and AMB. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
Authors have no financial or non-financial interests that are directly or indirectly related the work submitted for the publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hashim, L., Vari, D., Bhat, A.M. et al. Adaptive Growth of the Ductus Arteriosus and Aortic Isthmus in Various Ductus-Dependent Complex Congenital Heart Diseases. Pediatr Cardiol (2023). https://doi.org/10.1007/s00246-023-03236-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00246-023-03236-4