Abstract
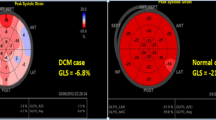
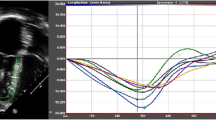
Left ventricular outflow tract velocity time integral (LVOT-VTI), a Doppler-derived measure of stroke distance, is used as a surrogate marker of cardiac function in adults. LVOT-VTI is easily obtained, independent of ventricular geometry and wall motion abnormalities. We investigated the relationship between LVOT-VTI and conventional measures of function in young patients by comparing controls to children with dilated cardiomyopathy (DCM). Sixty-two healthy and 52 DCM patients over 1 year were studied retrospectively. The average pulsed (PW) and continuous wave (CW) LVOT-VTIs from apical views were measured from three cycles. Body surface area (BSA) and Ejection fraction (EF) were obtained. We compared LVOT-VTIs between study and control groups and assessed BSA’s impact on LVOT-VTI. The entire cohort was classified into three levels of LV function which were compared. We determined LVOT-VTI cutoff values that indicated an EF <50%. The mean PW-LVOT-VTI in the DCM group was significantly lower than that of the normal group (0.15 vs. 0.18 m; p < 0.0012). The mean CW-LVOT-VTI was significantly lower in DCM (0.20 vs. 0.24 m; p < 0.0001). There was no impact of BSA on LVOT-VTI except when comparing BSA and CW-LVOT-VTI in the normal group. There was a positive relationship between LVOT-VTI and EF for PW (Rs = 0.29, p = 0.0022) and CW (Rs = 0.22, p = 0.0364) and a difference in mean LVOT-VTI between EF groups (p < 0.0001). ROC analysis demonstrated that PW-LVOT-VTI <0.17 m (AUC = 0.73; p < 0.0001) and CW-LVOT-VTI <0.22 m (AUC = 0.76; p < 0.0001) was associated with EF <50%. This study indicates that LVOT-VTI can be a useful alternative measure of LV performance in children over 1 year.




Similar content being viewed by others
References
Hanseus K, Bjorkhem G, Lundstrom NR (1994) Cardiac function in healthy infants and children: Doppler echocardiographic evaluation. Pediatr Cardiol 15(5):211–218
Thomas DE, Yousef ZR, Fraser AG (2009) A critical comparison of echocardiographic measurements used for optimizing cardiac resynchronization therapy: stroke distance is best. Eur J Heart Fail 11(8):779–788
Childs C, Goldring S, Tann W, Hillier VF (1998) Suprasternal Doppler ultrasound for assessment of stroke distance. Arch Dis Child 79(3):251–255
Goldman JH, Schiller NB, Lim DC, Redberg RF, Foster E (2001) Usefulness of stroke distance by echocardiography as a surrogate marker of cardiac output that is independent of gender and size in a normal population. Am J Cardiol 87(4):499–502
Haites NE, McLennan FM, Mowat DH, Rawles JM (1984) How far is the cardiac output? Lancet 324(8410):1025–1027
Mowat DH, Haites NE, Rawles JM (1983) Aortic blood velocity measurement in healthy adults using a simple ultrasound technique. Cardiovasc Res 17(2):75–80
Haites NE, McLennan FM, Mowat DH, Rawles JM (1985) Assessment of cardiac output by the Doppler ultrasound technique alone. Br Heart J 53(2):123–129
Huntsman LL, Stewart DK, Barnes SR, Franklin SB, Colocousis JS, Hessel EA (1983) Noninvasive Doppler determination of cardiac output in man. Clin Validat Circ 67(3):593–602
Stevens SM, Farzaneh-Far R, Na B, Whooley MA, Schiller NB (2009) Development of an echocardiographic risk-stratification index to predict heart failure in patients with stable coronary artery disease: the heart and soul study. JACC Cardiovasc Imaging 2(1):11–20
Ristow B, Na B, Ali S, Whooley MA, Schiller NB (2011) Left ventricular outflow tract and pulmonary artery stroke distances independently predict heart failure hospitalization and mortality: the heart and soul study. J Am Soc Echocardiogr 24(5):565–572
Richardson JR, Ferguson J, Hiscox J, Rawles J (1998) Non-invasive assessment of cardiac output in children. J Accid Emerg Med 15(5):304–307
Pees C, Glagau E, Hauser J, Michel-Behnke I (2013) Reference values of aortic flow velocity integral in 1193 healthy infants, children, and adolescents to quickly estimate cardiac stroke volume. Pediatr Cardiol 34(5):1194–1200
Poutanen T, Tikanoja T, Sairanen H, Jokinen E (2006) Normal mitral and aortic valve areas assessed by three- and two-dimensional echocardiography in 168 children and young adults. Pediatr Cardiol 27(2):217–225
Poutanen T, Tikanoja T, Sairanen H, Jokinen E (2003) Normal aortic dimensions and flow in 168 children and young adults. Clin Physiol Funct Imaging 23(4):224–229
Margossian R, Chen S, Sleeper LA et al (2015) The reproducibility and absolute values of echocardiographic measurements of left ventricular size and function in children are algorithm dependent. J Am Soc Echocardiogr 28(5):549–558
Wyatt HL, Meerbaum S, Heng MK, Gueret P, Corday E (1980) Cross-sectional echocardiography. III. Analysis of mathematic models for quantifying volume of symmetric and asymmetric left ventricles. Am Heart J 100(6 Pt 1):821–828
Trent RJ, Rawles JM (1999) Risk stratification after acute myocardial infarction by Doppler stroke distance measurement. Heart 82(2):187–191
Volpi A, De Vita C, Franzosi MG et al (1993) Determinants of 6-month mortality in survivors of myocardial infarction after thrombolysis. Results of the GISSI-2 data base. The Ad hoc Working Group of the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI)-2 Data Base. Circulation 88(2):416–429
Punn R, Axelrod DM, Sherman-Levine S, Roth SJ, Tacy TA (2014) Predictors of mortality in pediatric patients on venoarterial extracorporeal membrane oxygenation. Pediatr Crit Care Med 15(9):870–877
Light LH (1978) Implications of aortic blood velocity measurements in children [proceedings]. J Physiol 285:17–18
Jansen AH, Bracke FA, van Dantzig JM et al (2006) Correlation of echo-Doppler optimization of atrioventricular delay in cardiac resynchronization therapy with invasive hemodynamics in patients with heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol 97(4):552–557
Acknowledgements
The authors wish to thank B. Rajaratnam and Sang Oh from the Department of Statistics, Stanford University for their help with the initial statistical analysis and data handling.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Navaratnam, M., Punn, R., Ramamoorthy, C. et al. LVOT-VTI is a Useful Indicator of Low Ventricular Function in Young Patients. Pediatr Cardiol 38, 1148–1154 (2017). https://doi.org/10.1007/s00246-017-1630-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-017-1630-9