Abstract
The arterial switch operation (ASO) for neonates is the standard management for transposition of the great arteries (TGA) with an intact ventricular septum (IVS). Patients presenting for late ASO are at risk due to the possibility of left ventricle (LV) involution. This study aimed to assess the early postoperative course and outcome for children with TGA/IVS and still conditioned LV presenting for late primary ASO. A retrospective study of all TGA/IVS patients who underwent a primary ASO between March 2002 and March 2008 was conducted. The cases were divided into two groups. Group A included all the cases of early ASO repaired before the age of 3 weeks, whereas group B included all the preslected cases of late ASO repaired after the age of 3 weeks. The demographics, intensive care unit (ICU) parameters, complications, and short-term outcomes of the two groups were compared. The study enrolled of 91 patients: 64 patients (70%) in group A and 27 patients (30%) in group B. The mean age was 11 ± 4 days in group A and 37 ± 17 days in group B (P < 0.001). The two groups showed no significant statistical differences in ICU parameters, complications, or mortality. For patients with TGA/IVS, ASO still can be tolerated beyond the first month of life in selected cases. Provided the LV still is conditioned, age should not be a limitation for ASO.
Similar content being viewed by others
The current surgical management for transposition of the great arteries (TGA) with an intact ventricular septum (IVS) involves an arterial switch operation (ASO) within the first 3 weeks of life [1–3]. Beyond this age, surgical management is controversial [2, 4–7] because the natural history of TGA/IVS is characterized by progressive involution of the left ventricle (LV), which may not function well at systemic pressure and resistance in older infants. This situation may place some infants with subsystemic LV pressure at risk for low cardiac output and LV failure after ASO [8, 9].
Occasionally, patients with TGA/IVS cannot undergo early ASO because of late presentation, late diagnosis or referral, intercurrent medical problems such as necrotizing enterocolitis, or other conditions such as sepsis. The alternative managements generally used for this group of patients are the Senning procedure, the Mustard procedure, or two-stage repair involving the use of a pulmonary artery band to prepare the LV for a later ASO [5]. The short- and long-term outcomes for these surgical alternatives are much less favorable than that for primary ASO. For this reason, trials have been conducted to extend the age limit for the primary ASO beyond the first 3 weeks of life to include a larger number of patients. Recently, encouraging reports about the outcome of primary repair for late-presenting patients with TGA/IVS opened the discussions again regarding the age limit for the primary repair [2].
Study Aim
This study aimed to investigate the early postoperative course and outcome for children with TGA/IVS undergoing late primary ASO. The differences in the early postoperative course and outcome between selected patients undergoing late repair (after the age of 3 weeks) and patients who had an early repair (within the first 3 weeks of life) were reviewed.
Methods
Patients
A retrospective study investigated all patients with TGA/IVS who underwent a primary arterial switch repair at the King Abdulaziz Cardiac Center between March 2002 and March 2008. The cases were divided into two groups. Group A included patients who had undergone primary ASO before the age of 3 weeks, whereas group B included preselected patients who had undergone primary ASO after the age of 3 weeks. The study excluded patients who had a deconditioned LV, as proved by a preoperative echocardiographic (ECHO) study, and these patients were submitted to either two-stage repair (prepared by pulmonary artery banding) or an atrial switch operation (Senning or Mustard).
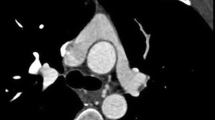
Echocardiography
Transthoracic ECHO evaluation was performed for each patient preoperatively using an HP–Sonos-5500 machine (Hewlette Packard company, Houston, TX, USA). The studies included the standard views (subcostal, apical, parasternal long- and short-axis, and suprasternal views). The LV condition was assessed by measuring the LV posterior wall thickness in diastole at the midcavity level. The LV geometry was classified as type 1 (a well-conditioned LV (Video-1, see Electronic Supplementary Material)), type 2 (between types 1 and 3), or type 3 (a deconditioned LV) (Figs. 1, 2). The study excluded patients with a deconditioned LV (type 3) from the study (Video-2, see Electronic Supplementary Material).
Preoperative Management
Most of the patients submitted to late arterial switch had undergone a balloon atrial septostomy (BAS) earlier in life before their transfer to our center (52%), whereas the patients who went for early ASO were either receiving prostaglandin at the time of surgery or had a BAS performed at our center (44%).
Surgical Technique
The surgical technique used was first described by Jatene who used the Lecompt maneuver to transpose the pulmonary artery to the anterior position. The standard steps include cannulation, cardioplegia, transsection of the great arteries, coronary mobilization, coronary and aortic anastomoses, closure of the atrial septal defect, patch closure of the coronary donor sites, the LeCompte maneuver, completion of the pulmonary anastomosis, and finally, decannulation. Hypothermic myocardial protection was provided by core cooling to a rectal temperature of 28°C, followed by aortic cross-clamping and infusion of a cool crystalloid cardioplegia.
At completion of the repair and after extracorporeal circulation had been finalized, a controlled ultrafiltration was performed with two aims: to eliminate the inflammatory mediators from the blood (cytokines) and to decrease the fluid load that would accumulate in the extracellular space. If these measures were not sufficient and the patient had severe edema with hemodynamic compromise, we elected to delay the sternal closure until the patient stabilized. In selected cases, a peritoneal dialysis catheter also was inserted.
Postoperative Management
Postoperative care in the form of maintaining adequate homeostasis and a high-flow, low-resistance circulation was our target, which typically was achieved with the help of inodilators, vasodilators, and inotropes, which were used in almost all cases,. In addition, we targeted adequate urinary output, peripheral temperature, and absence of high-core temperature. Acidosis in blood gases was avoided. Early peritoneal dialysis, additional inotropic support, and extracorporeal membrane oxygenation (ECMO) were used when necessary.
The infants were weaned off the ventilator after hemodynamic stabilization. Inotropic support was gradually withdrawn, and the children were shifted out of the intensive care unit (ICU).
Results
Of the 146 patients with TGA who underwent surgery during the study period, 98 had a TGA/IVS. Of these 98 patients, 91 had a primary ASO and were included in the study. Five of these patients had a rapid two-stage repair, whereas two patients underwent a Mustard operation. There were 64 patients (70%) in group A and 27 patients (30%) in group B. The average age was 11 ± 4 days in group A and 37 ± 17 days in group B (P < 0.001), There were no other statistically significant differences in the ICU parameters including the inotropic support (number, duration, or doses), ventilation time, ICU stay, hospital stay (Table 1), complications (Table 2) or mortality rate between the two groups. The hospital mortality rate for both groups was 4.4%. There were two mortalities in group A (3.1%), both of which were early, and two mortalities in group B (7%), one early and one late. Although the mortality rate was slightly higher in group B, the difference was not statistically significant (P = 0.73).
Balloon atrial septostomy (BAS) was performed for 28 patients (44%) in group A and 14 patients (52%) in group B. Mechanical hemodynamic support was used for one patient in group B (3.75%) but was not required in group A. Delayed sternal closure was performed for 13 patients (20%) in group A, whereas 4 patients (15%) in group B required delayed sternal closure (P = 0.75) (Table 2).
Discussion
The surgical management for TGA/IVS beyond the age of 3 weeks still is controversial. The concern regarding deconditioning of the LV and inability to handle the systemic circulation was always considered a contraindication for ASO beyond the age of 3 weeks [2, 10].
Traditionally, it has been accepted that the LV can sustain the systemic circulation up to the age of 21 days. Hence, ASO ordinarily is offered to neonates with TGA/IVS who are younger than 21 days. A wide variation exists in the rate of preoperative LV deconditioning. The size of the interatrial communication and duct clearly influences LV preload and afterload, but other factors, possibly genetically predetermined, also may play a role in dictating the involution of pulmonary vascular resistance and LV performance [3].
Furthermore, some patients with TGA are known to have an associated pulmonary hypertension, whereas others may continue to have high pulmonary vascular resistance that does not fall as expected normally for babies at the age of 1 month [11]. Indeed, it is possible that in the presence of a high pulmonary blood flow (because of the patent arterial ductus) together with some degree of postcapillary pulmonary hypertension (related to a restrictive oval foramen) or precapillary pulmonary hypertension (related to a patent arterial duct), the LV can grow and retain the capacity to develop systemic pressures and remain well conditioned after several weeks of life. This theory is supported by recent reports showing the success of primary ASO for patients with TGA/IVS beyond the presumed cutoff age limit of 3 weeks, suggesting an extension of this limit [2, 3, 12]. The explanation for continuing trials to extend the age limit for this group of patients is that the ASO results have been proved and accepted worldwide as superior to the other proposed surgical options such as Senning and Mustard procedures [3].
The other surgical alternative for this group of patients is to retrain the LV by pulmonary artery banding (PAB) for 1 to 2 weeks before the ASO [6, 7]. It is believed that rapid LV training leads to LV remodeling as a result of increased LV afterload, LV wall shear stress, and LV volume overload. This remodeling improves the performance of the LV in adapting to the systemic circulation. This approach has been adopted in many centers with variable success [5, 10].
The approach of rapid LV retraining by PAB compared with the primary ASO was found to have a less favorable outcome, with higher mortality and morbidity rates, prolonged ICU stay with increased risk of nosocomial infection, and increasing hospital costs. Added that, reports described an increased incidence of late LV dysfunction, increased incidence of neoaortic regurgitation, and right ventricular outflow tract obstruction [3, 7]. Despite all these complications, which commonly occur with the two-stage ASO, it remains a better approach than the atrial switch procedures (Senning and Mustard surgery), which also have many postoperative complications, especially the common atrial arrhythmias and LV dysfunction [3].
The potential for improved preservation of systemic ventricular function with ASO became the most pressing reason for considering ASO rather than Senning surgery for infants presenting late [13]. There is evidence that by adopting appropriate perioperative support, which may include the use of LV assist devices or ECMO, ASO can be performed as a primary procedure for patients up to the age of 2 months even if there is echocardiographic or catheter evidence of low LV pressures [2, 12].
For older patients with TGA/IVS, adaptation of the LV to the acutely increased work after ASO may take longer. Multiple studies have shown the success of primary ASO in late presenters with TGA/IVS. Kang et al. [3] published their series of primary ASO for infants older than 21 days, comparing the outcomes with those of ASO for infants younger than 21 days. They found only a 3.8% operative mortality rate in “late switch” group and a greater need for ECMO in this group. Davis et al. [12] reported on 18 infants older than 21 days who underwent primary ASO with only one mortality. Duncan et al. [14] reported on eight infants ages 15 to 46 days who underwent primary ASO with no mortality.
In our series, the mortality rate for the late ASO was 7%, which was slightly higher than the mortality rate for the early ASO (3.1%). However, this difference was not statistically significant (P = 0.73). There is evidence that performing late ASO remains associated with prolonged ventilatory support, a longer hospital stay, a greater need for mechanical LV support, and delayed sternal closure [6]. In our series, however there was no statistically significant difference in these postoperative parameters or complications (Tables 1, 2). The greater need for mechanical support for the late ASO patients was not evident in our study because we had only one patient in this group who required ECMO support, and no patients required ECMO support in the early group (P = 0.65).
Our study had some limitations. We did not calculate the LV mass index, which is one of the tools used in LV assessment. However, we depended on other echocardiographic assessment tools including LV posterior wall thickness, LV end-diastolic internal diameter, LV cavity shape, and interventricular septum thickness and movement [2, 3].
Other limitations to our study were the retrospective nature of the study and an inability to analyze the factors that could delay the involution of the LV, especially the effects of pulmonary artery pressure, pulmonary vascular resistance, patent ductus arteriosus size, and the interatrial communication. These effects may have a significant role in determining the pressure and volume load of LV and its susceptibility for developing involution [2, 3, 12]. Nevertheless, our results are consistent with previously published reports and support extending the age limit for primary arterial operation and individualizing the decision as long as the ECHO data show a fairly conditioned LV.
Conclusion
The ASO for patients with TGA/IVS still can be tolerated beyond the first month of life. Encouraging results of primary ASO for patients with TGA/IVS older than 3 weeks allow us to report that provided the LV remains well conditioned, children older than 3 weeks with TGA/IVS can safely undergo primary ASO. Further studies are required to redefine the age limit for late presenters with TGA/IVS.
References
Kirklin J, Barratt-Boyes B (1993) Cardiac surgery. Churchill Livingstone, New York, pp 1383–1467
Foran JP, Sullivan ID, Elliott MJ, de Leval MR (1998) Primary arterial switch operation for transposition of the great arteries with intact ventricular septum in infants older than 21 days. J Am Coll Cardiol 31:883–889
Kang N, de Leval MR, Elliott M, Tsang V, Kocyildirim E, Sehic I, Foran J, Sullivan I (2004) Extending the boundaries of the primary arterial switch operation in patients with transposition of the great arteries and intact ventricular septum. Circulation 110:123–127
Kirklin JW, Blackstone EH, Tchervenkov CI, Castaneda AR (1992) Clinical outcomes after the arterial switch operation for transposition: patient, support, procedural, and institutional risk factors. Congenital Heart Surgeons Society. Circulation 86:1501–1515
Jonas RA, Giglia TM, Sanders SP, Wernovsky G, Nadal-Ginard B, Mayer JE Jr, Castaneda AR (1989) Rapid two-stage arterial switch for transposition of the great arteries and intact ventricular septum beyond the neonatal period. Circulation 80:1203–1208
Lacour-Gayet F, Piot D, Zoghbi J, Serraf A, Gruber P, Mace L, Touchot A, Planché C (2001) Surgical management and indication of left ventricular retraining in arterial switch for transposition of the great arteries with intact ventricular septum. Eur J Cardiothorac Surg 20:824–829
Boutin C, Wernovsky G, Sanders SP, Jonas RA, Castaneda AR, Colan SD (1994) Rapid two-stage arterial switch operation: evaluation of left ventricular systolic mechanics late after an acute pressure overload stimulus in infancy. Circulation 90:1294–1303
Kirklin JK, Pacifico AD, Kirklin JW (1987) Intraventricular tunnel repair of double outlet right ventricle. J Card Surg 2:231–245
Weyman AE, Wann S, Feigenbaum H, Dillon JC (1976) Mechanism of abnormal septal motion in patients with right ventricular volume overload: a cross-sectional echocardiographic study. Circulation 54:179–186
Norwood WI, Dobell AR, Freed MD, Kirklin JW, Blackstone EH (1988) Intermediate results of the arterial switch repair: a 20-institution study. J Thorac Cardiovasc Surg 96:854–863
Luciani GB, Chang AC, Starnes VA (1996) Surgical repair of transposition of the great arteries in neonates with persistent pulmonary hypertension. Ann Thorac Surg 61:800–804
Davis AM, Wilkinson JL, Karl TR, Mee RB (1993) Transposition of the great arteries with intact ventricular septum: arterial switch repair in patients 21 days of age or older. J Thorac Cardiovasc Surg 106:111–115
Gewillig M, Cullen S, Mertens B, Lesaffre E, Deanfield J (1991) Risk factors for arrhythmia and death after Mustard operation for simple transposition of the great arteries. Circulation 84(5 Suppl):III187–III192
Duncan BW, Poirier NC, Mee RB, Drummond-Webb JJ, Qureshi A, Mesia CI, Graney JA, Malek CL, Latson LA (2004) Selective timing for the arterial switch operation. Ann Thorac Surg 77:1691–1696; discussion 1697
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Movie 1
A two-dimensional short-axis echocardiographic (ECHO) view of a patient from group A showing a well-conditioned left ventricle (posterior chamber). The left ventricle has adequate shape, function, left ventricular posterior wall thickness, and interventricular septal thickness
Movie 2
A two-dimensional short-axis echocardiographic (ECHO) view for a patient with a deconditioned left ventricle showing the left ventricle banana shaped and squashed, thinning of the left ventricle (LV) posterior wall, and bulging of the interventricular septum toward the LV
Rights and permissions
About this article
Cite this article
Ismail, S.R., Kabbani, M.S., Najm, H.K. et al. Early Outcome for the Primary Arterial Switch Operation Beyond the Age of 3 Weeks. Pediatr Cardiol 31, 663–667 (2010). https://doi.org/10.1007/s00246-010-9679-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-010-9679-8