Abstract
Introduction
Cerebellar cortical infarct cavities are a newly recognised entity associated with atherothromboembolic cerebrovascular disease and worse physical functioning. We aimed to investigate the relationship of cerebellar cortical infarct cavities with symptomatic vertebrobasilar ischaemia and with vascular risk factors.
Methods
We evaluated the MR images of 46 patients with a recent vertebrobasilar TIA or stroke and a symptomatic vertebral artery stenosis ≥50 % from the Vertebral Artery Stenting Trial (VAST) for the presence of cerebellar cortical infarct cavities ≤1.5 cm. At inclusion in VAST, data were obtained on age, sex, history of vertebrobasilar TIA or stroke, and vascular risk factors. Adjusted risk ratios were calculated with Poisson regression analyses for the relation between cerebellar cortical infarct cavities and vascular risk factors.
Results
Sixteen out of 46 (35 %) patients showed cerebellar cortical infarct cavities on the initial MRI, and only one of these 16 patients was known with a previous vertebrobasilar TIA or stroke. In patients with symptomatic vertebrobasilar ischaemia, risk factor profiles of patients with cerebellar cortical infarct cavities were not different from patients without these cavities.
Conclusion
Cerebellar cortical infarct cavities are seen on MRI in as much as one third of patients with recently symptomatic vertebral artery stenosis. Since patients usually have no prior history of vertebrobasilar TIA or stroke, cerebellar cortical infarct cavities should be added to the spectrum of common incidental brain infarcts visible on routine MRI.


Similar content being viewed by others
References
Corea F, Hénon H, Milia P, Amici S, Leys D (2000) Silent infarcts and outcome. Cerebrovasc Dis 10(Suppl 4):42–44
Compter A, Kappelle LJ, Algra A, van der Worp HB (2013) Nonfocal symptoms are more frequent in patients with vertebral artery than carotid artery stenosis. Cerebrovasc Dis 35:378–384
Samim M, Hendrikse J, van der Worp HB, Agostoni P, Nijhoff F, Doevendans PA, Stella PR (2015) Silent ischemic brain lesions after transcatheter aortic valve replacement: lesion distribution and predictors. Clin Res Cardiol 104:430–438
Jauch EC, Saver JL, Adams HP et al (2013) Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44:870–947
Wardlaw JM, Smith EE, Biessels GJ et al (2013) Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 12:822–838
Vermeer SE, Prins ND, den Heijer T, Hofman A, Koudstaal PJ, Breteler MM (2003) Silent brain infarcts and the risk of dementia and cognitive decline. N Engl J Med 348:1215–1222
Park K-Y, Chung P-W, Kim YB, Moon HS, Suh BC, Won YS (2009) Association between small deep cerebellar ischemic lesion and small-vessel disease. Cerebrovasc Dis 28:314–320
De Cocker LJ, van Veluw SJ, Fowkes M, Luijten PR, Mali WP, Hendrikse J (2013) Very small cerebellar infarcts: integration of recent insights into a functional topographic classification. Cerebrovasc Dis 36:81–87
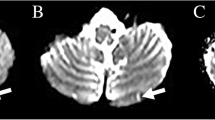
De Cocker LJ, van Veluw SJ, Biessels GJ, Spliet WG, Thunnissen IE, Luijten PR, Hendrikse J, Zwanenburg JJ (2014) Ischaemic cavities in the cerebellum: an ex vivo 7 Tesla MRI study with pathologic correlation. Cerebrovasc Dis 38:17–23
De Cocker LJ, Geerlings MI, Hartkamp NS, Grool AM, Mali WP, Van der Graaf Y, Kloppenborg RP, Hendrikse J (2015) Cerebellar infarct patterns: the SMART-Medea study. NeuroImage Clin 8:314–321
De Reuck JL, Deramecourt V, Auger F et al (2015) The significance of cortical cerebellar microbleeds and microinfarcts in neurodegenerative and cerebrovascular diseases. A post-mortem 7.0-tesla magnetic resonance study with neuropathological correlates. Cerebrovasc Dis 39:138–143
De Cocker LJ, Kloppenborg RP, van der Graaf Y, van der Graaf Y, Luijten PR, Hendrikse J, Geerlings MI (2015) Cerebellar cortical infarct cavities: correlation with risk factors and MRI markers of cerebrovascular disease. Stroke 46:3154–3160
Compter A, van der Worp HB, Schonewille WJ, Vos JA, Algra A, Lo TH, Mali WP, Moll FL, Kappelle LJ (2008) VAST: Vertebral Artery Stenting Trial. Protocol for a randomised safety and feasibility trial. Trials 9:65
Compter A, van der Worp HB, Schonewille WJ, Vos JA, Boiten J, Nederkoorn PJ, Uyttenboogaart M, Lo RT, Algra A, Kappelle LJ (2015) Stenting versus medical treatment in patients with symptomatic vertebral artery stenosis: a randomised open-label phase 2 trial. Lancet Neurol 14:606–614
Hartkamp NS, De Cocker LJ, Helle M, van Osch MJ, Kappelle LJ, Bokkers RP, Hendrikse J (2013) In vivo visualization of the PICA perfusion territory with super-selective pseudo-continuous arterial spin labeling MRI. Neuroimage 83:58–65
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We declare that all human and animal studies have been approved by the ethics committee of the University Medical Center Utrecht in The Netherlands and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that all patients gave informed consent prior to inclusion in this study.
Conflict of interest
JH has received research support from European Research Council (ERC) grant number: ERC-2014-StG – 637024_HEARTOFSTROKE.
Rights and permissions
About this article
Cite this article
De Cocker, L.J.L., Compter, A., Kappelle, L.J. et al. Cerebellar cortical infarct cavities and vertebral artery disease. Neuroradiology 58, 853–857 (2016). https://doi.org/10.1007/s00234-016-1707-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-016-1707-9