Abstract
Introduction
Differentiation between normal solid (non-cystic) pineal glands and pineal pathologies on brain MRI is difficult. The aim of this study was to assess the size of the solid pineal gland in children (0–5 years) and compare the findings with published pineoblastoma cases.
Methods
We retrospectively analyzed the size (width, height, planimetric area) of solid pineal glands in 184 non-retinoblastoma patients (73 female, 111 male) aged 0–5 years on MRI. The effect of age and gender on gland size was evaluated. Linear regression analysis was performed to analyze the relation between size and age. Ninety-nine percent prediction intervals around the mean were added to construct a normal size range per age, with the upper bound of the predictive interval as the parameter of interest as a cutoff for normalcy.
Results
There was no significant interaction of gender and age for all the three pineal gland parameters (width, height, and area). Linear regression analysis gave 99 % upper prediction bounds of 7.9, 4.8, and 25.4 mm2, respectively, for width, height, and area. The slopes (size increase per month) of each parameter were 0.046, 0.023, and 0.202, respectively. Ninety-three percent (95 % CI 66–100 %) of asymptomatic solid pineoblastomas were larger in size than the 99 % upper bound.
Conclusion
This study establishes norms for solid pineal gland size in non-retinoblastoma children aged 0–5 years. Knowledge of the size of the normal pineal gland is helpful for detection of pineal gland abnormalities, particularly pineoblastoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Three to four percent of patients with hereditary retinoblastoma also develop pineoblastoma (trilateral retinoblastoma) [1]. Before the age of 5 years, 95 % of all pineoblastomas are diagnosed [2]. Unfortunately, most patients with pineoblastoma die from this disease [2]. Asymptomatic pineoblastoma patients have shown a much better survival compared to symptomatic pineoblastoma, and the same was seen in small (≤15 mm) versus large (>15 mm) tumors [2]. Asymptomatic patients showed a 5-year survival of 50 %, whereas in patients with symptomatic disease, only 4 % survived [2], emphasizing the importance of early detection. Guidelines advise to perform magnetic resonance imaging in all newly referred retinoblastoma patients and to also include a scan of the entire brain [3].
Unfortunately, however, it is quite challenging to differentiate between a normal pineal gland and pineoblastoma, especially since the best prognosis after pineoblastoma is for patients with small tumors [4–6]. This leaves a small size window in which pineoblastoma should be diagnosed, therefore knowledge about the normal size range at the different ages of the pineal gland is important.
Besides pineoblastomas, knowledge of the normal pineal gland size in children is helpful for detecting abnormal glands and other pineal neoplasms [7]. Actually, small pineal tumors are often difficult to distinguish from normal tissue, due to a similar signal intensity compared to the gland itself and the physiologic enhancement after contrast medium injection due to the lack of a blood brain barrier. On MRI, the gland is usually isointense compared to grey matter on both T1- and T2-weighted images [8, 9]. Pineal gland growth in the first years of life has been documented [10, 11]. Cysts in the pineal gland are a common finding (25–41 % of otherwise normal glands of adolescent and adults at autopsy) [11, 12]; they occur at all ages, from the fetal period to senility [11, 13–18]. Few studies published in literature evaluated the range of the pineal size at different ages. In necropsy-based studies, some authors found a correlation between age and increase of pineal weight, sometimes related to sex, body weight, and different decades [14, 19, 20]; others did not find any correlation [21]. Most of the hitherto performed MRI studies used an inadequately high slice thickness that did not allow for a reliable differentiation of parenchymal and cystic components [10]. Moreover, MRI studies have characterized the pineal gland mainly in adults whereas only sparse information is available for the pediatric pineal gland.
We hypothesize that abnormal growth of the pineal parenchyma has to be considered a far more alerting sign in comparison to presence of cysts or their increase in size. Moreover, correlation of pineal size with age in children is stronger if only the solid part of the gland is measured [10]. Regarding the normal range of the pineal size, only sparse data exist in the literature concerning the in vivo microstructure and volume of the pineal gland in adults and even less is known in children [10, 12]. A recent study showed that there is no difference in pineal gland size of retinoblastoma versus non-retinoblastoma patients allowing for usage of the results from this paper in retinoblastoma patients as well [22].
The first goal of our study was to determine the normal growth pattern of solid pineal glands in a large population, aged 0–5 years. The second goal was to compare pineoblastoma cases from the literature with normal pineal gland sizes. The cystic pineal gland will be analyzed in part II of this study.
Materials and methods
This retrospective study included patients from four European neuroimaging or radiological university centers in Amsterdam, Essen, Lausanne, and Siena. After excluding patients with any known endocrinologic or neurologic disorders (possibly) affecting or related to the pineal gland and distortion of pineal region from adjacent pathologies or artifacts hampering the evaluation of the gland, as well as those patients who were undergoing radiation therapy or chemotherapy, we retrospectively reviewed 184 (Siena n = 39, Essen n = 121, Lausanne n = 17, and Amsterdam n = 7) consecutive non-retinoblastoma patients (73 female, 111 male) in the age range from 0 to 5 years who underwent MR imaging from July 2005 through January 2015 in whom a solid (non-cystic) pineal gland could be clearly identified. In these patients, MRI was performed because of conditions that were not related to the pineal gland; the children were mainly affected by seizures, hydrocephalus, prematurity, development retardation, brain malformations, and neonatal asphyxia.
Imaging
Due to the multicenter setting of this study, the examinations were performed on different 1.5 and 3.0 Tesla MR systems (Magnetom Avanto, Aera, Symphony or Skyra, Siemens Healthcare, Erlangen, Germany) and different T2-weighted sequences were used. We only included MR examinations if the sagittal T2-weighted sequences had a slice thickness of no more than 2 mm to minimize partial volume effects. The slice thickness of the included patients varied between 0.6 and 2 mm.
MR data analysis
The datasets were anonymized prior to analysis. Pineal size was estimated measuring its largest antero-posterior (width) and supero-inferior (height) diameters on the sagittal T2-weighted sequences (as shown in Fig. 1) and by calculating their planimetric area according to the formula: (width / 2) ⨯ (height / 2) ⨯ π. Measurements were performed by four senior neuroradiologists (S.G., P.d.G., P.G., and P.M.) with 12, 12, 17, and 26 years of experience, respectively.
Statistics
We calculated the interobserver agreement (intraclass correlation coefficient [ICC]) for the gland size parameters that were (blinded for the initial measurements) also measured by A.C., M.C.J., and S.S. on a random subset of the included patients (30 patients with a solid gland and 30 patients with a cystic gland). The Kolmogorov-Smirnov test was used to verify the null hypothesis that the variable age of female and male subsamples came from the same continuous distribution. Patients were assigned to one of three 20 months age categories (unlike in part II of this article, we chose not to assign patients to categories of 1 year because there was a very uneven distribution of patients across the age interval: 0–5 years).
The χ 2 independence test was calculated comparing the frequencies of the three categories of age [0, 20), [20, 40), and [40, 60] months in female and male subsamples. Lavene’s test was used to verify the null hypothesis of equal variance (i.e., homoscedasticity) of the pineal measurements across the age intervals by gender. The variable area (square root) and width (natural log) were transformed in order to meet the homoscedasticity assumption. The pineal variables were then subjected to a two-way analysis of variance (ANOVA) test with gender (two levels) and the three age categories [0, 20), [20, 40), and [40, 60] months. Tukey’s honestly significant difference test was performed for the post hoc analysis. Simple linear regression analysis was performed to predict each pineal variable (area, width, and height) based on age.
In addition, 99 % predictive intervals around the mean were used to represent the range where single new observations of pineal parameters would likely fall given specified values of the variable age. Prediction intervals account for the variability around the mean response inherent in any prediction, so they addressed the issue of finding predicted outcomes of area, width, or height based on age.
All statistical calculations were performed using the Statistical Package for the Social Sciences Software Package (SPSS Statistics, version 20; IBM, Armonk, NY, USA) and R (version 3.2.2, 2015, The R Foundation for Statistical Computing).
Comparison with pineoblastoma
To evaluate the clinical usefulness of these age-dependent prediction intervals, we combined the regression line of width (which is usually also the maximum diameter of the gland) with the maximum diameter of pineoblastoma from the meta-analysis by De Jong and colleagues [2] to single graphs. We differentiated between symptomatic and asymptomatic pineoblastoma, and between tumor type: solid, cystic, partially cystic, and unknown; the original articles of eligible pineoblastoma cases included in the meta-analysis were re-evaluated for this. Of most interest in this part will be the asymptomatic solid pineoblastomas, as they resemble the solid pineal glands closest in terms of size and appearance. In part II, a similar comparison will be made.
Results
Both gender-based subsamples showed an asymmetric distribution of age such that the age range [0, 20) months counted up to 67.1 and 52.2 % in female and male, respectively (Fig. 2).
The Kolmogorov-Smirnov test did not reject the null hypothesis that the variable age of female and male subsamples came from the same continuous distribution (p = 0.12). The chi-square test showed no significant interaction between age and gender, hence the age distribution did not relate significantly to gender (p = 0.083).
The width and height measurements showed ICCs of 0.996 (95 % confidence interval [CI] 0.991–0.998) and 0.996 (95 % CI 0.992–0.999), respectively.
Analysis of variance
Lavene’s test showed p values of 0.21, 0.57, and 0.072 respectively for width, height, and area, implying that the group variances were not statistically heterogeneous and the usual ANOVA can be used. The results of ANOVA tests are displayed in Appendix A. The results of the ANOVA tests showed that age significantly predicted the three variables (width, height, and area). Neither gender nor the interaction effect of gender*age were statistically significant. In addition, the post hoc Tukey’s test suggested the presence of a shift in the evolution of the three parameters after the age of 20 months. Specifically, all the three pineal parameters evaluated in the first age interval [0, 20) were significantly lower than in the other age intervals (Appendix B).
Linear regression analysis
Linear regression of area on age significantly predicted area measurements (p < 0.0001; Table 1). Age also explained a significant proportion of the variance in area (adjusted R 2 = 0.26; F test: p < 0.0001). Area (mm2) can be expressed by the equation 8.5 + 0.202 ⨯ age. This finding indicates that the size of area increased by 0.202 mm2 for each month of age starting with a mean area size of 8.5 mm2 at an age of 0 months. Of interest for the normal range of pineal gland size are the upper bounds of the 99 % prediction intervals. Thanks to the relatively large sample size, these 99 % prediction intervals approach linearity and a similar formula can be constructed. For area, the equation of the upper bound is then 25.4 + 0.202 ⨯ age. Similarly, significant regression equations were obtained for the other two relationships width versus age and height versus age, with an adjusted R 2 of 0.25 (F test: p < 0.0001) and 0.20 (F test: p < 0.0001); width and height respectively gave the following formulas: 4.1 + 0.046 ⨯ age and 2.6 + 0.023 ⨯ age (see Table 1 and Fig. 3). For the 99 % upper bounds, 7.9 + 0.046 ⨯ age and 4.8 + 0.023 ⨯ age can be used as the formula respectively for width and height.
In multivariable linear regression analysis of all size parameters, gender was statistically insignificant (p values of 0.96, 0.11, and 0.30 respectively for width, height, and area) and was therefore not considered in further analysis. This result backed up that the progression of the pineal parameters with respect to age was independent of the gender of the patients.
Two out-of-bound points arose in the width versus age regression (Fig. 3a), resulting in a false-positive rate of 1.1 % (2/184). One out-of-bound point was found for the regression of height on age (false-positive rate 0.5 % HSC63227[1/184]; Fig. 3b). One point in the area versus age regression (Fig. 3c) lay beyond the upper bound, which yielded a false-positive rate of 2.2 % (4/184).
Comparison with pineoblastoma
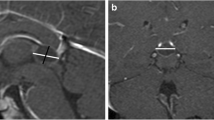
In Fig. 4a, we plotted the linear regression line with 99 % prediction interval of the width (which is similar to the maximum diameter of the gland) of normal solid pineal glands (Table 1) together with the maximum diameter at time of diagnosis of the asymptomatic trilateral retinoblastomas as published in the meta-analysis by De Jong et al. [2] (one circle represents one pineoblastoma case, n = 27; see Fig. 4a). Eighty-nine percent (24 of 27; 95 % CI 71–89 %) of the pineal trilateral retinoblastoma cases, especially of interest, 93 % (13 of 14; 95 % CI 66–100 %) of the solid pineoblastomas, lie beyond the upper bound of normal pineal glands. Most pineoblastomas will not be symptomatic before they reach a certain size; see Fig. 4b where we plotted both the symptomatic (n = 44) and asymptomatic pineoblastomas (n = 27). Figure 4c shows which symptomatic pineoblastomas were solid or (partially) cystic.
Regression line of the normal solid pineal gland width (mm) versus a maximum diameter (mm) of only asymptomatic pineoblastomas, b maximum diameter (mm) of both symptomatic and asymptomatic pineoblastomas, and c maximum diameter (mm) of only symptomatic pineoblastomas. *99 % prediction intervals. †These pineoblastomas are shown in the graph with a size of 10 mm, but had a reported size of 5–15 mm
Discussion
The objective of this study was to provide normative values for solid pineal gland size by gender and age in non-retinoblastoma children from 0 to 5 years and to compare with pineoblastoma tumor size. Linear modeling was used to describe the relationship between solid pineal gland size and age. Age significantly explained the increase in the pineal gland size parameters width, height, and area independent of gender. Even though there were substantially less data points beyond the age of 20 months, the observed sample does support the hypothesis of a linear relationship between age and size (area, width, and height). Presentation of prediction intervals around the estimated mean values is informative about the ranges of the expected normal growth in the pineal gland size. Accordingly, new observations outside the bounds should be considered a warning signal of abnormality. Under this perspective, our study provides clinically useful backing material for interpretation of pineal gland growth in young children. A joint comparison of pineal size to the three prediction intervals of area, width, and height is recommended in order to get rid of ambiguous interpretation of the warning signals and for reducing the false-positive rate.
The pineal gland develops from an embryonic evagination of the third ventricle. In autopsy-based studies, available only in adults, reference values have been reported for pineal weight as well as approximated volumes [19, 21, 23]. Halfway the first decade of life, the structure of the pineal gland approaches that of a mature gland. If the cavum pineale is completely obliterated, the gland is “solid.” If the obliteration is incomplete, one or more cystic cavities remain, which are lined by cells that may differentiate to glial or ependymal cells. Parts of the cysts retain a connection with the ventricular system, which may induce their further enlargement [10, 13].
In 1995, Schmidt et al. were the first to estimate the pineal size by MRI in a large population of children aged 1 day to 15 years [12]. The authors found a mean transaxial diameter of 5.6 mm (SD 2.1), a midsagittal diameter of 5.0 mm (SD 2.4), and a planimetric area of 28.5 mm2 (SD 17.8) that did not change with age, and thus suggested a growth arrest of the pineal gland after infancy.
Sumida et al. [24] retrospectively studied by MRI a large population of patients aged 2 weeks to 20 years. In patients younger than 2 years, the mean size of the pineal gland was as follows: maximum length = 4.8 mm (SD 0.9) and height = 2.9 mm (SD 0.6). In patients aged 2 to 20 years, the gland size was larger and remained stable (average length = 6.1 mm [SD 1.2], average height = 3.7 mm [SD 0.8]). Compared to our study, they examined a smaller sample size of 63 patients in the age range of 0–5 years. The results of Schmidt et al. [12] and Sumida et al. [24] could overestimate the size of the glands because of the inclusion of cystic glands in their series; actually, asymptomatic pineal cyst may exert an important influence on pineal size. A serial MRI study performed by Barboriak et al. [16] in a small series over a period of 6 months to 9 years confirmed that pineal cysts remain unchanged on the whole and that cysts can either form or involute in individual patients. For more information about the cystic pineal gland, please see part II.
Recently, Bumb et al. [10] evaluated the correlation between pineal gland volume and age in 54 patients aged 0–17 years (median 2.0) with true-fast imaging with steady-state precession (FISP) sequences; in the presence of cysts, pineal parenchymal volume was defined as pineal gland volume minus cyst volume. The authors showed that the solid pineal parenchymal volume correlated more strongly with age than did the cystic pineal parenchymal volume [10]. The data of the study by Bumb et al. showed an increase of pineal volume with age, which was especially strong if only solid parenchyma is included (Pearson’s correlation coefficient r = 0.66); actually, the solid pineal parenchymal volume showed a mean of 3.9 mm3 (SD 2.8) at less than 1 year, 20.4 mm3 (SD 17.2) at 1–2 years, 21.0 mm3 (SD 16.7) at 2–4 years, and 40.0 mm3 (SD 24.1) at 5–11 years.
Bumb et al. suggested a possible bias in measuring pineal glands when including glands with a cystic component. Even though Bumb et al. [10] used a very reliable 3D evaluation method, in our study (based on T2-weighted sagittal 2D images with a slice thickness of ≤2 mm) we looked at a narrower age interval of the subject population, which only included the ages from 0 to 5 years. This, together with our far higher number of patients (184 versus about 30), allowed for a higher statistical significance of pineal gland size in that age range.
Compared with pineal trilateral retinoblastoma
Normal gland sizes might also be used outside the context of retinoblastoma, but for retinoblastoma patients, knowledge of the normal gland could help with early detection of pineal trilateral retinoblastoma. In this situation, especially the solid (non-cystic) asymptomatic trilateral retinoblastomas—since patients with asymptomatic disease showed much better survival after pineoblastoma than did patients with symptoms [2]—are of interest as we restricted this study to the size of the normal solid pineal gland. Most asymptomatic solid pineoblastomas were above the upper bound normal pineal gland width, suggesting that the results of this study could indeed be useful to differentiate normal from abnormal solid pineal glands. We compared the maximum diameter (in any direction) of pineoblastoma with the upper 99 % prediction bound of the width of a normal gland, which is actually a conservative measurement in some cases, as some of the measurements of pineoblastoma actually might better be compared to the height of the lesion and should therefore be compared to the upper 99 % prediction bound of the gland height.
Limitations
We have to address some limitations of our study. First of all, owing to the technical parameters chosen in our study, we only obtained the area of the glands, and true three-dimensional volumes of the glands could not be assessed. We assumed measurements from the transversal plane not to be statistically different with those from the sagittal plane, based on the measurements performed in a previous study in a series of 277 pineal glands [12]. Moreover, true-FISP sequences used by Bumb et al. [10] are not available in all MR units, so we used the universally available T2-weighted TSE sequence with a slice thickness 0.75–2 mm to measure the size of the pineal glands. This allowed for obtaining reliable measurements and the same certainty regarding pineal cysts (lower limit of diameter 2 mm) as was shown in the FISP sequences.
Second, small sample sizes may result in a potential large error in the estimates, causing wider prediction intervals than the estimated extent of individual variation, because it is affected by the uncertainty of sample estimates of mean and variance [20].
This study provides upper bounds for the sizes of normal pineal glands of patients aged 0–5 years, helping radiologists to decide whether they are within or outside the range of a clinical population. Of course, this does imply that a pineoblastoma will not be detectable based on pineal gland size until it has reached a certain size. Knowledge of the size of the normal pineal gland is helpful for detection of pineal gland abnormalities, particularly pineoblastoma.
References
de Jong MC, Kors WA, de Graaf P et al (2015) The incidence of trilateral retinoblastoma: a systematic review and meta-analysis. Am J Ophthalmol 160:1116–1126.e5
de Jong MC, Kors WA, de Graaf P et al (2014) Trilateral retinoblastoma: a systematic review and meta-analysis. Lancet Oncol 15:1157–67
de Graaf P, Göricke S, Rodjan F et al (2012) Guidelines for imaging retinoblastoma: imaging principles and MRI standardization. Pediatr Radiol 42:2–14
Popovic MB, Balmer A, Maeder P et al (2006) Benign pineal cysts in children with bilateral retinoblastoma: a new variant of trilateral retinoblastoma? Pediatr Blood Cancer 46:755–61
Rodjan F, de Graaf P, Moll AC et al (2010) Brain abnormalities on MR imaging in patients with retinoblastoma. AJNR Am J Neuroradiol 31:1385–9
Rodjan F, de Graaf P, Brisse HJ et al (2012) Trilateral retinoblastoma: neuroimaging characteristics and value of routine brain screening on admission. J Neurooncol 109:535–44
Sun B, Wang D, Tang Y et al (2009) The pineal volume: a three-dimensional volumetric study in healthy young adults using 3.0 T MR data. Int J Dev Neurosci 27:655–60
Tien RD, Barkovich AJ, Edwards MS (1990) MR imaging of pineal tumors. AJR Am J Roentgenol 155:143–51
Zee CS, Segall H, Apuzzo M et al (1991) MR imaging of pineal region neoplasms. J Comput Assist Tomogr 15:56–63
Bumb JM, Brockmann MA, Groden C et al (2012) TrueFISP of the pediatric pineal gland: volumetric and microstructural analysis. Clin Neuroradiol 22:69–77
Mandera M, Marcol W, Bierzynska-Macyszyn G, Kluczewska E (2003) Pineal cysts in childhood. Childs Nerv Syst 19:750–755
Schmidt F, Penka B, Trauner M et al (1995) Lack of pineal growth during childhood. J Clin Endocrinol Metab 80:1221–5
Carr J (1944) Cystic hydrops of the pineal gland. J Nerv Dis 99:552–72
Tapp E, Huxley M (1972) The histological appearance of the human pineal gland from puberty to old age. J Pathol 108:137–144
Al-Holou WN, Garton HJL, Muraszko KM et al (2009) Prevalence of pineal cysts in children and young adults. Clinical article. J Neurosurg Pediatr 4:230–6
Barboriak DP, Lee L, Provenzale JM (2001) Serial MR imaging of pineal cysts: implications for natural history and follow-up. AJR Am J Roentgenol 176:737–43
Tamaki N, Shirataki K, Lin TK et al (1989) Cysts of the pineal gland. A new clinical entity to be distinguished from tumors of the pineal region. Childs Nerv Syst 5:172–6
Golzarian J, Balériaux D, Bank WO et al (1993) Pineal cyst: normal or pathological? Neuroradiology 35:251–3
Rodin AE, Overall J (1967) Statistical relationships of weight of the human pineal to age and malignancy. Cancer 20:1203–14
Jolicoeur P (2012) Introduction to Biometry. Springer, New York, pp 61–62
Hasegawa A, Ohtsubo K, Mori W (1987) Pineal gland in old age; quantitative and qualitative morphological study of 168 human autopsy cases. Brain Res 409:343–9
Pham TTH, Siebert E, Asbach P et al (2015) Magnetic resonance imaging based morphologic evaluation of the pineal gland for suspected pineoblastoma in retinoblastoma patients and age-matched controls. J Neurol Sci. doi:10.1016/j.jns.2015.10.046
Tapp E, Huxley M (1971) The weight and degree of calcification of the pineal gland. J Pathol 105:31–9
Sumida M, Barkovich AJ, Newton TH (1996) Development of the pineal gland: measurement with MR. AJNR Am J Neuroradiol 17:233–6
Acknowledgments
MCdJ is financially supported by a grant from the ODAS Foundation, Delft, The Netherlands. The European Retinoblastoma Imaging Collaboration (ERIC) is financially supported by a grant from the ODAS Foundation, Delft, The Netherlands. The authors’ work was independent of the funding organizations, none of whom had involvement in the design or conduct of this study, data management and analysis, manuscript preparation, and review or authorization for submission.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
We declare that all human and animal studies have been approved by the ethics committee of the VU University Medical Center, Amsterdam, and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that the ethics committee waived informed patient consent.
Conflict of interest
We declare that we have no conflict of interest.
Additional information
PG and MCdJ are joint first authors.
The European Retinoblastoma Imaging Collaboration
Prof. Jonas A. Castelijns, MD, PhD, Pim de Graaf, MD, PhD, and Marcus C. de Jong, MD, MSc (Department of Radiology and Nuclear Medicine, VU University Medical Center, Amsterdam, the Netherlands), Hervé J. Brisse, MD, PhD (Department of Radiology, Institut Curie, Paris, France), Paolo Galluzzi, MD (Unit of Diagnostic and Therapeutic Neuroradiology, Department of Neurosciences, Siena University Hospital, Siena, Italy), Sophia Göricke, MD, Selma Sirin, MD (Institute of Diagnostic and Interventional Radiology and Neuroradiology, University Hospital Essen, Germany), and Philippe Maeder, MD (Department of Radiology, Centre Hospitalier Universitaire Vaudois (CHUV), and University of Lausanne, Lausanne, Switzerland).
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 103 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Galluzzi, P., de Jong, M.C., Sirin, S. et al. MRI-based assessment of the pineal gland in a large population of children aged 0–5 years and comparison with pineoblastoma: part I, the solid gland. Neuroradiology 58, 705–712 (2016). https://doi.org/10.1007/s00234-016-1684-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-016-1684-z