Abstract
Introduction
We evaluated the normal venous anatomy of the anterior medullary/anterior pontomesencephalic venous (AMV/APMV) system and bridging veins connected to the dural sinuses using magnetic resonance (MR) imaging and demonstrated cases of dural arteriovenous fistulas (DAVFs) with bridging venous drainage.
Materials and methods
MR images obtained using a 3D gradient echo sequence in 70 patients without lesions affecting the deep or posterior venous channels were reviewed to evaluate the normal anatomy of the AMV/APMV system and bridging veins. MR images and digital subtraction angiography in 80 cases with intracranial or craniocervical junction DAVFs were reviewed to evaluate the bridging venous drainage from DAVFs.
Results
MR images clearly revealed AMV/APMV in 35 cases. Fifteen cases showed a direct connection between AMV and APMV, while 15 cases showed an indirect communication via the transverse pontine vein or the bridging vein. In the five remaining cases, the AMV and APMV end separately to the bridging vein or the transverse pontine vein. Bridging veins were identified in 34 cases, connecting to the cavernous sinus in 33, to the suboccipital cavernous sinus in 11, and the inferior petrosal sinus in five cases. In 80 DAVF cases, seven of 40 cavernous sinus DAVFs, two craniocervical junction DAVFs, and one inferior petrosal sinus DAVF drained via bridging veins to the brain stem.
Conclusion
The AMV/APMV and bridging veins showed various anatomies and frequently showed a connection to the cavernous sinus. Knowledge of the venous anatomy is helpful for the diagnosis and intravascular treatment of DAVFs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The anterior pontomesencephalic–anterior medullary venous (APM–AMV) system is an important venous channel that drains blood from the brain stem and cerebellum. The anterior pontomesencephalic vein (APMV) is connected to the basal vein via the peduncular vein, superiorly, which runs longitudinally in the peduncular fossa or along the anterior surface of the cerebral peduncle, and is often continuous with the AMV, inferiorly [1]. The AMV usually runs in the midline along the anterior surfaces of the pons and medulla, which connect to the anterior spinal vein, inferiorly (Fig. 1). This longitudinal venous channel communicates with the adjacent dural sinuses via the transverse pontine vein and/or bridging veins [2]. Therefore, dural arteriovenous fistulas (DAVFs) can drain through bridging veins into the APM–AMV system and may cause serious symptoms such as pontine hemorrhage and venous edema [3–6]. However, little attention has been paid to the venous anatomy of the bridging veins and the APM–AMV system. In this study, we evaluated the venous anatomy of the APM–AMV system and its bridging veins that communicate with the APM–AMV system and the dural sinuses using magnetic resonance imaging (MRI). Cases of dural AVF draining via the venous system were also reviewed and demonstrated.
Schematic diagram of the APM–AMV system. The APMV connects to the peduncular vein superiorly, which runs longitudinally in the peduncular fossa and is continuous with the transverse pontine vein and the AMV inferiorly at the mid-pons level. The AMV usually runs in the midline along the anterior surface of the pons and medulla, which connects to the anterior spinal vein inferiorly. The transverse pontine vein connects to the petrosal vein laterally
Materials and methods
We retrospectively evaluated MRI from consecutive patients examined using fat-suppressed contrast-enhanced 3D fast gradient-echo MRI between March 2004 and April 2006. Among them, patients with pathological conditions potentially affecting the APM–AMV system such as cerebellopontine angle tumors were excluded from the study, leaving 70 participating patients (25 men and 45 women; age range, 26–83 years; mean age, 57.6 years). The fat-suppressed contrast-enhanced 3D fast gradient-echo images using the 1.5 T MR unit (Excelart Vantage, Toshiba Medical Systems, Tokyo, Japan) were evaluated. The imaging parameters were as follows: repetition time/echo time, 25:5.5; flip angle, 20°; matrix size, 224 × 256; section, 1 mm. The scanning area covered between the level of the orbital roof and the craniocervical junction. Postcontrast images after the intravenous injection of 0.1 mmol/kg gadolinium chelate (Omniscan) were obtained for each patient.
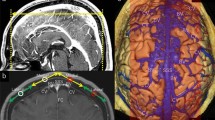
The images were transferred to a workstation, and the transverse images were evaluated by consensus between two neuroradiologists (H.K. and Y.S.) for the normal anatomies of the APM–AMV system and its bridging veins. The vertical continuity of such veins was evaluated by paging the transverse images on the same window (Fig. 2).
Normal MRI of the APM–AMV system. The anterior spinal vein runs along the anterior surface of the cord and receives the bridging vein [arrowhead in (a)] from the suboccipital cavernous sinus at the craniocervical junction level. The AMV also runs in the midline on the anterior surface of the medulla and pons (type 1) and then joins with the APMV via the transverse pontine vein (type B). The APMV continues to the peduncular vein superiorly. Note the bridging vein to the cavernous sinus [arrowheads in (e)]. Arrows indicate AMV/APMV
We retrospectively reviewed 80 cases of dural AVFs that performed digital subtraction angiography (DSA) in our institution between January 2000 and March 2007 and evaluated DSA and MRI with regard to the draining route via the APM–AMV system. The locations of dural AVFs were in the cavernous sinus in 40, transverse sigmoid sinus in 17, tentorial in seven, condylar canals in five, craniocervical junction in seven, anterior fossa in two, and others in seven cases.
Results
Normal venous anatomy
Among 70 patients, the APM–AMV system was entirely evaluated in 35 patients. In the other patients, the APMV and/or AMV could not be identified or was scantly visible when evaluating longitudinal continuity. In 35 patients, we observed several variations of the APM–AMV system at two levels of the pontomedullary junction and the mid-pons.
Pontomedullary junction level
The patterns of the AMV at the pontomedullary junction were classified into six types (Fig. 3). These were type 1, single AMV running superiorly in the midline along the anterior surface of the pons; type 2, single AMV running superior laterally; type 3, double AMVs with one running in the midline and the other running superior laterally; type 4, double AMVs both running superior laterally; type 5, triple AMV; and type 6, absent AMV superiorly beyond the pontomedullary junction. Fifteen patients (43%) were considered as type 1, five (14%) were type 2, six (17%) were type 3, four (11%) were type 4, two (6%) were type 5, and three (8%) were type 6.
Various types of the anterior medullary vein at the pontomedullary junction level. Type 1 single AMV running superiorly in the midline along the anterior surface of the pons. Type 2 single AMV running superior laterally. Type 3 double AMVs, one running in the midline and the other running superior laterally. Type 4 double AMVs, both running superior laterally. Type 5 triple AMVs. Type 6 absent AMV beyond the pontomedullary junction, superiorly
Mid-pons level
The patterns of the APMV and the AMV at the mid-pons level were classified into three types (Fig. 4): type A, the AMV directly continues to the APMV; type B, the AMV communicates with the APMV via the transverse pontine vein in which there are two subtypes of unilateral communication and bilateral communication; type C, the AMV is interrupted at the APMV, at the mid-pons level. In type C, the AMV and APMV end to the cavernous sinus, separately through the bridging veins and/or the transverse pontine vein (Fig. 5) or to the petrosal vein. There were 15 patients (43%) of type A, 15 (43%) of type B, and five (14%) of type C. In the type B group, there were nine cases of unilateral communication and six cases of bilateral communication.
Variations of the APMV and the AMV at the mid-pons level. Type A the AMV directly continues to the APMV. Type B the AMV communicates with the APMV via the transverse pontine vein in which there are two subtypes of communication (unilateral communication: B1 and bilateral communication: B2). Type C the AMV interrupts the APMV at the mid-pons level. The AMV and APMV end at the cavernous sinus separately through the bridging veins
MRI of the type 1 and type C APM–AMV system. The AMV (arrows) runs along the anterior surface of the medulla and pons (type 1), then runs superolaterally at the mid-pons level and ends at the left cavernous sinus via the bridging vein (type C). The APMV (arrowheads) also ends at the left cavernous sinus via a different bridging vein
Bridging veins
Bridging veins were identified in 34 of 35 patients (97%). The bridging veins communicated with the APMV–AMV and cavernous sinus, inferior petrosal sinus, suboccipital cavernous sinus, marginal sinus, and jugular bulb (Fig. 6). Bridging veins communicating with the APMV–AMV (via the transverse pontine vein) to the posterior aspect of the cavernous sinus were observed in 33 patients (94%) in which bilateral bridging veins to both cavernous sinuses were seen in 15 patients. Bridging veins to the suboccipital cavernous sinus were observed in 11 patients (31%). Five patients (14%) showed that the veins were bridged to the inferior petrosal sinus while three patients showed bridging to the marginal sinus, and bridging to the jugular bulb was seen in one patient.
Dural arteriovenous fistulas
Among the 81 cases of intracranial or craniocervical junction dural AVFs, bridging venous drainage to the APM–AMV system was found in ten cases. The locations of dural AVFs in the ten cases were in the cavernous sinus in seven, at the craniocervical junction in two, and at the inferior petrosal sinus in one case (Figs. 7, 8, 9 and 10). Two cases of dural AVFs were located on one craniocervical junction and one inferior petrosal sinus showing symptoms due to edema of brainstem or spinal cord (Fig. 8). In one case of cavernous dural AVF, transient worsening of symptoms occurred after incomplete transvenous embolization with residual bridging venous drainage due to brainstem edema (Fig. 9).
Craniocervical junction DAVF draining via bridging vein and AMV/APMV system (type 1 and type C). A 70-year-old woman with a dural AVF located at the craniocervical junction. The AVF was incidentally found on angiography when evaluating for a cerebral aneurysm at the left internal carotid artery (not shown). Bilateral vertebral angiography (a–d) showed that the AVF drained via the anterior medullary vein, and the bridging vein into the right cavernous sinus. MRI (e–i) show that the dural AVF draining into the anterior medullary vein continuing superiorly in the midline along the anterior surface of the medulla and pons. The AMV (arrows) runs right laterally at the mid-pons level and joins the right cavernous sinus via the bridging vein (arrowheads). Because the AVF showed no symptoms, and MRI showed no brainstem edema; the AVF was treated by stereotactic radiosurgery
Craniocervical junction DAVF draining via bridging vein and AMV (type 6). A 77-year-old man with symptoms of spinal cord edema. Angiography showed that the AVF was located at the cervicocranial junction and was fed by the meningeal branches from the left occipital artery and the left vertebral artery. Selective angiography (a) via microcatheter positioned at a branch of the right occipital artery shows that the AVF drains into the AMV and backward inferiorly to the spinal vein, probably due to hypoplasty of the AMV at the pontomedullary junction (arrow; type 6). CT (b) after embolization with glue shows glue cast (white arrow) in the fistulous point at the right suboccipital cavernous sinus
Cavernous sinus DAVF with bridging venous drainage. A 42-year-old woman with ocular symptoms. Bilateral carotid angiography showed a dural AVF at the cavernous sinus, which drained into the superior orbital vein, the superficial middle cerebral vein, and the basal vein via the bridging venous system (a, b). Transvenous embolization was performed, but unfortunately, the procedure was interrupted because the catheter was accidentally pulled back to the inferior petrosal sinus and never advanced into the CS. The final angiogram showed occlusion of most of the AVF, but the residual AVF drained via the bridging vein into the transverse pontine vein (arrows) and to the APMV (c, d). Transient worsening of the symptoms due to pontine edema that developed after embolization
Cavernous sinus DAVF with bridging venous drainage A 48-year-old woman with ocular symptoms. Bilateral internal and external carotid angiograms showing a dural AVF at the left cavernous sinus, which drained into the superior orbital vein, the superficial middle cerebral vein, and the basal vein (a). Three-dimensional DSA image (b) well demonstrated the AVF draining via the bridging vein (white arrowheads) into the APMV and the AMV (white arrows). Selective venogram (c) via a microcatheter positioned at the outlet to the bridging vein clearly demonstrate the bridging venous drainage to the APMV (arrows). With special attention to the bridging venous drainage, the AVF was completely occluded without any complications (d)
Discussion
The APMV and the AMV are the longitudinal venous channels that run along the anterior surface of the brain stem. The APM–AMV runs more closely to the brain stem than the basilar artery; thus, the APM–AMV can exactly define the anterior outline of the brainstem on lateral view of angiography [7, 8]. This information has been used in diagnostic neuroradiology. However, the recent advances in technology of less invasive modalities including MRI and multidetector-low computed tomography (CT) can directly depict the brain stem and lesions. Only little attention has been paid to the APM–AMV system in diagnostic neuroradiology.
During the fourth stage of embryonic development, numerous primary transverse (pial-arachnoid) veins first become identified on the surface of the neural tube, which connect to the dural plexus. Between these primary transverse veins, secondary longitudinal anastomoses soon develop parallel to the basilar artery. Then, most of the primary transverse veins are reduced according to the enlargement of the brain. In this way, the venous net and the main pial veins of the medulla and pons are formed [9]. Therefore, several variations of the APMV–AMV system can occur depending on the degree of the regression and the development of the primary transverse and secondary longitudinal veins.
In our results, there were several variations in the course of the APM–AMV system. The variations of the AMV were frequently found at the pontomedullary junction level. The AMV communicates with the vein of the pontomedullary sulcus at the pontomedullary sulcus and is contiguous to the median anterior medullary vein (type 1), one or two anterior lateral (ponto)medullary veins (type 2 or 4), both the median and lateral anterior (ponto)medullary vein (type 3 or 5), or is discontinued superiorly (type 6).
At the mid-pons level, the AMV often communicates with the APMV directly (type A) or indirectly via the transverse pontine vein (type B). However, there was no communication between the APMV and AMV in 14% of cases (type C). In the type C group, the bridging vein to the cavernous sinus would play an important role for brain stem venous drainage.
To the best of our knowledge, only one anatomical study has been reported in the English literature on the bridging veins connecting the brain stem venous system with the adjacent dural sinus. Matsushima et al. [2] mentioned that there were several bridging veins connecting the APM–AMV system to the adjacent dural sinuses, in an excellent anatomical study. They reported that the bridging veins run from the APMV or transverse pontine vein to the posterior portion of the cavernous sinus just below the Meckel’s cave; from the vein of the pontomedullary sulcus or anterior, lateral, and transverse medullary veins to the inferior petrous sinus, the sigmoid sinus, the marginal sinus, or the anterior condylar vein. According to their results, in 25 adult cadavers, bridging veins to the cavernous sinus were identified in 12.5%, to the inferior petrosal sinus in 8.3%, to the sigmoid sinus in 37.5%, and to the marginal sinus around the foramen in 41.7%. In our study, bridging veins to the cavernous sinus were more frequently observed in 94% of patients (of 35 cases). Although we cannot clearly explain why we obtained such a difference in the frequency of visibility of the bridging veins, we hypothesize that the differences may be the results of different methodologies between a cadaver-based anatomical study and a clinical MR evaluation.
For the cases of dural AVFs potentially draining via the APM–AMV system, the development of the APM–AMV system and its bridging veins would be related to the symptoms. In our series, both cases of dural AVFs at the craniocervical junction drained via the AMV superiorly. One case without symptoms showed the AMV directly connected to the APMV (type 1), and the AVF drained into the cavernous sinus via the developed bridging vein without venous stasis. In contrast, another case with spinal cord edema showed that the AMV was interrupted at the pontomedullary junction (type 6) and the AVF drained via the vein of the pontomedullary sulcus and backward into the spinal veins. Kai et al. [10] reported six cases of AVF at the cervicomedullary junction including four cases of dural AVFs. All four cases of dural AVFs presented with subsrachnoid hemorrhage, and the AVFs drained ascending into the cavernous sinus, the superior petrosal sinus, or the inferior petrosal sinus. Several cases of intracranial dural AVFs draining into the APM–AMV system have been reported, and the majority of the reported cases showed brain stem injury due to venous congestion and/or hemorrhage [3–6]. Two potential drainage routes to the APM–AMV system of the petrosal venous route and the bridging venous routes exist. The petrosal venous route is commonly seen in dural AVFs at the superior petrosal sinus, tentorium, and rarely in cavernous dural AVFs. The AVF drains via the petrosal vein contiguous with the transverse pontine vein into the AMV–APMV system [5]. To the best of our knowledge, only one case has been reported for the bridging venous drainage in the English literature [6]. Although we found some additional cases of angiography suggesting bridging venous drainage to the APM–AMV in previously published papers, none showed specific descriptions of the drainage route to the brain stem [4, 5, 11]. In our review of cases of cavernous dural AVFs, we demonstrated a high incidence of cases of bridging venous drainage into the APM–AMV system (seven of 40 cases). Our result of a high incidence of bridging veins connecting the APMV–AMV system and the cavernous sinus using normal MRI supports the idea that the cavernous dural AVF can frequently drain via bridging veins. Because of the very small size of the bridging veins and the overlap from other vessels, the veins may be often misidentified by conventional DSA without special attention to particular veins. Although the cavernous dural AVF is generally thought to be a benign type of intracranial dural AVF, the AVF with bridging venous drainage into the brainstem can cause fatal symptoms. Furthermore, inadequate embolization for such cases can lead to serious complications such as brain stem edema due to venous congestion (Fig. 9). Kim et al. [11] demonstrated the transvenous embolization of cavernous dural AVFs in 57 patients. In their study series, venous congestion of the posterior fossa after transvenous embolization developed in two patients. One patient showed permanent deficits, and the other improved after additional treatments. Angiography after embolization in one patient showed remarkable residual shunt draining into the APMV suggesting bridging venous drainage. Therefore, it is very important for the treatment of cavernous dural AVFs to assess deep venous drainage including bridging venous drainage before and during transvenous embolization.
Our study has several limitations. Spatial resolution of MRI was limited in evaluating the normal venous anatomy of the APM–AMV system. Although we evaluated 70 cases, the APM–AMV system could have been entirely evaluated in only 35 cases. It is possible that the APM–AMV system was too small to be identified on MRI in some cases. Some variations of the venous system, which could not be evaluated by MRI, may be presented. Our work may scratch only the surface of the great variability of the normal venous anatomy of the AMV/APMV system and its bridging veins. However, we believe that the knowledge of the venous anatomy would be helpful for the diagnosis and interventional treatment of dural AVFs.
References
Lasjaunias P, Berenstein A, Ter Brugge KG (2001) Surgical Neuroangiography 1. Clinical Vascular Anatomy and Variations, 2nd edn. Springer-Verlag, Berlin Heidelberg New York, pp 680–682
Matsushima T, Rhoton AL, Oliveira F, Peace D (1983) Microsurgical anatomy of the vein of the posterior fossa. J Neurosurg 59:63–105
Iwasaki M, Murakami K, Tomita T, Numagami Y, Nishijima M (2006) Cavernous sinus dural arteriovenous fistula complicated by pontine venous congestion. A case report. Surg Neurol 65:516–519 doi:10.1016/j.surneu.2005.06.044
Ricolfi F, Manelfe C, Meder JF et al (1999) Intracranial dural arteriovenous fistulae with perimedullary venous drainage. Anatomical, clinical and therapeutic considerations. Neuroradiology 41:803–812 doi:10.1007/s002340050846
Takahashi S, Tomura N, Watarai J, Mizoi K, Manabe H (1999) Dural arteriovenous fistula of the cavernous sinus with venous congestion of the brain stem: report of two cases. AJNR Am J Neuroradiol 20:886–888
Takahashi S, Kato K, Tomura N, Watarai J, Mizoi K (2001) Dural arteriovenous fistula of the cavernous sinus with cortical venous reflux of the posterior fossa via a bridging vein. Radiat Med 19:219–222
Bradac GB (1970) The ponto-mesencephalic veins: radio-anatomical study. Neuroradiology 1:52–57 doi:10.1007/BF00347661
Peeters FLM (1973) The vertebral angiogram in patients with tumors in or near the midline. Neuroradiology 5:53–58 doi:10.1007/BF02464632
Padget DH (1957) The development of the cranial venous system in man, from the view point of comparative anatomy. Contr Embryol 36:79–140
Kai Y, Hamada J, Morioka M, Yano S, Mizuno T, Kuratsu J (2005) Arteriovenous fistulas at the cervicomedullary junction presenting with subarachnoid hemorrhage: six case reports with special reference to the angiographic pattern of venous drainage. AJNR Am J Neuroradiol 26:1949–1954
Kim DJ, Kim DI, Suh SH et al (2006) Results of transvenous embolization of cavernous dural arteriovenous fistula: a single-center experience with emphasis on complications and management. AJNR Am J Neuroradiol 27:2078–2082
Conflict of interest statement
We declare that we have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Kiyosue, H., Tanoue, S., Sagara, Y. et al. The anterior medullary–anterior pontomesencephalic venous system and its bridging veins communicating to the dural sinuses: normal anatomy and drainage routes from dural arteriovenous fistulas. Neuroradiology 50, 1013–1023 (2008). https://doi.org/10.1007/s00234-008-0433-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-008-0433-3