Abstract
Introduction
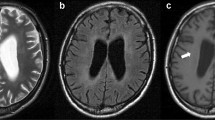
It is not always possible to differentiate infective from neoplastic brain lesions with conventional MR imaging. In this study, we assessed the utility of various perfusion indices in the differentiation of infective from neoplastic brain lesions.
Methods
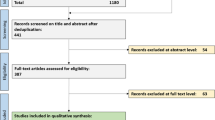
A total of 103 patients with infective brain lesions (group I, n=26) and neoplastic brain lesions (high-grade glioma, HGG, group II, n=52; low-grade glioma, LGG, group III, n=25) underwent dynamic contrast-enhanced MR imaging. The perfusion indices, including relative cerebral blood volume (rCBV), relative cerebral blood flow (rCBF), transfer coefficient (ktrans) and leakage (ve), were calculated and their degree of correlation with immunohistologically obtained microvessel density (MVD) and vascular endothelial growth factor (VEGF) determined. The rCBV was corrected for the leakage effect. Discriminant analysis for rCBV, rCBF, ktrans and ve was performed to predict the group membership of each case and post hoc analysis was performed to look for group differences.
Results
The rCBV, rCBF, ktrans, ve, MVD and VEGF were significantly different (P<0.001) between the three groups. Discriminant analysis showed that rCBV predicted 73.1% of the infective lesions, 84.6% of the HGG and 72.0% of the LGG. The rCBF classified 86.5% of the HGG, 80.0% of the LGG and 65.4% of the infective lesions. The ktrans discriminated 98.1% of the HGG, 76.0% of the LGG and 88.5% of the infective lesions correctly. The ve classified 98.1% of the HGG, 76.0% of the LGG and 84.6% the infective lesions. The rCBV was correlated significantly with MVD and VEGF, while the correlation between ktrans and MVD was not significant.
Conclusion
Physiological perfusion indices such as ktrans and ve appear to be useful in differentiating infective from neoplastic brain lesions. Adding these indices to the current imaging protocol is likely to improve tissue characterization of these focal brain mass lesions.







Similar content being viewed by others
References
Gupta RK, Kathuria M, Pradhan S (1999) Magnetization transfer MR imaging in CNS tuberculosis. AJNR Am J Neuroradiol 20:867–875
Gupta RK, Husain M, Vatsal DK, Kumar R, Chawla S, Husain N (2002) Comparative evaluation of magnetization transfer MR imaging and in-vivo proton MR spectroscopy in brain tuberculomas. Magn Reson Imaging 20:375–381
Mishra AM, Gupta RK, Jaggi RS, Reddy JS, Jha DK, Husain N, Prasad KN, Behari S, Husain M (2004) Role of diffusion-weighted imaging and in vivo proton MR spectroscopy in the differential diagnosis of ring enhancing intracranial cystic mass lesions. J Comput Assist Tomogr 28:540–547
Garg M, Gupta RK, Husain M, Chawla S, Chawla J, Kumar R, Rao SB, Misra MK, Prasad KN (2004) Brain abscesses: etiologic categorization with in vivo proton MR spectroscopy. Radiology 230:519–527
Holmes TM, Petrella JR, Provenzale JM (2004) Distinction between cerebral abscesses and high-grade neoplasms by dynamic susceptibility contrast perfusion MRI. AJNR Am J Neuroradiol 183:1247–1252
Chan JH, Tsui EY, Chau LF, Chow KY, Chan MS, Yuen MK, Chan TL, Cheng WK, Wong KP (2002) Discrimination of an infected brain tumor by cerebral brain abscess by combined MR perfusion and diffusion imaging. Comput Med Imaging Graph 26:19–23
Batra A, Tripathi RP (2003) Perfusion magnetic resonance imaging in intracerebral parenchymal tuberculosis: preliminary findings. J Comput Assist Tomogr 27:882–888
Folkman J (2002) Role of angiogenesis in tumor growth and metastasis. Semin Oncol 29:15–18
Carmeliet P, Jain RK (2000) Angiogenesis in cancer and other diseases. Nature 407:249–257
Machein MR, Kullmer J, Fiebich BL, Plate KH, Wamke PC (1999) Vascular endothelial growth factor expression, vascular volume, and capillary permeability in human brain tumors. Neurosurgery 44:732–741
van der Flier M, Hoppenreijs S, van Rensburg AJ, Ruyken M, Kolk AH, Springer P, Hoepelman AI, Kimpen JL, Schoeman JF (2004) Vascular endothelial growth factor and blood brain barrier disruption in tuberculous meningitis. Pediatr Infect Dis J 23:608–613
Abe Y, Sugisaki K, Dannenberg AM Jr (1996) Rabbit vascular endothelial adhesion molecules: ELAM-1 is most elevated in acute inflammation, whereas VCAM-1 and ICAM-1 predominate in chronic inflammation. J Leukoc Biol 60:692–703
Kielian T, Hickey WF (2000) Proinflammatory cytokine, chemokine, and cellular adhesion molecule expression during the acute phase of experimental brain abscess development. Am J Pathol 157:647–658
Baldwin AC, Kielian T (2004) Persistent immune activation associated with a mouse model of Staphylococcus aureus-induced experimental brain abscess. J Neuroimmunol 151:24–32
Jackson A (2003) Imaging microvasculature structure with contrast enhanced MRI. Br J Radiol 76:159–173
Cha S, Lu S, Johnson G, Knopp EA (2000) Dynamic susceptibility contrast MR imaging: correlation of signal intensity changes with cerebral blood volume measurements. J Magn Reson Imaging 11:114–119
Aronen HJ, Glass J, Pardo FS, Belliveau JW, Gruber ML, Buchbinder BR, Gazit IE, Linggood RM, Fischman AJ, Rosen BR (1995) Echo-planar MR cerebral blood volume mapping of gliomas: clinical utility. Acta Radiol 36:520–528
Aronen HJ, Perkio J (2002) Dynamic susceptibility contrast MRI of gliomas. Neuroimaging Clin N Am 12:501–523
Jackson A (2004) Analysis of dynamic contrast enhanced MRI. Br J Radiol 77:154–166
Singh A, Haris M, Rathore D, Purwar A, Sarma MK, Bayu G, Husain N, Rathore RK, Gupta RK (2007) Quantification of physiological and hemodynamic indices using T1 dynamic contrast-enhanced MRI in intracranial mass lesions. J Magn Reson Imaging 26:871–880
Kleihues P, Louis DN, Scheithauer BW, Rorke LB, Reifenberger G, Burger PC, Cavenee WK (2002) The WHO classification of tumors of the nervous system. J Neuropathol Exp Neurol 61:215–225
Woods RP, Grafton ST, Holmes CJ, Cherry SR, Mazziotta JC (1998) Automated image registration: I. General methods and intrasubject, intramodality validation. J Comput Assist Tomogr 22:139–152
Dvorak HF, Brown LF, Detmar M, Dvorak AM (1995) Vascular permeability factor/vascular endothelial growth factor, microvascular hyperpermeability, and angiogenesis. Am J Pathol 146:1029–1039
Shweiki D, Neerman M, Itin A, Keshet E (1995) Induction of vascular endothelial growth factor expression by hypoxia and by glucose deficiency in multicell spheroids: implications for tumor angiogenesis. Proc Natl Acad Sci U S A 92:768–772
Black KL, Ningaraj NS (2004) Modulation of tumor capillaries for enhanced drug delivery selectively to brain tumor. Cancer Control 11:165–173
Chio CC, Baba T, Black KL (1992) Selective blood-tumor barrier disruption by leukotrienes. J Neurosurg 77:407–410
Uchida M, Chen Z, Liu Y, Black KL (2002) Overexpression of bradykinin type 2 receptors on glioma cells enhances bradykinin-mediated blood-brain tumor barrier permeability increase. Neurol Res 24:739–774
Premack BA, Schall TJ (1996) Chemokine receptors: gateways to inflammation and infection. Nat Med 2:1174–1178
Maenpaa A, Kovanen PE, Paetau A, Jaaskelainen J, Timonen T (1997) Lymphocyte adhesion molecule ligands and extracellular matrix proteins in gliomas and normal brain: expression of VCAM-1 in gliomas. Acta Neuropathol 94:216–225
Badruddoja MA, Krouwer HG, Rand SD, Rebro KJ, Pathak AP, Schmainda KM (2003) Antiangiogenic effects of dexamethasone in 9L gliosarcoma assessed by MRI cerebral blood volume maps. Neuro Oncol 5:235–243
Law M, Yang S, Babb JS, Knopp EA, Golfinos JG, Zagzag D, Johnson G (2004) Comparison of cerebral blood volume and vascular permeability from dynamic susceptibility contrast enhanced perfusion MR imaging with glioma grade. AJNR Am J Neuroradiol 25:746–755
Patankar TF, Haroon HA, Mills SJ, Baleriaux D, Bukley DL, Parker GJ (2005) Is volume transfer coefficient (ktrans) related to histologic grade in human gliomas. AJNR Am J Neuroradiol 26:2455–2465
Roberts HC, Roberts TP, Brasch RC, Dillon WP (2000) Quantitative measurement of microvascular permeability in human brain tumors achieved using dynamic contrast-enhanced MR imaging: correlation with histologic grade. AJNR Am J Neuroradiol 21:891–899
Acknowledgements
This work was funded by the Department of Science and Technology, New Delhi (grant no. SP/SO/HS-50/2002). Mohammad Haris received financial assistance from the University Grant Commission, New Delhi. Anup Singh received financial assistance from the Council of Scientific and Industrial Research, New Delhi.
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haris, M., Gupta, R.K., Singh, A. et al. Differentiation of infective from neoplastic brain lesions by dynamic contrast-enhanced MRI. Neuroradiology 50, 531–540 (2008). https://doi.org/10.1007/s00234-008-0378-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-008-0378-6