Abstract
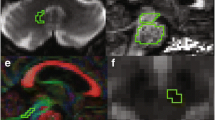
The purpose of the study was to explore the possibilities of using diffusion tensor imaging (DTI) and tractography (DTT) for the differential diagnosis and monitoring of disease progression in idiopathic Parkinson’s disease (IPD), compared with the atypical parkinsonian disorders multiple system atrophy (MSA) and progressive supranuclear palsy (PSP). A 3.0-T MR scanner was used. DTI was acquired using a single-shot EPI sequence with diffusion encoding in 32 directions and a voxel size of 2 × 2 × 2 mm3. DTI data were analysed and DTT was performed using the PRIDE fibre tracking tool supplied by the manufacturer. The fractional anisotropy (FA) and apparent diffusion coefficient (ADC) within each tract were determined. DTI and DTT images in patients with moderate to advanced MSA demonstrated degeneration of the middle cerebellar peduncles and pontine crossing tracts, with decreased FA and increased ADC. This accounted for most of the pontine and cerebellar atrophy characteristic of this disease. In contrast, patients with PSP showed a selective degeneration of the superior cerebellar peduncle. Three-dimensional images of whole-brain white matter tracts demonstrated a reduction of cortical projection fibres in all patients with PSP. Visualization of the selective degeneration of individual fibre tracts, using DTI and DTT, adds qualitative data facilitating the differential diagnosis of parkinsonian disorders. Repeated measurements of FA and ADC values in a whole fibre tract might be used for monitoring disease progression and studying the effect of treatment in neuroprotective trials. The results are preliminary considering the small number of subjects in the study.





Similar content being viewed by others
References
Litvan I, Bhatia KP, Burn DJ, Goetz CG, Lang AE, McKeith I, Quinn N, Sethi KD, Shults C, Wenning GK (2003) Movement Disorders Society Scientific Issues Committee report: SIC Task Force appraisal of clinical diagnostic criteria for Parkinsonian disorders. Mov Disord 18:467–486
Schrag A, Kingsley D, Phatouros C, Mathias CJ, Lees AJ, Daniel SE, Quinn NP (1998) Clinical usefulness of magnetic resonance imaging in multiple system atrophy. J Neurol Neurosurg Psychiatry 65:65–71
Schocke MF, Seppi K, Esterhammer R, Kremser C, Jaschke W, Poewe W, Wenning GK (2002) Diffusion-weighted MRI differentiates the Parkinson variant of multiple system atrophy from PD. Neurology 58:575–580
Schocke MF, Seppi K, Esterhammer R, Kremser C, Mair KJ, Czermak BV, Jaschke W, Poewe W, Wenning GK (2004) Trace of diffusion tensor differentiates the Parkinson variant of multiple system atrophy and Parkinson’s disease. Neuroimage 21:1443–1451
Toosy AT, Werring DJ, Orrell RW, Howard RS, King MD, Barker GJ, Miller DH, Thompson AJ (2003) Diffusion tensor imaging detects corticospinal tract involvement at multiple levels in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 74:1250–1257
Sach M, Winkler G, Glauche V, Liepert J, Heimbach B, Koch MA, Büchel C, Weiller C (2004) Diffusion tensor MRI of early upper motor neuron involvement in amyotrophic lateral sclerosis. Brain 127:340–350
Kubicki M, Westin CF, McCarley RW, Shenton ME (2005) The application of DTI to investigate white matter abnormalities in schizophrenia. Ann N Y Acad Sci 1064:134–148
Naggara O, Oppenheim C, Rieu D, Raoux N, Rodrigo S, Dalla Barba G, Meder JF (2006) Diffusion tensor imaging in early Alzheimer’s disease. Psychiatry Res 146:243–249
Jacob S, Finsterbusch J, Weishaupt JH, Khorram-Sefat D, Frahm J, Ehrenreich H (2003) Diffusion tensor imaging for long-term follow-up of corticospinal tract degeneration in amyotrophic lateral sclerosis. Neuroradiology 45:598–600
Yoshikawa K, Nakata Y, Yamada K, Nakagawa M (2004) Early pathological changes in the parkinsonian brain demonstrated by diffusion tensor MRI. J Neurol Neurosurg Psychiatry 75:481–484
de Crespigny AJ, Moseley ME (1998) Eddy current-induced image warping in diffusion-weighted EPI. Proceedings of the International Society for Magnetic Resonance in Medicine, ISMRM, Berkeley, CA, p 661
Stieltjes B, Kaufmann WE, van Zijl PCM, Fredericksen K, Pearlson GD, Solaiyappan M, Mori S (2001) Diffusion tensor imaging and axonal tracking in the human brainstem. Neuroimage 14:723–735
Wakana S, Jiang H, Nagae-Poetscher LM, van Zijl PCM, Mori S (2004) Fiber tract-based atlas of human white matter anatomy. Radiology 230:77–87
Habas C, Cabanis EM (2006) Cortical projections to the human red nucleus: a diffusion tensor tractography study with a 1.5-T MRI machine. Neuroradiology 48:755–762
Salamon N, Sicotte N, Alger J, Shattuck D, Perlman S, Sinha U, Schultze-Haakh H, Salamon G (2005) Analysis of the brain-stem white-matter tracts with diffusion tensor imaging. Neuroradiology 47:895–902
DaSilva AFM, Tuch DS, Wiegell MR, Hadjikhani N (2003) A primer on diffusion tensor imaging of anatomical substructures. Neurosurg Focus 15:1–4
Heimer L (1983) The human brain and spinal cord. Springer-Verlag, Berlin Heidelberg New York, pp 214–221
Osborn AG (ed) (2004) Diagnostic imaging: brain. Amirsys, Salt Lake City, pp I10:78–85
Yekhlef F, Ballan G, Macia F, Delmer O, Sourgen C, Tison F (2003) Routine MRI for the differential diagnosis of Parkinson’s disease, MSA, PSP, and CBD. J Neural Transm 110:151–169
Seppi K, Schocke MF, Esterhammer R, Kremser C, Brenneis C, Mueller J, Boesch S, Jaschke W, Poewe W, Wenning GK (2003) Diffusion-weighted imaging discriminates progressive supranuclear palsy from PD, but not from the parkinson variant of multiple system atrophy. Neurology 60:922–927
Schultz JB, Skalej M, Wedekind D, Luft AR, Abele M, Voigt K, Dichgans J, Klockgether T (1999) Magnetic resonance imaging-based volumetry differentiates idiopathic Parkinson’s syndrome from multiple system atrophy and progressive supranuclear palsy. Ann Neurol 45:65–74
Ghaemi M, Hilker R, Rudolf J, Sobesky J, Heiss W-D (2002) Differentiating multiple system atrophy from Parkinson’s disease: contribution of striatal and midbrain MRI volumetry and multi-tracer PET imaging. J Neurol Neurosurg Psychiatry 73:517–523
Brenneis C, Seppi K, Schocke MF, Müller J, Luginger E, Bösch S, Löscher WN, Büchel C, Poewe W, Wenning GK (2003) Voxel-based morphometry detects cortical atrophy in the Parkinson variant of multiple system atrophy. Mov Disord 18:1132–1138
Boxer AL, Geschwind MD, Belfor N, Gorno-Tempini ML, Schauer GF, Miller BL, Weiner MW, Rosen HJ (2006) Patterns of brain atrophy that differentiate corticobasal degeneration syndrome from progressive supranuclear palsy. Arch Neurol 63:81–86
Paviour DC, Price SL, Jahanshahi M, Lees AJ, Fox NC (2006) Longitudinal MRI in progressive supranuclear palsy and multiple system atrophy: rates and regions of atrophy. Brain 129:1040–1049
Paviour DC, Price SL, Stevens JM, Lees AJ, Fox NC (2005) Quantitative MRI measurement of superior cerebellar peduncle in progressive supranuclear palsy. Neurology 64:675–679
Shiga K, Yamada K, Yoshikawa K, Mizuno T, Nishimura T, Nakagawa M (2005) Local tissue anisotropy decreases in cerebellopetal fibers and pyramidal tract in multiple system atrophy. J Neurol 252:589–596
Nicoletti G, Fera F, Condino F, Auteri W, Gallo O, Pugliese P, Arabia G, Morgante L, Barone P, Zappia M, Quattrone A (2006) MRI imaging of middle cerebellar peduncle width: differentiation of multiple system atrophy from Parkinson disease. Radiology 239:825–830
Padovani A, Borroni B, Brambati SM, Agosti C, Broli M, Alonso R, Scifo P, Bellelli G, Alberici A, Gasparotti R, Perani D (2006) Diffusion tensor imaging and voxel based morphometry in early progressive nuclear palsy. J Neurol Neurosurg Psychiatry 77:457–463
Ohshita T, Oka M, Imon Y, Yamaguchi S, Mimori Y, Nakamura S (2000) Apparent diffusion coefficient measurements in progressive supranuclear palsy. Neuroradiology 42:643–647
Acknowledgements
This study was supported by Lund University Hospital grants for research on Parkinson’s disease. The investigations performed in this study comply with current Swedish laws.
Author information
Authors and Affiliations
Corresponding author
Appendix: Tractography (continued)
Appendix: Tractography (continued)
Different voxel comparison parameters were tested by varying the anisotropy threshold and the direction threshold. No improvement in the detection of fibre tracts could be found at different values compared with the values recommended by the software manufacturer. Therefore, an anisotropy threshold with a minimum FA value of 0.3 and deflection threshold 850 (0 full deflection, 1000 no deflection) were used throughout the systematic tractography described here. Attempts to track both major and minor, supratentorial and infratentorial tracts were made, as detailed in the Results. Tracking of the CST, MCP, SCP, PCT, CC and the ILF was performed systematically in all subjects using multiple ROIs. ROIs were always placed perpendicular to the main direction of the tract so that the whole tract would be included. For the CST, tracking was performed between the posterior crus of the internal capsule at the level of the lateral ventricle and the cerebral peduncle or pons. The MCP was tracked both by using multiple ROIs in the coronal plane within the tract on the left and right side, respectively, and by tracking between ROIs placed in the left and right peduncle. Tractography of the ILF was performed between two ROIs in the coronal plane, separated by a distance of 4 mm, going through the PCTs and the central portion of the CC. In the CC, tractography was performed separately in the genu, central portion and splenium, respectively. The average values for the FA and ADC in each tract was calculated and compared between subjects, as well as for repeated measurements in the same subject. For all structures except the CC and PCT, the average FA and ADC values of the left- and right-sided tracts were calculated.
Rights and permissions
About this article
Cite this article
Nilsson, C., Markenroth Bloch, K., Brockstedt, S. et al. Tracking the neurodegeneration of parkinsonian disorders – a pilot study. Neuroradiology 49, 111–119 (2007). https://doi.org/10.1007/s00234-006-0165-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-006-0165-1