Abstract
Background
Numerous studies have suggested that non-steroidal anti-inflammatory drugs (NSAIDs) might be associated with increased risk of miscarriage. However, these results are conflicting and inconclusive.
Methods
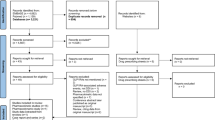
We performed this systematic review and meta-analysis to assess the relationship between NSAIDs exposure and risk of miscarriage. A systematic literature search was conducted to identify relevant studies published from the time of database inception until June 2021.
Results
A total of ten studies involving 207,341 pregnant women were subjected to meta-analysis. There was no statistically significantly increased risk of miscarriage with the use of NSAIDs during pregnancy (OR = 1.37, 95% CI 0.99–1.88, p = 0.057). However, our findings showed that women exposed to NSAIDs around the time of conception were at increased risk of miscarriage (OR 2.32, 95% CI 1.16–4.66, p = 0.018). Furthermore, no significant association between NSAID use and miscarriage was evident during the first trimester of pregnancy (OR = 1, 95% CI = 0.83–1.2, p = 0.996), possibly attributable to the small sample size.
Conclusion
Our findings indicate that NSAID exposure around the time of conception might be a risk factor for miscarriage. Further studies are needed to evaluate whether the risk varies by the type, dosage, or timing of NSAID exposure.



Similar content being viewed by others
References
Patrono C, Rocca B (2009) Nonsteroidal antiinflammatory drugs: past, present and future. Pharmacol Res 59(5):285–289. https://doi.org/10.1016/j.phrs.2009.01.011
Sharma UR, Nediyedath Rathnakaran A, Raj BPP, Padinjakkara G, Das A, Vada S, Mudagal MP (2021) The positive effect of pregnancy in rheumatoid arthritis and the use of medications for the management of rheumatoid arthritis during pregnancy. Inflammopharmacology. https://doi.org/10.1007/s10787-021-00808-9
Jackson E, Kapp N (2020) Pain management for medical and surgical termination of pregnancy between 13 and 24 weeks of gestation: a systematic review. BJOG 127(11):1348–1357. https://doi.org/10.1111/1471-0528.16212
Nezvalová-Henriksen K, Spigset O, Nordeng H (2013) Effects of ibuprofen, diclofenac, naproxen, and piroxicam on the course of pregnancy and pregnancy outcome: a prospective cohort study. BJOG 120(8):948–959. https://doi.org/10.1111/1471-0528.12192
Werler MM, Mitchell AA, Hernandez-Diaz S, Honein MA (2005) Use of over-the-counter medications during pregnancy. Am J Obstet Gynecol 193(3 Pt 1):771–777. https://doi.org/10.1016/j.ajog.2005.02.100
Crespin S, Bourrel R, Hurault-Delarue C, Lapeyre-Mestre M, Montastruc JL, Damase-Michel C (2011) Drug prescribing before and during pregnancy in south west France: a retrolective study. Drug Saf 34(7):595–604. https://doi.org/10.2165/11589170-000000000-00000
Quenby S, Gallos ID, Dhillon-Smith RK, Podesek M, Stephenson MD, Fisher J, Brosens JJ, Brewin J, Ramhorst R, Lucas ES, McCoy RC, Anderson R, Daher S, Regan L, Al-Memar M, Bourne T, MacIntyre DA, Rai R, Christiansen OB, Sugiura-Ogasawara M, Odendaal J, Devall AJ, Bennett PR, Petrou S, Coomarasamy A (2021) Miscarriage matters: the epidemiological, physical, psychological, and economic costs of early pregnancy loss. Lancet 397(10285):1658–1667. https://doi.org/10.1016/s0140-6736(21)00682-6
Haw B, Murugesu N, Tobias A, Zamora J, Khan KS (2019) Management of first-trimester miscarriage: a systematic review and network meta-analysis. Hum Reprod Update 25(3):362–374. https://doi.org/10.1093/humupd/dmz002
Magro Malosso ER, Saccone G, Simonetti B, Squillante M, Berghella V (2018) US trends in abortion and preterm birth. J Matern Fetal Neonatal Med 31(18):2463–2467. https://doi.org/10.1080/14767058.2017.1344963
Kaczynski P, Kowalewski MP, Waclawik A (2016) Prostaglandin F2α promotes angiogenesis and embryo-maternal interactions during implantation. Reproduction 151(5):539–552. https://doi.org/10.1530/rep-15-0496
Dawood MY (1993) Nonsteroidal antiinflammatory drugs and reproduction. Am J Obstet Gynecol 169(5):1255–1265. https://doi.org/10.1016/0002-9378(93)90292-q
van der Weiden RM, Helmerhorst FM, Keirse MJ (1991) Influence of prostaglandins and platelet activating factor on implantation. Hum Reprod 6(3):436–442
van der Weiden RM, Wouters JM (1997) Infertility may sometimes be associated with non-steroidal anti-inflammatory drug consumption. Br J Rheumatol 36(5):605. https://doi.org/10.1093/rheumatology/36.5.605a
Hultzsch S, Paulus W, Padberg S, Fietz AK, Schaefer C, Dathe K (2021) First trimester naproxen exposure and outcome of pregnancy - A German case series. Reprod Toxicol 103:51–57. https://doi.org/10.1016/j.reprotox.2021.05.006
Nielsen GL, Sørensen HT, Larsen H, Pedersen L (2001) Risk of adverse birth outcome and miscarriage in pregnant users of non-steroidal anti-inflammatory drugs: population based observational study and case-control study. BMJ 322(7281):266–270. https://doi.org/10.1136/bmj.322.7281.266
Li DK, Liu L, Odouli R (2003) Exposure to non-steroidal anti-inflammatory drugs during pregnancy and risk of miscarriage: population based cohort study. BMJ 327(7411):368. https://doi.org/10.1136/bmj.327.7411.368
Nakhai-Pour HR, Broy P, Sheehy O, Bérard A (2011) Use of nonaspirin nonsteroidal anti-inflammatory drugs during pregnancy and the risk of spontaneous abortion. CMAJ 183(15):1713–1720. https://doi.org/10.1503/cmaj.110454
Bérard A, Kori S (2012) Dihydroergotamine (DHE) use during gestation and the risk of adverse pregnancy outcomes. Headache 52(7):1085–1093. https://doi.org/10.1111/j.1526-4610.2012.02172.x
Edwards DR, Aldridge T, Baird DD, Funk MJ, Savitz DA, Hartmann KE (2012) Periconceptional over-the-counter nonsteroidal anti-inflammatory drug exposure and risk for spontaneous abortion. Obstet Gynecol 120(1):113–122. https://doi.org/10.1097/AOG.0b013e3182595671
Daniel S, Koren G, Lunenfeld E, Bilenko N, Ratzon R, Levy A (2014) Fetal exposure to nonsteroidal anti-inflammatory drugs and spontaneous abortions. CMAJ 186(5):E177-182. https://doi.org/10.1503/cmaj.130605
Daniel S, Koren G, Lunenfeld E, Levy A (2015) NSAIDs and spontaneous abortions - true effect or an indication bias? Br J Clin Pharmacol 80(4):750–754. https://doi.org/10.1111/bcp.12653
Dathe K, Fietz AK, Pritchard LW, Padberg S, Hultzsch S, Meixner K, Meister R, Schaefer C (2018) No evidence of adverse pregnancy outcome after exposure to ibuprofen in the first trimester - Evaluation of the national Embryotox cohort. Reprod Toxicol 79:32–38. https://doi.org/10.1016/j.reprotox.2018.05.003
Dathe K, Padberg S, Hultzsch S, Köhler LM, Meixner K, Fietz AK, Tissen-Diabaté T, Meister R, Schaefer C (2018) Exposure to cox-2 inhibitors (coxibs) during the first trimester and pregnancy outcome: a prospective observational cohort study. Eur J Clin Pharmacol 74(4):489–495. https://doi.org/10.1007/s00228-017-2385-1
Li DK, Ferber JR, Odouli R, Quesenberry C (2018) Use of nonsteroidal antiinflammatory drugs during pregnancy and the risk of miscarriage. Am J Obstet Gynecol 219(3):275.e271-275.e278. https://doi.org/10.1016/j.ajog.2018.06.002
Padberg S, Tissen-Diabaté T, Dathe K, Hultzsch S, Meixner K, Linsenmeier V, Meister R, Schaefer C (2018) Safety of diclofenac use during early pregnancy: A prospective observational cohort study. Reprod Toxicol 77:122–129. https://doi.org/10.1016/j.reprotox.2018.02.007
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283 (15): 2008–2012. https://doi.org/10.1001/jama.283.15.2008
Higgins JP (2014) Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane collaboration. Available at: www.cochrane-handbook.org [6 December 2014]
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558. https://doi.org/10.1002/sim.1186
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634. https://doi.org/10.1136/bmj.315.7109.629
Antonucci R, Zaffanello M, Puxeddu E, Porcella A, Cuzzolin L, Pilloni MD, Fanos V (2012) Use of non-steroidal anti-inflammatory drugs in pregnancy: impact on the fetus and newborn. Curr Drug Metab 13(4):474–490. https://doi.org/10.2174/138920012800166607
Bloor M, Paech M (2013) Nonsteroidal anti-inflammatory drugs during pregnancy and the initiation of lactation. Anesth Analg 116(5):1063–1075. https://doi.org/10.1213/ANE.0b013e31828a4b54
Mahesh G, Anil Kumar K, Reddanna P (2021) Overview on the Discovery and Development of Anti-Inflammatory Drugs: Should the Focus Be on Synthesis or Degradation of PGE(2)? J Inflamm Res 14:253–263. https://doi.org/10.2147/jir.S278514
Koslowsky B, Grisaru-Granovsky S, Livovsky DM, Milgrom Y, Goldin E, Bar-Gil Shitrit A (2018) Pregnancy-Onset Inflammatory Bowel Disease: A Subtle Diagnosis. Inflamm Bowel Dis 24(8):1826–1832. https://doi.org/10.1093/ibd/izy081
Miranda-Hernández D, Sánchez A, Sánchez-Briones RE, Rivas-Ruiz R, Cruz-Reynoso L, Cruz-Domínguez P, Jara LJ, Saavedra M (2020) Impact of Systemic Lupus Erythematosus on Pregnancy: Analysis of a Large 10-Year Longitudinal Mexican Cohort. J Clin Rheumatol. https://doi.org/10.1097/rhu.0000000000001626
Sugawara E, Kato M, Fujieda Y, Oku K, Bohgaki T, Yasuda S, Umazume T, Morikawa M, Watari H, Atsumi T (2019) Pregnancy outcomes in women with rheumatic diseases: a real-world observational study in Japan. Lupus 28(12):1407–1416. https://doi.org/10.1177/0961203319877258
Acknowledgements
X.H.Y. and Y.D.S. conceived the study and revised the manuscript critically for important intellectual content. D.N.B. and H.Y.J. made substantial contributions to its design, acquisition, analysis, and interpretation of data.
Funding
The authors report no funds received for this study.
Author information
Authors and Affiliations
Contributions
X.H.Y. and D.N.B. searched the library and wrote the manuscript text. D.N.B. and H.Y.J. extracted data and reviewed all articles. X.H.Y. and Y.D.S. evaluated the bias. Y.D.S. designed the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval
No ethical approval was required for this review, as all data were already published in peer-reviewed journals.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ying, Xh., Bao, Dn., Jiang, Hy. et al. Maternal non-steroidal anti-inflammatory drug exposure during pregnancy and risk of miscarriage: a systematic review and meta-analysis. Eur J Clin Pharmacol 78, 171–180 (2022). https://doi.org/10.1007/s00228-021-03222-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-021-03222-w