Abstract
Purpose
Acute nephrotoxicity is a common adverse reaction of tacrolimus therapy; however, its risk factors in pediatric nephrotic syndrome (NS) remain to be evaluated. The objective of this study was to investigate the risk factors and characteristics of tacrolimus-induced acute nephrotoxicity in children with NS.
Methods
Past records of children with NS admitted to our hospital from 2014 to 2018 were reviewed. The incidence and characteristics of nephrotoxicity were analyzed. Multivariate logistic regression analysis was used to identify the risk factors of nephrotoxicity. A clinically applicable risk score was developed and validated.
Results
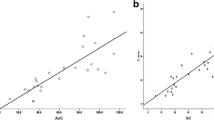
Tacrolimus-induced nephrotoxicity occurred in 25 of 129 patients, 13 patients were grade 1, and the renal function was recovered in 22 patients. Multivariate regression analysis showed that the maximum trough concentrations (C12h) of tacrolimus (OR, 1.48; 95% CI, 1.16 to 1.88; P < 0.001), huaiqihuang granules (OR, 0.095; 95% CI, 0.014 to 0.66; P = 0.017), and diarrhea (OR, 22.00; 95% CI, 1.58 to 306.92; P = 0.022) were independently associated with tacrolimus-induced nephrotoxicity. The maximum C12h were significantly higher in patients with nephrotoxicity (median 9.0 ng/ml) and the cut-off value for acute nephrotoxicity was 6.5 ng/ml. The area under the receiver operating characteristic curve was 0.821 for the proposed model based on the observations used to create the model and 0.817 obtained from k-fold cross-validation.
Conclusions
High trough concentration of tacrolimus and diarrhea can potentiate the risk of tacrolimus-induced acute nephrotoxicity in children with NS, while huaiqihuang granules can protect this condition.


Similar content being viewed by others
References
Group KDIGOKGW (2012) KDIGO clinical practice guideline for glomerulonephritis. Kidney Int Suppl 2:139–274
Wang X, Xu H (2013) New insights into treatment of nephrotic syndrome in children. Contrib Nephrol 181:119–130. https://doi.org/10.1159/000348470
Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D, Kellum JA (2006) RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit Care 10(3):R73. https://doi.org/10.1186/cc4915
Noone DG, Iijima K, Parekh R (2018) Idiopathic nephrotic syndrome in children. Lancet 392(10141):61–74. https://doi.org/10.1016/S0140-6736(18)30536-1
Xia T, Zhu S, Wen Y, Gao S, Li M, Tao X, Zhang F, Chen W (2018) Risk factors for calcineurin inhibitor nephrotoxicity after renal transplantation: a systematic review and meta-analysis. Drug Des Devel Ther 12:417–428. https://doi.org/10.2147/DDDT.S149340
Segarra A, Vila J, Pou L, Majo J, Arbos A, Quiles T, Piera LL (2002) Combined therapy of tacrolimus and corticosteroids in cyclosporin-resistant or -dependent idiopathic focal glomerulosclerosis: a preliminary uncontrolled study with prospective follow-up. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association 17(4):655–662
Pinana JL, Perez-Pitarch A, Garcia-Cadenas I, Barba P, Hernandez-Boluda JC, Esquirol A, Fox ML, Terol MJ, Queralto JM, Vima J, Valcarcel D, Ferriols-Lisart R, Sierra J, Solano C, Martino R (2017) A time-to-event model for acute kidney injury after reduced-intensity conditioning stem cell transplantation using a tacrolimus- and sirolimus-based graft-versus-host disease prophylaxis. Biology of blood and marrow transplantation. J Am Soc Blood Marrow Transplant 23(7):1177–1185. https://doi.org/10.1016/j.bbmt.2017.03.035
Sikma MA, Hunault CC, van de Graaf EA, Verhaar MC, Kesecioglu J, de Lange DW, Meulenbelt J (2017) High tacrolimus blood concentrations early after lung transplantation and the risk of kidney injury. Eur J Clin Pharmacol 73(5):573–580. https://doi.org/10.1007/s00228-017-2204-8
Wu Z, Xu Q, Qiu X, Jiao Z, Zhang M, Zhong M (2017) FOXP3 rs3761548 polymorphism is associated with tacrolimus-induced acute nephrotoxicity in renal transplant patients. Eur J Clin Pharmacol 73(1):39–47. https://doi.org/10.1007/s00228-016-2140-z
Rayar M, Tron C, Jezequel C, Beaurepaire JM, Petitcollin A, Houssel-Debry P, Camus C, Verdier MC, Dehlawi A, Lakehal M, Desfourneaux V, Meunier B, Sulpice L, Bellissant E, Boudjema K, Lemaitre F (2018) High intrapatient variability of tacrolimus exposure in the early period after liver transplantation is associated with poorer outcomes. Transplantation 102(3):e108–e114. https://doi.org/10.1097/TP.0000000000002052
Yang EM, Lee ST, Choi HJ, Cho HY, Lee JH, Kang HG, Park YS, Cheong HI, Ha IS (2016) Tacrolimus for children with refractory nephrotic syndrome: a one-year prospective, multicenter, and open-label study of Tacrobell(R), a generic formula. World Journal of Pediatrics: WJP 12(1):60–65. https://doi.org/10.1007/s12519-015-0062-y
Jahan A, Prabha R, Chaturvedi S, Mathew B, Fleming D, Agarwal I (2015) Clinical efficacy and pharmacokinetics of tacrolimus in children with steroid-resistant nephrotic syndrome. Pediatr Nephrol 30(11):1961–1967. https://doi.org/10.1007/s00467-015-3133-3
Roberti I, Vyas S (2010) Long-term outcome of children with steroid-resistant nephrotic syndrome treated with tacrolimus. Pediatr Nephrol 25(6):1117–1124. https://doi.org/10.1007/s00467-010-1471-8
Choudhry S, Bagga A, Hari P, Sharma S, Kalaivani M, Dinda A (2009) Efficacy and safety of tacrolimus versus cyclosporine in children with steroid-resistant nephrotic syndrome: a randomized controlled trial. American journal of kidney diseases : the official journal of the National Kidney Foundation 53(5):760–769. https://doi.org/10.1053/j.ajkd.2008.11.033
Pandirikkal VB, Jain M, Gulati S (2007) Tacrolimus-induced HUS: an unusual cause of acute renal failure in nephrotic syndrome. Pediatr Nephrol 22(2):298–300. https://doi.org/10.1007/s00467-006-0265-5
Sinha R, Marks SD (2013) Tacrolimus toxicity secondary to diarrhoea in nephrotic syndrome. Acta Paediatr 102(7):e291–e292. https://doi.org/10.1111/apa.12260
Group KDIGOKAKIW (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138
Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, Janecek E, Domecq C, Greenblatt DJ (1981) A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 30(2):239–245
Chawla LS, Bellomo R, Bihorac A, Goldstein SL, Siew ED, Bagshaw SM, Bittleman D, Cruz D, Endre Z, Fitzgerald RL, Forni L, Kane-Gill SL, Hoste E, Koyner J, Liu KD, Macedo E, Mehta R, Murray P, Nadim M, Ostermann M, Palevsky PM, Pannu N, Rosner M, Wald R, Zarbock A, Ronco C, Kellum JA, Acute Disease Quality Initiative W (2017) Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat Rev Nephrol 13(4):241–257. https://doi.org/10.1038/nrneph.2017.2
Group KDIGOKCKDW (2012) Clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3(1):1–150
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol : JASN 20(3):629–637. https://doi.org/10.1681/ASN.2008030287
Sullivan LM, Massaro JM, D’Agostino RB Sr (2004) Presentation of multivariate data for clinical use: the Framingham Study risk score functions. Stat Med 23(10):1631–1660. https://doi.org/10.1002/sim.1742
Li J, Chen S, Qin X, Fu Q, Bi H, Zhang Y, Wang X, Liu L, Wang C, Huang M (2017) Wuzhi Tablet (Schisandra sphenanthera Extract) is a promising tacrolimus-sparing agent for renal transplant recipients who are CYP3A5 expressers: a two-phase prospective study. Drug Metab Dispos: the biological fate of chemicals 45(11):1114–1119. https://doi.org/10.1124/dmd.117.076737
Kuypers DR, Claes K, Evenepoel P, Maes B, Vanrenterghem Y (2004) Clinical efficacy and toxicity profile of tacrolimus and mycophenolic acid in relation to combined long-term pharmacokinetics in de novo renal allograft recipients. Clin Pharmacol Ther 75(5):434–447. https://doi.org/10.1016/j.clpt.2003.12.009
Dansirikul C, Staatz CE, Duffull SB, Taylor PJ, Lynch SV, Tett SE (2006) Relationships of tacrolimus pharmacokinetic measures and adverse outcomes in stable adult liver transplant recipients. J Clin Pharm Ther 31(1):17–25. https://doi.org/10.1111/j.1365-2710.2006.00697.x
Wingard JR, Nash RA, Przepiorka D, Klein JL, Weisdorf DJ, Fay JW, Zhu J, Maher RM, Fitzsimmons WE, Ratanatharathorn V (1998) Relationship of tacrolimus (FK506) whole blood concentrations and efficacy and safety after HLA-identical sibling bone marrow transplantation. Biol Blood Marrow Transplant : journal of the American Society for Blood and Marrow Transplantation 4(3):157–163. https://doi.org/10.1053/bbmt.1998.v4.pm9923414
Niioka T, Komatsuda A, Kato S, Togashi M, Okuyama S, Omokawa A, Nara M, Wakui H, Takahashi N, Miura M (2015) Effects of CYP3A5 polymorphism and the tacrolimus 12 h concentration on tacrolimus-induced acute renal dysfunction in patients with lupus nephritis. Xenobiotica; the fate of foreign compounds in biological systems 45(12):1147–1153. https://doi.org/10.3109/00498254.2015.1045571
Vanhove T, Annaert P, Kuypers DR (2016) Clinical determinants of calcineurin inhibitor disposition: a mechanistic review. Drug Metab Rev 48(1):88–112. https://doi.org/10.3109/03602532.2016.1151037
Xu X, Nie S, Zhang A, Mao J, Liu HP, Xia H, Xu H, Liu Z, Feng S, Zhou W, Liu X, Yang Y, Tao Y, Feng Y, Chen C, Wang M, Zha Y, Feng JH, Li Q, Ge S, Chen J, He Y, Teng S, Hao C, Liu BC, Tang Y, He W, He P, Hou FF (2018) Acute kidney injury among hospitalized children in China. Clin Journal Am Soc Nephrol : CJASN 13(12):1791–1800. https://doi.org/10.2215/CJN.00800118
Hong T, Zhang M, Fan J (2015) Cordyceps sinensis (a traditional Chinese medicine) for kidney transplant recipients. Cochrane Database Syst Rev 10:CD009698. https://doi.org/10.1002/14651858.CD009698.pub2
Guo Y, Wang M, Mou J, Zhao Z, Yang J, Zhu F, Pei G, Zhu H, Wang Y, Xu G, Zeng R, Yao Y (2018) Pretreatment of Huaiqihuang extractum protects against cisplatin-induced nephrotoxicity. Sci Rep 8(1):7333. https://doi.org/10.1038/s41598-018-25610-6
Liu H, Sun W, Gu LB, Tu Y, Yu BY, Hu H (2017) Huaiqihuang granules () reduce proteinuria by enhancing nephrin expression and regulating necrosis factor kappaB signaling pathway in adriamycin-induced nephropathy. Chin J Integr Med 23(4):279–287. https://doi.org/10.1007/s11655-015-2293-0
Naesens M, Kuypers DR, Sarwal M (2009) Calcineurin inhibitor nephrotoxicity. Clin J Am Soc Nephrol : CJASN 4(2):481–508. https://doi.org/10.2215/CJN.04800908
Cumming AD, Jeffrey S, Lambie AT, Robson JS (1989) The kallikrein-kinin and renin-angiotensin systems in nephrotic syndrome. Nephron 51(2):185–191. https://doi.org/10.1159/000185283
Moss NG, Powell SL, Falk RJ (1985) Intravenous cyclosporine activates afferent and efferent renal nerves and causes sodium retention in innervated kidneys in rats. Proc Natl Acad Sci U S A 82(23):8222–8226
Hausberg M, Lang D, Levers A, Suwelack B, Kisters K, Tokmak F, Barenbrock M, Kosch M (2006) Sympathetic nerve activity in renal transplant patients before and after withdrawal of cyclosporine. J Hypertens 24(5):957–964. https://doi.org/10.1097/01.hjh.0000222767.15100.e4
Xu JR, Zhu JM, Jiang J, Ding XQ, Fang Y, Shen B, Liu ZH, Zou JZ, Liu L, Wang CS, Ronco C, Liu H, Teng J (2015) Risk factors for long-term mortality and progressive chronic kidney disease associated with acute kidney injury after cardiac surgery. Medicine 94(45):e2025. https://doi.org/10.1097/MD.0000000000002025
Funding
This work was supported by grants from the Wuhan Health and Family Planning Commission (No. WZ18Q03 to P.G.) and National Natural Scientific Foundation of China (NSFC, No.81803503 to X.L.G.; No. 71874062 to R.H.).
Author information
Authors and Affiliations
Contributions
PG, HX, and XW planned the study; PG and XG collected the data and wrote the manuscript; RH and XS carried out the statistical analyses; JL and ML contributed to the interpretation of the data. All authors contributed to, and have approved, the final manuscript.
Corresponding authors
Ethics declarations
The study was approved by the local ethical committees of Wuhan Children’s Hospital.
Conflict of interest
There are no conflicts of interests to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gao, P., Guan, XL., Huang, R. et al. Risk factors and clinical characteristics of tacrolimus-induced acute nephrotoxicity in children with nephrotic syndrome: a retrospective case-control study. Eur J Clin Pharmacol 76, 277–284 (2020). https://doi.org/10.1007/s00228-019-02781-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-019-02781-3