Abstract
Purpose
This study was designed to evaluate the association of non-genetic factors and polymorphisms CYP2C9*2 (rs1799853), CYP2C9*3 (rs1075910), and VKORC1-G1639A (rs9923231) with time in therapeutic range (TTR), and to build a regression model to predict the quality of oral anticoagulation control in a sample of Brazilian patients.
Methods
This is a retrospective cohort study developed at an anticoagulation clinic of a university hospital. Overall, 312 patients were included. The quality of oral anticoagulation control was evaluated by TTR. TTR was dichotomized for analysis, using two cutoff points for classification as inadequate (TTR ≤ 60.0%) and optimal (TTR ≥ 75.0%) control.
Results
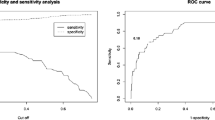
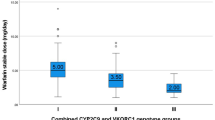
The average age was 60.4 ± 13.5 years, with a predominance of women (187; 59.9%). The -G1639A polymorphism of the VKORC1 gene, when evaluated, based on the recessive inheritance pattern [AA × (GA + GG)], patients with AA genotype exhibited a higher TTR (68.2% versus 62.8%, p = 0.017). TTR ≤ 60.0% was associated with number of drugs in chronic use, assistance for warfarin administration, reports of not taking warfarin, absenteeism, sex (female), and target INR (International Normalized Ratio; 2.00–3.00). TTR ≥ 75.0% was associated with sex (male), target INR (2.00–3.00), assistance for warfarin administration, reports of not taking warfarin, and absenteeism. The two algorithms proposed showed adequate ability to predict TTR presenting good sensitivity and specificity.
Conclusions
Our findings provided useful information for risk stratification depending on TTR level and for future investigations on the quality of oral anticoagulation control in Brazilian anticoagulation clinics.
Similar content being viewed by others
References
Wiedermann CJ, Stockner I (2008) Warfarin-induced bleeding complications - clinical presentation and therapeutic options. Thromb Res 122(Suppl):S13–S18. https://doi.org/10.1016/S0049-3848(08)70004-5
Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti G (2012) Oral anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141:e44S–e88S. https://doi.org/10.1378/chest.11-2292
Rosendaal FR, Cannegieter SC, van der Meer FJ, Briet E (1993) A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost 69:236–239
Connolly SJ, Pogue J, Eikelboom J et al (2008) Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centers and countries as measured by time in therapeutic range. Circulation 118:2029–2037. https://doi.org/10.1161/CIRCULATIONAHA.107.750000
Schein JR, White CM, Nelson WW, Kluger J, Mearns ES, Coleman CI (2016) Vitamin K antagonist use: evidence of the difficulty of achieving and maintaining target INR range and subsequent consequences. Thromb J 14:14. https://doi.org/10.1186/s12959-016-0088-y
Vazquez FJ, Gonzalez JP, LeGal G, Carrier M, Gándara E (2016) Risk of major bleeding in patients receiving vitamin K antagonists or low doses of aspirin. A systematic review and meta-analysis. Thromb Res 138:1–6. https://doi.org/10.1016/j.thromres.2015.12.013
White HD, Gruber M, Feyzi J, Kaatz S, Tse HF, Husted S, Albers GW (2007) Comparison of outcomes among patients randomized to warfarin therapy according to anticoagulant control: results from SPORTIF III and V. Arch Intern Med 167:239–245. https://doi.org/10.1001/archinte.167.3.239
van Walraven C, Jennings A, Oake N, Fergusson D, Forster AJ (2006) Effect of study setting on anticoagulation control: a systematic review and metaregression. Chest 129:1155–1166. https://doi.org/10.1378/chest.129.5.1155
Costa GL, Lamego RM, Colosimo EA et al (2012) Identifying potential predictors of high-quality oral anticoagulation assessed by time in therapeutic international normalized ratio range: a prospective, long-term, single-center, observational study. Clin Ther 34:1511–1520. https://doi.org/10.1016/j.clinthera.2012.06.002
Leite PM, Castilho RO, Ribeiro AL, Martins MA (2016) Consumption of medicinal plants by patients with heart diseases at a pharmacist-managed anticoagulation clinic in Brazil. Int J Clin Pharm 38:223–227. https://doi.org/10.1007/s11096-016-0270-0
Pirmohamed M, Burnside G, Eriksson N, Jorgensen AL, Toh CH, Nicholson T, Kesteven P, Christersson C, Wahlström B, Stafberg C, Zhang JE, Leathart JB, Kohnke H, Maitland-van der Zee A, Williamson PR, Daly AK, Avery P, Kamali F, Wadelius M, EU-PACT Group (2013) A randomized trial of genotype-guided dosing of warfarin. N Engl J Med 369:2294–2303. https://doi.org/10.1056/NEJMoa1311386
Dahal K, Sharma SP, Fung E, Lee J, Moore JH, Unterborn JN, Williams SM (2015) Meta-analysis of randomized controlled trials of genotype-guided vs standard dosing of warfarin. Chest 148:701–710. https://doi.org/10.1378/chest.14-2947
Wen MS, Chang KC, Lee TH, Chen YF, Hung KC, Chang YJ, Liou CW, Chen JJ, Chang CH, Wang CY, Jeng JS, Chuang HP, Chen YT, Chen CH, Wu JY, Chen YT, Lee MT (2017) Pharmacogenetic dosing of warfarin in the Han-Chinese population: a randomized trial. Pharmacogenomics 18:245–253. https://doi.org/10.2217/pgs-2016-0154
Finkelman BS, Gage BF, Johnson JA, Brensinger CM, Kimmel SE (2011) Genetic warfarin dosing: tables versus algorithms. J Am Coll Cardiol 57:612–618. https://doi.org/10.1016/j.jacc.2010.08.643
Klein TE, Altman RB, Eriksson N et al (2009) Estimation of the warfarin dose with clinical and pharmacogenetic data. N Engl J Med 360:753–764. https://doi.org/10.1056/NEJMoa0809329
Gage BF, Eby C, Johnson JA et al (2008) Use of pharmacogenetic and clinical factors to predict the therapeutic dose of warfarin. Clin Pharmacol Ther 84:326–331. https://doi.org/10.1038/clpt.2008.10
Francis B, Lane S, Pirmohamed M, Jorgensen A (2014) A review of a priori regression models for warfarin maintenance dose prediction. PLoS One 9:e114896. https://doi.org/10.1371/journal.pone.0114896
Pavani A, Naushad SM, Rupasree Y, Kumar TR, Malempati AR, Pinjala RK, Mishra RC, Kutala VK (2012) Optimization of warfarin dose by population-specific pharmacogenomic algorithm. Pharmacogenomics J 12:306–311. https://doi.org/10.1038/tpj.2011.4
Ekladious SM, Issac MS, El-Atty Sharaf SA, Abou-Youssef HS (2013) Validation of a proposed warfarin dosing algorithm based on the genetic make-up of Egyptian patients. Mol Diagn Ther 17:381–390. https://doi.org/10.1007/s40291-013-0046-3
Cho HJ, On YK, Bang OY et al (2011) Development and comparison of a warfarin-dosing algorithm for Korean patients with atrial fibrillation. Clin Ther 33:1371–1380. https://doi.org/10.1016/j.clinthera.2011.09.004
Skov J, Bladbjerg EM, Leppin A, Jespersen J (2013) The influence of VKORC1 and CYP2C9 gene sequence variants on the stability of maintenance phase warfarin treatment. Thromb Res 131:125–129. https://doi.org/10.1016/j.thromres.2012.11.004
Santos PC, Marcatto LR, Duarte NE et al (2015) Development of a pharmacogenetic-based warfarin dosing algorithm and its performance in Brazilian patients: highlighting the importance of population-specific calibration. Pharmacogenomics 16:865–876. https://doi.org/10.2217/pgs.15.48
Park YK, Lee MJ, Kim JH, Lee JS, Park RW, Kim GM, Chung CS, Lee KH, Kim JS, Lee SY, Bang OY (2017) Genetic and non-genetic factors affecting the quality of anticoagulation control and vascular events in atrial fibrillation. J Stroke Cerebrovasc Dis 26:1383–1390. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.02.022
Friedrich DC, Genro JP, Sortica VA, Suarez-Kurtz G, de Moraes ME, Pena SD, dos Santos A, Romano-Silva MA, Hutz MH (2014) Distribution of CYP2D6 alleles and phenotypes in the Brazilian population. PLoS One 9:e110691. https://doi.org/10.1371/journal.pone.0110691
de Lima Silva RG, Bertollo CM, Ferreira IG, Brant LC, Martins MAP (2017) Assessment of oral anticoagulation control at two pharmacist-managed clinics in Brazil. Int J Clin Pharm 39:1157–1161. https://doi.org/10.1007/s11096-017-0511-x
Skinner HA, Holt S, Schuller R, Roy J, Israel Y (1984) Identification of alcohol abuse using laboratory tests and a history of trauma. Ann Intern Med 101:847–851
Perini JA, Struchiner CJ, Silva-Assuncao E et al (2008) Pharmacogenetics of warfarin: development of a dosing algorithm for brazilian patients. Clin Pharmacol Ther 84:722–728. https://doi.org/10.1038/clpt.2008.166
Kaatz S, Ahmad D, Spyropoulos AC, Schulman S (2015) Definition of clinically relevant non-major bleeding in studies of anticoagulants in atrial fibrillation and venous thromboembolic disease in non-surgical patients: communication from the SSC of the ISTH. J Thromb Haemost. https://doi.org/10.1111/jth.13140
Redman AR, Zheng J, Shamsi SA, Huo J, Kelly EJ, Ho RJ, Ritchie DM, Hon YY (2008) Variant CYP2C9 alleles and warfarin concentrations in patients receiving low-dose versus average-dose warfarin therapy. Clin Appl Thromb Hemost 14:29–37. https://doi.org/10.1177/1076029607304403
Gage BF, Eby C, Milligan PE, Banet GA, Duncan JR, McLeod H (2004) Use of pharmacogenetics and clinical factors to predict the maintenance dose of warfarin. Thromb Haemost 91:87–94. https://doi.org/10.1160/TH03-06-0379
Abohelaika S, Kamali F, Avery P, Robinson B, Kesteven P, Wynne H (2014) Anticoagulation control and cost of monitoring of older patients on chronic warfarin therapy in three settings in North East England. Age Ageing 43:708–711. https://doi.org/10.1093/ageing/afu074
Martins MAP, Costa JM, Mambrini JVM, Ribeiro ALP, Benjamin EJ, Brant LCC, Paasche-Orlow MK, Magnani JW (2017) Health literacy and warfarin therapy at two anticoagulation clinics in Brazil. Heart 103:1089–1095. https://doi.org/10.1136/heartjnl-2016-310699
Oramasionwu CU, Bailey SC, Duffey KE et al (2014) The association of health literacy with time in therapeutic range for patients on warfarin therapy. J Health Commun 19(Suppl 2):19–28. https://doi.org/10.1080/10810730.2014.934934
Yao X, Abraham NS, Alexander GC et al (2016) Effect of adherence to oral anticoagulants on risk of stroke and major bleeding among patients with atrial fibrillation. J Am Heart Assoc 5. https://doi.org/10.1161/JAHA.115.003074
Obamiro KO, Chalmers L, Bereznicki LR (2016) A summary of the literature evaluating adherence and persistence with oral anticoagulants in atrial fibrillation. Am J Cardiovasc Drugs 16:349–363. https://doi.org/10.1007/s40256-016-0171-6
Valdelievre E, Quere I, Care B et al (2018) Time in therapeutic range (TTR) and follow-up of patients on vitamin K antagonist: a cohort analysis. J Med Vasc 43:155–162. https://doi.org/10.1016/j.jdmv.2018.02.001
Apostolakis S, Sullivan RM, Olshansky B, Lip GYH (2013) Factors affecting quality of anticoagulation control among patients with atrial fibrillation on warfarin: the SAMe-TT(2)R(2) score. Chest 144:1555–1563. https://doi.org/10.1378/chest.13-0054
Kim YK, Nieuwlaat R, Connolly SJ, Schulman S, Meijer K, Raju N, Kaatz S, Eikelboom JW (2010) Effect of a simple two-step warfarin dosing algorithm on anticoagulant control as measured by time in therapeutic range: a pilot study. J Thromb Haemost 8:101–106. https://doi.org/10.1111/j.1538-7836.2009.03652.x
Botton MR, Bandinelli E, Rohde LE, Amon LC, Hutz MH (2011) Influence of genetic, biological and pharmacological factors on warfarin dose in a Southern Brazilian population of European ancestry. Br J Clin Pharmacol 72:442–450. https://doi.org/10.1111/j.1365-2125.2011.03942.x
Soares RA, Santos PC, Machado-Coelho GL, do Nascimento RM, Mill JG, Krieger JE, Pereira AC (2012) CYP2C9 and VKORC1 polymorphisms are differently distributed in the Brazilian population according to self-declared ethnicity or genetic ancestry. Genet Test Mol Biomarkers 16:957–963. https://doi.org/10.1089/gtmb.2012.0019
Santos PC, Dinardo CL, Schettert IT, Soares RA, Kawabata-Yoshihara L, Bensenor IM, Krieger JE, Lotufo PA, Pereira AC (2013) CYP2C9 and VKORC1 polymorphisms influence warfarin dose variability in patients on long-term anticoagulation. Eur J Clin Pharmacol 69:789–797. https://doi.org/10.1007/s00228-012-1404-5
de Oliveira Almeida VC, Ribeiro DD, Gomes KB, Godard AL (2014) Polymorphisms of CYP2C9, VKORC1, MDR1, APOE and UGT1A1 genes and the therapeutic warfarin dose in Brazilian patients with twith thrombosis: a prospective cohort study. Mol Diagn Ther 18:675–683. https://doi.org/10.1007/s40291-014-0121-4
Burmester JK, Berg RL, Yale SH, Rottscheit CM, Glurich IE, Schmelzer JR, Caldwell MD (2011) A randomized controlled trial of genotype-based Coumadin initiation. Genet Med 13:509–518. https://doi.org/10.1097/GIM.0b013e31820ad77d
Ansell JE (1999) Empowering patients to monitor and manage oral anticoagulation therapy. JAMA 281:182–183
Heneghan C, Ward A, Perera R, Self-Monitoring Trialist Collaboration, Bankhead C, Fuller A, Stevens R, Bradford K, Tyndel S, Alonso-Coello P, Ansell J, Beyth R, Bernardo A, Christensen TD, Cromheecke ME, Edson RG, Fitzmaurice D, Gadisseur AP, Garcia-Alamino JM, Gardiner C, Hasenkam JM, Jacobson A, Kaatz S, Kamali F, Khan TI, Knight E, Körtke H, Levi M, Matchar D, Menéndez-Jándula B, Rakovac I, Schaefer C, Siebenhofer A, Souto JC, Sunderji R, Gin K, Shalansky K, Völler H, Wagner O, Zittermann A (2012) Self-monitoring of oral anticoagulation: systematic review and meta-analysis of individual patient data. Lancet 379:322–334. https://doi.org/10.1016/S0140-6736(11)61294-4
Christensen TD, Johnsen SP, Hjortdal VE, Hasenkam JM (2007) Self-management of oral anticoagulant therapy: a systematic review and meta-analysis. Int J Cardiol 118:54–61. https://doi.org/10.1016/j.ijcard.2006.06.018
Connock M, Stevens C, Fry-Smith A et al (2007) Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anticoagulation therapy: a systematic review and economic modelling. Health Technol Assess 11(3–4):9–66
Ontario HQ (2009) Point-of-care international normalized ratio (INR) monitoring devices for patients on long-term oral anticoagulation therapy: an evidence-based analysis. Ont Heal Technol Assess Ser 9:1–114
Cryder BT, Felczak MA, Darkwa A, Patel H, Janociak JD, Rihani R (2017) Transition of stable patients from traditional anticoagulation clinic services to telephonic management. Int J Clin Pharm 39:569–572. https://doi.org/10.1007/s11096-017-0428-4
Gurdasani D, Barroso I, Zeggini E, Sandhu MS (2019) Genomics of disease risk in globally diverse populations. Nat Rev Genet 20:520–535. https://doi.org/10.1038/s41576-019-0144-0
Funding
This study was supported by the National Council for Scientific and Technological Development (CNPq), the Coordination for the Improvement of Higher Level Education Personnel (CAPES) and the State of Minas Gerais Research Foundation (FAPEMIG), Brazil, and the Pró-reitoria Pesquisa of the Universidade Federal Minas Gerais, Brazil. KBG, RPS, and MOCR are fellows of CNPq.
Author information
Authors and Affiliations
Contributions
MFSP analyzed the database, interpreted the results obtained, and drafted the manuscript following the suggested recommendations from other authors. MOCR and MAPM contributed significantly to the conception and design of the study, reviewed the study proposal, and participated in drafting the manuscript and in each subsequent revision. AOMM designed the study, organized data collection, analyzed the data, interpreted the results, and revised the manuscript. KBGG and EIFC contributed to the process of genotyping and revised the manuscript critically. EAR provided statistical support and revised the manuscript. RPS provided statistical support, analyzed the data, organized data collection, interpreted the results, and revised the manuscript. DDR critically reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Praxedes, M.F.S., Martins, M.A.P., Mourão, A.O.M. et al. Non-genetic factors and polymorphisms in genes CYP2C9 and VKORC1: predictive algorithms for TTR in Brazilian patients on warfarin. Eur J Clin Pharmacol 76, 199–209 (2020). https://doi.org/10.1007/s00228-019-02772-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-019-02772-4