Abstract
Purpose
This study was designed to investigate the antisecretory activity of rabeprazole administered once daily in doses of 5, 10, 20, and 40 mg and different cytochrome P450 2C19 (CYP2C19) genotypes on gastric pH in healthy individuals. Additional objectives were delineating the nighttime from the daytime effect and determining the relationships between the pharmacokinetics and pharmacodynamics of rabeprazole.
Methods
Eight individuals of each of the three genotypes of CYP2C19—homozygous extensive metabolizers (homo-EMs), heterozygous EMs (hetero-EMs), and poor metabolizers (PMs)—were recruited. Twenty-four individuals received a once-daily dose, with dosing interval 24 h of 5, 10, 20, or 40 mg rabeprazole for 5 days in a 4-period crossover fashion. Twenty-four-hour intragastric pH and plasma rabeprazole concentrations were determined on day 5.
Results
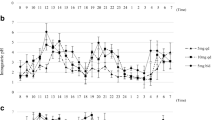
A dose-dependent increase in median pH and in pH 4 holding time was observed across all CYP2C19 genotypes. When rabeprazole was increased from 20 mg to 40 mg, the differences and 95% confidence intervals (CIs) of nighttime pH 4 holding time between 40 mg and 20 mg in homo-EMs, hetero-EMs, and PMs were 8.0% (−5.0% − 21.0%), 28.7% (15.7% − 41.6%), and 16.9% (3.9% − 29.9%), respectively. The relationship between the area under the plasma concentration-time curve up to the last time point at which rabeprazole was quantifiable (AUC0-t) and the pH 4 holding time could be described using a sigmoid maximum effect (Emax) model.
Conclusions
Our data demonstrate that increasing rabeprazole dose up to 40 mg once daily results in an increasing pharmacodynamic effect, which is most apparent for the control of nocturnal gastric acid secretion.



Similar content being viewed by others
References
Sachs G (1997) Proton pump inhibitors and acid-related diseases. Pharmacotherapy 17:22–37
Fass R, Shapiro M, Dekel R, Sewell J (2005) Systematic review: proton-pump inhibitor failure in gastro-oesophageal reflux disease—where next? Aliment Pharmacol Ther 22:79–94
Peghini PL, Katz PO, Bracy NA, Castell DO (1998) Nocturnal recovery of gastric acid secretion with twice-daily dosing of proton pump inhibitors. Am J Gastroenterol 93:763–767
Hatlebakk JG, Katz PO, Kuo B, Castell DO (1998) Nocturnal gastric acidity and acid breakthrough on different regimens of omeprazole 40 mg daily. Aliment Pharmacol Ther 12:1235–1240
Peghini PL, Katz PO, Castell DO (1998) Ranitidine controls nocturnal gastric acid breakthrough on omeprazole: a controlled study in normal subjects. Gastroenterology 115:1335–1339
Adachi K, Fujishiro H, Katsube T, Yuki M, Ono M, Kawamura A, Rumi MA, Watanabe M, Kinoshita Y (2001) Predominant nocturnal acid reflux in patients with Los Angeles grade C and D reflux esophagitis. J Gastroenterol Hepatol 16:1191–1196
Pace F, Pallotta S, Casalini S, Porro GB (2007) A review of rabeprazole in the treatment of acid-related diseases. Ther Clin Risk Manag 3:363–379
Lew EA, Barbuti RC, Kovacs TO, Sytnic B, Humphries TJ, Walsh JH (1998) An ascending single-dose safety and tolerance study of an oral formulation of rabeprazole (E3810). Aliment Pharmacol Ther 12:667–672
Williams MP, Blanshard C, Millson C, Sercombe J, Pounder RE (2000) A placebo-controlled study to assess the effects of 7-day dosing with 10, 20 and 40 mg rabeprazole on 24-h intragastric acidity and plasma gastrin in healthy male subjects. Aliment Pharmacol Ther 14:691–699
Ohning GV, Barbuti RC, Kovacs TO, Sytnik B, Humphries TJ, Walsh JH (2000) Rabeprazole produces rapid, potent, and long-acting inhibition of gastric acid secretion in subjects with Helicobacter pylori infection. Aliment Pharmacol Ther 14:701–708
Robinson M, Maton PN, Rodriguez S, Greenwood B, Humphries TJ (1997) Effects of oral rabeprazole on oesophageal and gastric pH in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther 11:973–980
Shimatani T, Inoue M, Kuroiwa T, Horikawa Y (2004) Rabeprazole 10 mg twice daily is superior to 20 mg once daily for night-time gastric acid suppression. Aliment Pharmacol Ther 19:113–122
Sugimoto M, Furuta T, Shirai N, Kajimura M, Hishida A, Sakurai M, Ohashi K, Ishizaki T (2004) Different dosage regimens of rabeprazole for nocturnal gastric acid inhibition in relation to cytochrome P450 2 C19 genotype status. Clin Pharmacol Ther 76:290–301
Kinoshita Y, Ashida K, Hongo M; Japan Rabeprazole Study Group for NERD (2011) Randomised clinical trial: a multicentre, double-blind, placebo-controlled study on the efficacy and safety of rabeprazole 5 mg or 10 mg once daily in patients with non-erosive reflux disease. Aliment Pharmacol Ther 33:213–224
Andersson T (1996) Pharmacokinetics, metabolism and interactions of acid pump inhibitors. Focus on omeprazole, lansoprazole and pantoprazole. Clin Pharmacokinet 31:9–28
Shirai N, Furuta T, Moriyama Y, Okochi H, Kobayashi K, Takashima M, Xiao F, Kosuge K, Nakagawa K, Hanai H, Chiba K, Ohashi K, Ishizaki T (2001) Effects of CYP2C19 genotypic differences in the metabolism of omeprazole and rabeprazole on intragastric pH. Aliment Pharmacol Ther 15:1929–1937
Shi S, Klotz U (2008) Proton pump inhibitors: an update of their clinical use and pharmacokinetics. Eur J Clin Pharmacol 64:935–951
Ishizaki T, Horai Y (1999) Review article: cytochrome P450 and the metabolism of proton pump inhibitors – emphasis on rabeprazole. Aliment Pharmacol Ther 13(Suppl 3):27–36
Yasuda S, Horai Y, Tomono Y, Nakai H, Yamato C, Manabe K, Kobayashi K, Chiba K, Ishizaki T (1995) Comparison of the kinetic disposition and metabolism of E3810, a new proton pump inhibitor, and omeprazole in relation to S-mephenytoin 4hydroxylation status. Clin Pharmacol Ther 58:143–154
Adachi K, Katsube T, Kawamura A, Takashima T, Yuki M, Amano K, Ishihara S, Fukuda R, Watanabe M, Kinoshita Y (2000) CYP2C19 genotype status and intragastric pH during dosing with lansoprazole or rabeprazole. Aliment Pharmacol Ther 14:1259–1266
Horai Y, Kimura M, Furuie H, Matsuguma K, Irie S, Koga Y, Nagahama T, Murakami M, Matsui T, Yao T, Urae A, Ishizaki T (2001) Pharmacodynamic effects and kinetic disposition of rabeprazole in relation to CYP2C19 genotypes. Aliment Pharmacol Ther 15:793–803
Ieiri I, Kishimoto Y, Okochi H, Momiyama K, Morita T, Kitano M et al (2001) Comparison of the kinetic disposition of and serum gastrin change by lansoprazole versus rabeprazole during an 8-day dosing scheme in relation to CYP2C19 polymorphism. Eur J Clin Pharmacol 57:485–492
Bell NJ, Hunt RH (1992) Role of gastric acid suppression in the treatment of gastro-oesophageal reflux disease. Gut 33:118–124
Katz PO, Johnson DA, Levine D, Rohss K, Junghard O, Astrand M, Nagy P (2010) A model of healing of Los Angeles grades C and D reflux oesophagitis: is there an optimal time of acid suppression for maximal healing? Aliment Pharmacol Ther 32:443–447
Klotz U (2006) Clinical impact of CYP2C19 polymorphism on the action of proton pump inhibitors: a review of a special problem. Int J Clin Pharmacol Ther 44:297–302
Andersson T, Rohss K, Bredberg E, Hassan-Alin M (2001) Pharmacokinetics and pharmacodynamics of esomeprazole, the S-isomer of omeprazole. Aliment Pharmacol Ther 15:1563–1569
Junghard O, Hassan-Alin M, Hasselgren G (2002) The effect of the area under the plasma concentration vs time curve and the maximum plasma concentration of esomeprazole on intragastric pH. Eur J Clin Pharmacol 58:453–458
Gillen D, Wirz AA, Neithercut WD, Ardill JE, McColl KEL (1999) Helicobacter pylori infection potentiates the inhibition of gastric acid secretion by omeprazole. Gut 44:468–475
Verdu EF, Armstrong D, Fraser R, Viani F, Idstrom JP, Cederberg C, Blum AL (1995) Effect of Helicobacter pylori status on intragastric pH during treatment with omeprazole. Gut 36:539–543
Verdu EF, Armstrong D, Idstrom JP, Labenz J, Stolte M, Dorta G, Börsch G, Blum AL (1995) Effect of curing Helicobacter pylori infection on intragastric pH during treatment with omeprazole. Gut 37:743–748
Acknowledgement
The authors thank Dr. Y. Kinoshita of Shimane University Faculty of Medicine for his valuable comments. The authors also thank all contributing staff members in Sekino Clinical Pharmacology Clinic for their involvement in this study, and the project members in Eisai Co., Ltd., Tokyo, Japan for the preparation support of this paper. The preparation support was also provided by Eisai Inc., Woodcliff Lake, NJ, USA
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hayato, S., Hasegawa, S., Hojo, S. et al. Dose–response relationships of rabeprazole 5, 10, 20, and 40 mg once daily on suppression of gastric acid secretion through the night in healthy Japanese individuals with different CYP2C19 genotypes. Eur J Clin Pharmacol 68, 579–588 (2012). https://doi.org/10.1007/s00228-011-1164-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-011-1164-7