Abstract
Purpose
Vitamin K antagonist (VKA) treatment can successfully prevent thromboembolic complications, but the modality has a narrow therapeutic window and numerous interactions with other pharmaceuticals. The aim of the study reported here was to describe the use of co-medications and the prevalence of polypharmacy among patients treated with VKA.
Methods
In a cross-sectional study, 250 consecutive patients (65% male, median age 68 years, most common indication for VKA treatment: atrial fibrillation) in the maintenance phase of VKA treatment were interviewed about their use of prescription medications, over-the-counter drugs and alternative medicines during the last 7 days.
Results
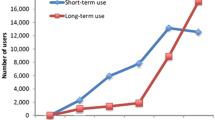
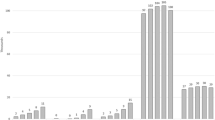
The interviewed patients used a median of five medications (range 1–13), including VKA. Approximately 50% of the patients also took alternative medicines. A wide range of conventional and alternative medicines were used, several of which harbour possible interactions with VKA. Polypharmacy was defined as the use of five or more medications, excluding alternative medicines. The group of polypharmacy patients included 53% of the study population. The use of amiodarone, age >50 years, the indication for VKA treatment being atrial fibrillation or mechanical heart valves and diabetes were independent predictors of polypharmacy.
Conclusions
The results of this study highlight that polypharmacy is a common phenomenon among patients on anticoagulant medication, particularly among elderly patients or those suffering from cardiovascular disease or diabetes.
Similar content being viewed by others
References
Gage BF, van Walraven C, Pearce L, Hart RG, Koudstaal PJ, Boode BS, Petersen P (2004) Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin. Circulation 110:2287–2292
Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, Van Gelder IC, Al-Attar N, Hindricks G, Prendergast B, Heidbuchel H, Alfieri O, Angelini A, Atar D, Colonna P, De CR, De SJ, Goette A, Gorenek B, Heldal M, Hohloser SH, Kolh P, Le Heuzey JY, Ponikowski P, Rutten FH (2010) Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J 31:2369–2429
Oake N, Fergusson DA, Forster AJ, van Walraven C (2007) Frequency of adverse events in patients with poor anticoagulation: a meta-analysis. Can Med Assoc J 176:1589–1594
Njaastad AM, Abildgaard U, Lassen JF (2006) Gains and losses of warfarin therapy as performed in an anticoagulation clinic. J Intern Med 259:296–304
Manotti C, Moia M, Palareti G, Pengo V, Ria L, Dettori AG (2001) Effect of computer-aided management on the quality of treatment in anticoagulated patients: a prospective, randomized, multicenter trial of APROAT (Automated PRogram for Oral Anticoagulant Treatment). Haematologica 86:1060–1070
Poller L, Shiach CR, MacCallum PK, Johansen AM, Munster AM, Magalhaes A, Jespersen J (1998) Multicentre randomised study of computerised anticoagulant dosage. European Concerted Action on Anticoagulation. Lancet 352:1505–1509
Poller L, Keown M, Ibrahim S, Lowe G, Moia M, Turpie AG, Roberts C, van den Besselaar AM, van der Meer FJ, Tripodi A, Palareti G, Shiach C, Bryan S, Samama M, Burgess-Wilson M, Heagerty A, Maccallum P, Wright D, Jespersen J (2008) An international multicenter randomized study of computer-assisted oral anticoagulant dosage vs. medical staff dosage. J Thromb Haemost 6:935–943
Delaney JA, Opatrny L, Brophy JM, Suissa S (2007) Drug–drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding. Can Med Assoc J 177:347–351
Sansone RA, Sansone LA (2009) Warfarin and Antidepressants: Happiness without Hemorrhaging. Psychiatry (Edgmont) 6:24–29
Fugh-Berman A, Ernst E (2001) Herb-drug interactions: review and assessment of report reliability. Br J Clin Pharmacol 52:587–595
Ramsay NA, Kenny MW, Davies G, Patel JP (2005) Complimentary and alternative medicine use among patients starting warfarin. Br J Haematol 130:777–780
Holbrook AM, Pereira JA, Labiris R, McDonald H, Douketis JD, Crowther M, Wells PS (2005) Systematic overview of warfarin and its drug and food interactions. Arch Intern Med 165:1095–1106
Juurlink DN (2007) Drug interactions with warfarin: what clinicians need to know. Can Med Assoc J 177:369–371
Thijssen HH, Soute BA, Vervoort LM, Claessens JG (2004) Paracetamol (acetaminophen) warfarin interaction: NAPQI, the toxic metabolite of paracetamol, is an inhibitor of enzymes in the vitamin K cycle. Thromb Haemost 92:797–802
Poller L, Keown M, Ibrahim S, Lowe G, Moia M, Turpie AG, Roberts C, van den Besselaar AM, van der Meer FJ, Tripodi A, Palareti G, Shiach C, Bryan S, Samama M, Burgess-Wilson M, Heagerty A, Maccallum P, Wright D, Jespersen J (2009) A multicentre randomised assessment of the DAWN AC computer-assisted oral anticoagulant dosage program. Thromb Haemost 101:487–494
Gasse C, Hollowell J, Meier CR, Haefeli WE (2005) Drug interactions and risk of acute bleeding leading to hospitalisation or death in patients with chronic atrial fibrillation treated with warfarin. Thromb Haemost 94:537–543
Schaefer K, Maerkedahl H, Birk HO, Henriksen LO (2010) Polypharmacy in general practice. Dan Med Bull 57:A4165
Atkin PA, Veitch PC, Veitch EM, Ogle SJ (1999) The epidemiology of serious adverse drug reactions among the elderly. Drugs Aging 14:141–152
Onder G, Pedone C, Landi F, Cesari M, Della VC, Bernabei R, Gambassi G (2002) Adverse drug reactions as cause of hospital admissions: results from the Italian Group of Pharmacoepidemiology in the Elderly (GIFA). J Am Geriatr Soc 50:1962–1968
Klein TE, Altman RB, Eriksson N, Gage BF, Kimmel SE, Lee MT, Limdi NA, Page D, Roden DM, Wagner MJ, Caldwell MD, Johnson JA (2009) Estimation of the warfarin dose with clinical and pharmacogenetic data. N Engl J Med 360:753–764
Hanlon JT, Pieper CF, Hajjar ER, Sloane RJ, Lindblad CI, Ruby CM, Schmader KE (2006) Incidence and predictors of all and preventable adverse drug reactions in frail elderly persons after hospital stay. J Gerontol A Biol Sci Med Sci 61:511–515
Wittkowsky AK, Boccuzzi SJ, Wogen J, Wygant G, Patel P, Hauch O (2004) Frequency of concurrent use of warfarin with potentially interacting drugs. Pharmacotherapy 24:1668–1674
Acknowledgements
The authors would like to thank Gunhild Andreasen, Anders Vestergaard Fournaise, Tanja Graff, Anette Larsen, Bodil Leed, Pernille Tandrup Nielsen, Asta Nørregård and Kathrine Overgaard for technical assistance and Jørgen Gram for helpful comments on an early draft of the manuscript.
Financial support
This project was supported by Grant number 09–063088 from The Danish Council for Strategic Research.
Declarations of conflicts of interest
The authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Skov, J., Bladbjerg, EM., Sidelmann, J. et al. Plenty of pills: polypharmacy prevails in patients of a Danish anticoagulant clinic. Eur J Clin Pharmacol 67, 1169–1174 (2011). https://doi.org/10.1007/s00228-011-1045-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-011-1045-0