Abstract
Objective
The human immundeficiency virus (HIV) protease inhibitor atazanavir is often used in once-daily observed therapy of methadone substituted former opiate drug users. We performed a matched-pairs analysis on 24 patients (12 men/women) taking atazanavir/ritonavir 300/100 mg daily plus reverse transcriptase inhibitors, with (n = 12) or without (n = 12) methadone co-administration.
Methods
Twenty-four-hour pharmacokinetic profiles of atazanavir/ritonavir were assessed at steady-state and measured by liquid chromatography–tandem mass spectrometry. The geometric mean (GM, t test) minimum and maximum plasma drug concentrations (Cmin, Cmax), area under the concentration–time curve (AUC), and total clearance (CLtotal) were compared between the groups of pairs, which were matched for age, sex, weight, and ethnicity.
Results
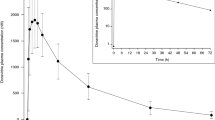
The GM [90% confidence interval (CI)] of the atazanavir Cmin, Cmax, and AUC of patients taking the methadone oral solution at doses of 20–175 mg/day simultaneously with antiretroviral therapy were impaired compared to patients not taking methadone oral solution: Cmin = 315 (range 197–448) vs. 519 (279–793) ng/mL [GM ratio (GMR) = 0.61, p = 0.229]; Cmax = 1714 (1238–2262) vs. 3190 (2412–4076) ng/mL (GMR = 0.54, p = 0.018); AUC = 21,987 (15,870–29,327) vs. 35,572 (26,211–46,728) ng h/mL (GMR = 0.62, p = 0.074). Methadone dose, which is proportional to the amount of methadone oral solution (10 mg/mL), was significantly correlated to atazanavir Cmax (r 2 = 0.40, p = 0.001) and AUC (r 2 = 0.32, p = 0.006). Ritonavir pharmacokinetics was similar between the groups with Cmin, Cmax, and AUC GMR of 1.01, 0.80, and 0.96, respectively.
Conclusion
The partial decrease in atazanavir plasma concentrations in patients concomitantly taking racemic methadone oral solution in this daily observed therapy setting deserves further attention, and therapeutic drug monitoring should be considered.


Similar content being viewed by others
References
Bristol Myers Squibb Company (2007) Reyataz product information. NDA 21-567/S-012. Bristol Meyers Squib, Princeton, NJ
CBER (1999) Guidance for the industry. In vivo drug metabolism/drug interactions studies. Study design, data analysis and recommendations for dosing and labeling. Center for Biologics Evaluation and Research (CBER), Rockville
Burger DM, Muller RJ, van der Leur MR, la Porte CJL (2002) Lopinavir plasma levels are significantly higher in female than in male HIV-1 infected patients. In: Program and abstracts of the 3rd Int Workshop Clinical Pharmacology of HIV Therapy. Washington D.C.
DiFrancesco R, Fischl MA, Donnelly J, Zingman BS, McCance-Katz EF, Moody DE, Reichman RC, Gripshover B, Morse GD (2007) Buprenorphine assay and plasma concentration monitoring in HIV-infected substance users. J Pharm Biomed Anal 44:188–195
Esser S, Staszewski S, Haberl A, Mulcahy F, Gölz J, Lazzarin A, Teofilo E, Vera J, Körber A, Ranneberg B, Gallo L (2008) 3OD—Once-daily (OD) TDF-containing HAART in HIV-1-infected former IVDU-patients receiving opiate substitution: efficacy, tolerability and adherence. In: 9th Int Congress Drug Therapy in HIV Infection. Glasgow
Esser S, Staszewski S, Haberl A, Mulcahy F, Gölz J, Lazzarin A, Teofilo E, Vera J, Körber A, Ranneberg B, Gallo L (2008) An open-label multicenter study to assess efficacy, tolerability and adherence of a once-daily (OD) TDF-Containing HAART in HIV-1-Infected Former IVDU-Patients receiving opiate substitution—final 48 weeks analysis of 3OD. In: 17th International AIDS Conference. Mexico City, Mexico
Friedland G, Andrews L, Schreibman T, Agarwala S, Daley L, Child M, Shi J, Wang Y, O'Mara E (2005) Lack of an effect of atazanavir on steady-state pharmacokinetics of methadone in patients chronically treated for opiate addiction. Aids 19:1635–1641
Gatti G, De Pascalis CR, De Luca A et al (2002) Predictors of amprenavir parameters of drug exposure in heavily pretreated HIV positive patients (abstract). In: Proc 6th Int Congress in Drug Therapy in HIV Infection. Glasgow, p 165
Hsyu PH, Lillibridge J, Daniels E, Kerr BM (2006) Pharmacokinetic interaction of nelfinavir and methadone in intravenous drug users. Biopharm Drug Dispos 27:61–68
Johnson V, Brun-Vezinet F, Clotet B, Conway B, Kuritzkes D, Pillay D, Schapiro J, Telenti A, Richman D (2005) Update of the drug resistance mutations in HIV-1: 2005. Topics HIV Med 13:125–131
Kurowski M, Sternfeld T, Sawyer A, Hill A, Mocklinghoff C (2003) Pharmacokinetic and tolerability profile of twice-daily saquinavir hard gelatin capsules and saquinavir soft gelatin capsules boosted with ritonavir in healthy volunteers. HIV Med 4:94–100
McCance-Katz EF, Moody DE, Morse GD, Ma Q, Difrancesco R, Friedland G, Pade P, Rainey PM (2007) Interaction between buprenorphine and atazanavir or atazanavir/ritonavir. Drug Alcohol Depend 91:269–278
Pai MP, Schriever CA, Diaz-Linares M, Novak RM, Rodvold KA (2004) Sex-related differences in the pharmacokinetics of once-daily saquinavir soft-gelatin capsules boosted with low-dose ritonavir in patients infected with human immunodeficiency virus type 1. Pharmacotherapy 24:592–599
Stephan C, Hentig N, Kourbeti I, Dauer B, Mosch M, Lutz T, Klauke S, Harder S, Kurowski M, Staszewski S (2004) Saquinavir drug exposure is not impaired by the boosted double protease inhibitor combination of lopinavir/ritonavir. Aids 18:503–508
Tossonian HK, Raffa JD, Grebely J, Trotter B, Viljoen M, Mead A, Khara M, McLean M, Duncan F, Fraser C, DeVlaming S, Conway B (2007) Methadone dosing strategies in HIV-infected injection drug users enrolled in a directly observed therapy program. J Acquir Immune Defic Syndr 45:324–327
Umeh O, Currier J (2006) Sex differences in the pharmacokinetics and toxicity of antiretroviral therapy. Expert Opin Drug Metab Toxicol 2:273–283
von Hentig N (2008) Atazanavir/ritonavir: a review of its use in HIV therapy. Drugs Today (Barc) 44:103–132
von Hentig N, Babacan E, Stephan C, Lennemann T, Knecht G, Carlebach A, Harder S, Staszewski S, Haberl A (2008) Pharmacokinetics of atazanavir/ritonavir in HIV-1 infected adult outpatients is not affected by gender-related cofactors. J Antimicrob Chemother 62:579–582
von Hentig N, Dauer B, Haberl A, Klauke S, Lutz T, Staszewski S, Harder S (2007) Tenofovir comedication does not impair the steady-state pharmacokinetics of ritonavir-boosted atazanavir in HIV-1-infected adults. Eur J Clin Pharmacol 63:935–940
Funding
This pharmacokinetic analysis was supported by internal funds.
Transparency declaration
None to declare
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haberl, A., Moesch, M., Nisius, G. et al. Atazanavir plasma concentrations are impaired in HIV-1-infected adults simultaneously taking a methadone oral solution in a once-daily observed therapy setting. Eur J Clin Pharmacol 66, 375–381 (2010). https://doi.org/10.1007/s00228-009-0767-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-009-0767-8