Abstract
Objective
This study evaluated the pharmacokinetics of isoniazid (INH) associated with optimal early bactericidal activity (EBA), defined as 90% of the maximum EBA (EBA90) and the influence of N-acetyltransferase-2 (NAT2) subtype on the ability of pulmonary tuberculosis (PTB) patients to reach the identified pharmacokinetic values after INH doses ranging from 0.2 to 10–12 mg/kg body weight.
Methods
INH serum concentrations and NAT2 subtype were determined during four studies of PTB patients in three of whom the EBA of INH was determined. The relationship of EBA to area under the curve (AUC) \({\left( {{\text{AUC}}_{{0 - \infty }} } \right)}\) and 2-h serum concentrations was examined by exponential regression and fitted curves estimated the \({\text{AUC}}_{{0 - \infty }} \) and 2-h serum concentrations at which EBA90 was reached.
Results
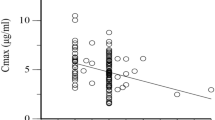
EBA90 was reached at an \({\text{AUC}}_{{0 - \infty }} \) of 10.52 μg/ml per hour and 2-h serum concentrations of 2.19 μg/ml. An \({\text{AUC}}_{{0 - \infty }} \) of 10.52 μg/ml per hour was reached by all 66 patients receiving a 10–12 mg/kg INH dose and all 21 receiving 6 mg/kg, except 1 of 10 (10%) homozygous fast (FF) acetylators; however, at 5 mg/kg, 4 of 12 (33%) FF and 26 of 27 (96%) heterozygous fast (FS), but all 21 homozygous slow (SS) acetylators did so; and 1 of 3 (33%) FF, 2 of 6 (33%) FS, but all 4 SS acetylators at dose 3 mg/kg. An INH 2-h serum concentration of 2.19 μg/ml was reached by all 66 patients receiving 10–12 mg/kg and all 21 receiving 6 mg/kg, except for 2 (20%) FF acetylators at a dose of 5 mg/kg; however, only 3 (25%) of 12 FF acetylators, but 26 (96%) of 27 FS acetylators, and all 21 SS acetylators reached this concentration; and at a dose of 3 mg/kg, 1 (33%) of 3 FF acetylators, 2 (33%) of 6 FF, but all 4 SS acetylators.
Conclusions
At a 6 mg/kg dose, all except a minority of FF NAT2 acetylators, achieve an INH \({\text{AUC}}_{{0 - \infty }} \) and 2-h INH serum concentrations associated with EBA90, as did all 4 SS acetylators receiving 3 mg/kg. Any dose reduction below 6 mg/kg body weight will tend to disadvantage a significant proportion of faster acetylators, but, conversely, SS acetylators require only a 3 mg/kg dose to achieve a satisfactory exposure to INH.


Similar content being viewed by others
References
Anonymous (1962) Isoniazid dosage. Tubercle 43:196–198
Bellman R (1983) Mathematical methods in medicine. Series in modern applied mathematics, vol 1. World Scientific, Singapore
Biehl JP (1957) Emergence of drug resistance as related to the dosage and metabolism of isoniazid. In: Transactions of 16th conference on the chemotherapy of tuberculosis. Veterans Administration Army Navy, Washington, DC, pp 108–113
Bönicke R, Reif W (1953) Enzymatische Inaktiviering von Isonikotinsaure hydrazide in menslichen und Tierschen Organismus. Arch Exp Pathol Pharmakol 220:321–333
Crofton J (1958) “Sputum conversion” and the metabolism of isoniazid. Am Rev Tuberc 77:869–871
Donald PR, Sirgel FA, Botha FJ et al (1997) The early bactericidal activity of isoniazid related to its dose size in pulmonary tuberculosis. Am J Respir Crit Care Med 156:895–900
Donald PR, Sirgel FA, Venter A et al (2001) Early bactericidal activity of amoxicillin in combination with clavulanic acid in patients with sputum smear-positive pulmonary tuberculosis. Scand J Infect Dis 33:466–469
Donald PR, Sirgel FA, Venter A et al (2002) The early bactericidal activity of streptomycin. Int J Tuberc Lung Dis 6:693–698
Donald PR, Sirgel FA, Venter A et al (2004) The influence of human N-acetyltransferase genotype on the early bactericidal activity of isoniazid. Clin Infect Dis 39:1425–1430
East African Hospitals/British Medical Research Council (1960) Comparative trial of isoniazid in combination with thiacetazone or a substituted diphenylthioures (SU1906) or PAS on the treatment of acute pulmonary tuberculosis in East Africa. Tubercle 41:399–423
East African/British Medical Research Council (1963) Isoniazid with thiacetazone in the treatment of pulmonary tuberculosis in East Africa. Second investigation. Tubercle 44:301–333
East African/British Medical Research Council (1966) Isoniazid with thiacetazone in the treatment of pulmonary tuberculosis in East Africa. Fourth investigation. Tubercle 47:315–339
Ellard G (1984) The potential clinical significance of isoniazid acetylator phenotype in the treatment of pulmonary tuberculosis. Tubercle 65:211–227
Elmendorf D, Cawthon WU, Muschenheim C, McDermott W (1952) The absorption, distribution, excretion and short-term toxicity of isonicotinic acid hydrazide (Nydrazid) in man. Am Rev Tuberc 429–442
Harris HW (1959) Report on study 16: high dosage INH. In: Transactions of the 18th conference on the chemotherapy of tuberculosis. Veterans Administration Army Navy, Washington, DC, pp 70–76
Hiratsuka M, Kishikawa Y, Takekuma Y et al (2002) Genotyping of the N-acetyltransferase 2 polymorphism in the prediction of adverse drug reactions to isoniazid in Japanese patients. Drug Metab Pharmacokinet 17:357–362
Hughes HB (1953) On the metabolic fate of isoniazid. J Pharmacol Exp Therap 109:444–454
Hughes HB, Biehl JP, Jones AP, Schmidt LH (1954) Metabolism of isoniazid in man as related to the occurrence of peripheral neuritis. Am Rev Tuberc 70:266–273
Jindani A, Aber VR, Edwards EA, Mitchison DA (1980) The early bactericidal activity of drugs in patients with pulmonary tuberculosis. Am Rev Respir Dis 121:939–949
Kinzig-Schippers M, Tomalik-Scharte D, Jetter A et al (2005) Should we use N-acetyltransferase type 2 genotyping to personalize isoniazid doses? Antimicrob Agents Chemother 49:1733–1738
Klee P (1952) Die Behandelung der Tuberkulose mit Neoteben (isonikotinsäuerhydrazid). Deutsche med Wchnschr 77:578–581
Miller SA, Dykes DD, Polesky HF (1988) A simple salting out procedure for extracting DNA from human nucleated cells. Nucl Acid Res 16:1215
Mitchell RS, Bell JC (1957) Clinical implications of isoniazid blood levels in pulmonary tuberculosis. New Eng J Med 257:1066–1070
Mitchison DA (1979) Basic mechanisms of chemotherapy. Chest 76(Suppl):771–781
Mitchison DA (1998) How drug resistance emerges as result of poor compliance during short course chemotherapy for tuberculosis. Int J Tuberc Lung Dis 2:10–15
Mount FW, Ferebee SH (1954) United States Public Health Service cooperative investigation of antimicrobial therapy of tuberculosis. Report on thirty-two-week observations on combinations of isoniazid, streptomycin and para-aminosalicylic acid. Am Rev Tuberc 70:521–526
Ohno M, Yamaguchi I, Yamamoto I et al (2000) Slow N-acetyltransferase 2 genotype affects the incidence of isoniazid and rifampicin-induced hepatotoxicity. Int J Tuberc Lung Dis 4:251–256
Parkin DP, Vandenplas S, Botha FJH et al (1997) Trimodality of isoniazid elimination. Phenotype and genotype in patients with tuberculosis. Am J Respir Crit Care Med 155:1717–1722
Peloquin CA, Nita AT, Burman WJ et al (1996) Low antituberculosis drug concentrations in patients with AIDS. Ann Pharmacother 30:919–925
R Development Core Team. R: 2006 A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0, URL http://www.R-project.org
Robitzek EH, Selikoff IJ (1952) Hydrazine derivatives of isonicotinic acid (Rimifon, Marsalid) in the treatment of active progressive caseous-pneumonic tuberculosis. Am Rev Tuberc 65:402–428
Russel WF, Kass I, Heaton AD, Dressler SH, Middlebrook G (1959) Combined drug treatment of tuberculosis. III Clinical application of the principles of appropriate and adequate chemotherapy to the treatment of pulmonary tuberculosis. J Clin Investigation 38:1366–1375
Seifart HI, Gent WI, Parkin DP, van Jaarsveld PP, Donald PR (1995) High-performance liquid chromatographic determination of isoniazid, acetylisoniazid and hydrazine in biological fluids. J Chromatogr [Br] 674:269–275
Selikoff IJ, Robitzek EH, Ornstein GG (1952) Treatment of pulmonary tuberculosis with hydrazine derivatives of isonicotinic acid. JAMA 150:973–980
Tuberculosis Chemotherapy Centre, Madras (1963) The prevention and treatment of isoniazid toxicity in the therapy of pulmonary tuberculosis. Bull Wld Hlth Org 38:455–475
Tuberculosis Chemotherapy Committee of the Medical Research Council (1953) Isoniazid in the treatment of pulmonary tuberculosis. Br Med J 1:521–536
Weiner M, Burman W, Vernon A et al (2003) Low isoniazid concentrations and outcome of tuberculosis treatment with once-weekly isoniazid and rifapentine. Am J Respir Crit Care Med 167:1341–1347
Weiner M, Benator D, Burman W et al (2005) Association between acquired rifamycin resistance and the pharmacokinetics of rifabutin and isoniazid among patients with HIV and tuberculosis. Clin Infect Dis 40:1481–1491
World Health Organization (2003) Standardized treatment regimen. In: Treatment of tuberculosis: guidelines for national programmes. WHO/CDS/TB/2003.313.Geneva. WHO.2003:37–38
Acknowledgement
Dr. Don Parkin died during the preparation of the manuscript. His co-authors would like to acknowledge the significant role he played in all of our studies of the pharmacology of isoniazid.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Donald, P.R., Parkin, D.P., Seifart, H.I. et al. The influence of dose and N-acetyltransferase-2 (NAT2) genotype and phenotype on the pharmacokinetics and pharmacodynamics of isoniazid. Eur J Clin Pharmacol 63, 633–639 (2007). https://doi.org/10.1007/s00228-007-0305-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-007-0305-5