Abstract
Objective
Landiolol hydrochloride is a new ultra-short-acting β1-adrenergic receptor blocking agent that is used for patients with tachycardia during general anesthesia. The hemodynamic response to a β-adrenergic receptor blocking agent is generally dependent on the subject. In the present investigation we investigated the effects of age and sex on the hemodynamic response to different doses of landiolol.
Methods
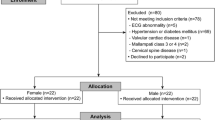
Following a persistence of tachycardia for more than 1 min, landiolol was infused at 0.03125, 0.0625 and 0.125 mg kg−1 min−1 for 1 min followed by 0.01, 0.02 and 0.04 mg kg−1min−1 for 10 min in groups L, M and H, respectively. Heart rate (HR), systolic (sBP) and diastolic blood pressure (dBP) were recorded each minute during the procedure. The respective changes were evaluated using logistic analysis with the equation \( Y{\left( t \right)} = {p + {\left( {q - p} \right)}} \mathord{\left/ {\vphantom {{p + {\left( {q - p} \right)}} {{\left[ {1 + \exp {\left\{ {{\left( {{4m} \mathord{\left/ {\vphantom {{4m} {{\left( {q - p} \right)}}}} \right. \kern-\nulldelimiterspace} {{\left( {q - p} \right)}}} \right)}{\left( {k - t} \right)}} \right\}}} \right]}}}} \right. \kern-\nulldelimiterspace} {{\left[ {1 + \exp {\left\{ {{\left( {{4m} \mathord{\left/ {\vphantom {{4m} {{\left( {q - p} \right)}}}} \right. \kern-\nulldelimiterspace} {{\left( {q - p} \right)}}} \right)}{\left( {k - t} \right)}} \right\}}} \right]}} \), where p, q, m and k indicate the upper asymptote, lower asymptote, maximum slope and time at the maximum slope.
Results
Parameters q and k for HR in group H were smaller than those in group L, whereas the parameters for sBP and dBP were unchanged among the three groups. Parameter q for HR in group H decreased with age of the patient. There was no significant difference in the landiolol-induced change in HR between males and females.
Conclusion
The hemodynamic response to landiolol is reliably modeled by the logistic function, especially in terms of HR. Landiolol causes a rapid and dose-dependent decrease in HR, whereas landiolol-induced changes in sBP and dBP are independent of dose. The landiolol-induced decrease in HR becomes larger with aging, but shows no sex difference. The logistic model may be useful for studying hemodynamic responses to landiolol based on age and sex differences, and may allow development of an improved monitoring system.
Implication statement
The logistic function reliably represents the hemodynamic responses to landiolol. Landiolol reduces HR rapidly and in a dose-dependentl manner whereas landiolol-induced changes in sBP and dBP are independent of dose. A larger decrease in HR is caused by landiolol in elderly patients, but there is no sex difference in the landiolol-induced change in HR.


Similar content being viewed by others
References
Biccard BM (2004) Peri-operative β-blockade and haemodynamic optimisation in patients with coronary artery disease and decreasing exercise capacity presenting for major noncardiac surgery. Anaesthesia 59:60–68
Mangano DT, Layug EL, Wallace A, Tateo I (1996) Effect of atenolol on mortality and cardiovascular morbidity after noncardiac surgery. Multicenter study of Perioperative Ischemia Research Group. N Engl J Med 335:1713–1720
Yuan L, Chia YY, Jan KT, Chen CS, Wang CH, Haung LH, Kang L (1994) The effect of single bolus dose of esmolol for controlling the tachycardia and hypertension during laryngoscopy and tracheal intubation. Acta Anaesthesiol Sin 32:147–152
Muraki K, Nakagawa H, Nagano N, Henmi S, Kawasumi H, Nakanishi T, Imaizumi K, Tokuno T, Atsuki K, Imaizumi Y, Watanabe M (1996) Effects of ONO-1101, a novel beta-antagonist, on action potential and membrane currents in cardiac muscle. J Pharmacol Exp Ther 278:555–563
Iguchi S, Iwamura H, Nishizaki M, Hayashi A, Senokuchi K, Kobayashi K, Sakaki K, Hachiya K, Ichioka Y, Kawamura M (1992) Development of a highly cardioselective ultra short-acting beta-blocker, ONO-1101. Chem Pharm Bull (Tokyo) 40:1462–1469
Goyagi T, Tanaka M, Nishikawa T (2005) Landiolol attenuates the cardiovascular response to tracheal intubation. J Anesth 19:282–286
Kitamura A, Sakamoto A, Inoue T, Ogawa R (1997) Efficacy of an ultrashort-acting beta-adrenoceptor blocker (ONO-1101) in attenuating cardiovascular responses to endotracheal intubation. Eur J Clin Pharmacol 51:467–471
Yamazaki A, Kinoshita H, Shimogai M, Fujii K, Nakahata K, Hironaka Y, Iranami H, Hatano Y (2005) Landiolol attenuates tachycardia in response to endotracheal intubation without affecting blood pressure. Can J Anaesth 52:254–257
Hirota K, Baba S, Fukushi S, Muraoka M, Matsuki A (2005) Efficacy of landiolol in attenuating hemodynamic responses to local epinephrine infiltration in patients undergoing vaginal total hysterectomy. J Anesth 19:17–20
Saito S, Nishihara F, Akihiro T, Nishikawa K, Obata H, Goto F, Yuki N (2005) Landiolol and esmolol prevent tachycardia without altering cerebral blood flow. Can J Anaesth 52:1027–1034
Sakamoto A, Ogawa R, Suzuki H, Kimura M, Okubo Y, Fujiya T (2004) Landiolol attenuates acute hemodynamic responses but does not reduce seizure duration during maintenance electroconvulsive therapy. Psychiatry Clin Neurosci 58:630–635
Ogata J, Yokoyama T, Okamoto T, Minami K (2003) Managing a tachyarrhythmia in a patient with pheochromocytoma with landiolol, a novel ultrashort-acting beta-adrenergic blocker. Anesth Analg 97:294–295
Ogata J, Okamoto T, Minami K (2003) Landiolol for the treatment of tachyarrhythmia associated with atrial fibrillation. Can J Anaesth 50:753
Yoshida Y, Hongo T, Sakamoto A, Ogawa R (2005) Successful management of tachycardiac atrial fibrillation in a septic patient with landiolol. Anesth Analg 100:294
Atarashi H, Kuruma A, Yashima M, Saitoh H, Ino T, Endoh Y, Hayakawa H (2000) Pharmacokinetics of landiolol hydrochloride, a new ultra-short-acting beta-blocker, in patients with cardiac arrhythmias. Clin Pharmacol Ther 68:143–150
Luzier AB, Killian A, Wilton JH, Wilson MF, Forrest A, Kazierad DJ (1999) Gender-related effects on metoprolol pharmacokinetics and pharmacodynamics in healthy volunteers. Clin Pharmacol Ther 66:594–601
Wilson DL (1994) The analysis of survival (mortality) data: fitting Gompertz, Weibull, and logistic functions. Mech Ageing Dev 74:15–33
Fujikawa H, Morozumi S (2005) Modeling surface growth of Escherichia coli on agar plates. Appl Environ Microbiol 71:7920–7926
Sabanathan K, Castleden CM, Adam HK, Ryan J, Fitzsimons TJ (1987) A comparative study of the pharmacokinetics and pharmacodynamics of atenolol, hydrochlorothiazide and amiloride in normal young and elderly subjects and elderly hypertensive patients. Eur J Clin Pharmacol 32:53–60
Scott M, Castleden CM, Adam HK, Smith RP, Fitzsimons TJ (1988) The effect of ageing on the disposition of nifedipine and atenolol. Br J Clin Pharmacol 25:289–296
Thompson DS, Waldron CB, Coltart DJ, Jenkins BS, Webb-Peploe MM (1983) Estimation of time constant of left ventricular relaxation. Br Heart J 49:250–258
Snedecor GW, Cochran WG (1971) Statistical methods, 6th edn. Iowa State Univ Press, Ames, Iowa
Colin P, Ghaleh B, Monnet X, Hittinger L, Berdeaux A (2004) Effect of graded heart rate reduction with ivabradine on myocardial oxygen consumption and diastolic time in exercising dogs. J Pharmacol Exp Ther 308:236–420
Warltier DC, Pagel PS, Kersten JR (2000) Approaches to the prevention of perioperative myocardial ischemia. Anesthesiology 92:253–259
Slogoff S, Keats AS (1985) Does perioperative myocardial ischemia lead to postoperative myocardial infarction? Anesthesiology 62:107–114
Oda Y, Nishikawa K, Hase I, Asada A (2005) The short-acting β1-adrenoceptor antagonists esmolol and landiolol suppress the bispectral index response to tracheal intubation during sevoflurane anesthesia. Anesth Analg 100:733–737
Sasao J, Tarver SD, Kindscher JD, Taneyama C, Benson KT, Goto H (2001) In rabbits, landiolol, a new ultra-short-acting beta-blocker, exerts a more potent negative chronotropic effect and less effect on blood pressure than esmolol. Can J Anaesth 48:985–989
Sugiyama A, Takahara A, Hashimoto K (1999) Electrophysiologic, cardiohemodynamic and beta-blocking actions of a new ultra-short-acting beta-blocker, ONO-1101, assessed by the in vivo canine model in comparison with esmolol. J Cardiovasc Pharmacol 34:70–77
Takahashi S, Fujii Y, Hoshi T, Uemura A, Miyabe M, Toyooka H (2003) Milrinone attenuates the negative inotropic effects of landiolol in halothane-anesthetized dogs. Can J Anaesth 50:830–834
Nakashima M, Kanamaru M (1997) Phase I study of ONO-1101, a new ultra short acting β1-blocking agent in healthy volunteers (in Japanese). Rinsho Iyaku 13:4823–4850
Sum CY, Yacobi A, Kartzinel R, Stampfli H, Davis CS, Lai CM (1983) Kinetics of esmolol, an ultra-short-acting beta blocker, and of its major metabolite. Clin Pharmacol Ther 34:427–434
Takahashi S, Fujii Y, Hoshi T, Inomata S, Miyabe M, Toyooka H (2000) Modifications of the hemodynamic consequences of theophylline intoxication with landiolol in halothane-anesthetized dogs. Can J Anaesth 47:265–272
Stadnicka A, Flynn NM, Bosnjak ZJ, Kampine JP (1993) Enflurane, halothane, and isoflurane attenuate contractile responses to exogenous and endogenous norepinephrine in isolated small mesenteric veins of the rabbit. Anesthesiology 78:326–334
Julius S (1992) Assessment of autonomic nervous function in human hypertension. Curr Opin Nephrol Hypertens 1:299–305
Minto CF, Schnider TW, Egan TD, Youngs E, Lemmens HJ, Gambus PL, Billard V, Hoke JF, Moore KH, Hermann DJ, Muir KT, Mandema JW, Shafer SL (1997) Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology 86:10–23
Schnider TW, Minto CF, Shafer SL, Gambus PL, Andresen C, Goodale DB, Youngs EJ (1999) The influence of age on propofol pharmacodynamics. Anesthesiology 90:1502–1516
Scott JC, Stanski DR (1987) Decreased fentanyl and alfentanil dose requirements with age. A simultaneous pharmacokinetic and pharmacodynamic evaluation. J Pharmacol Exp Ther 240:159–166
Chandler MP, DiCarlo SE (1998) Acute exercise and gender alter cardiac autonomic tonus differently in hypertensive and normotensive rats. Am J Physiol 274:R510–R516
Mier CM, Domenick MA, Wilmore JH (1997) Changes in stroke volume with beta-blockade before and after 10 days of exercise training in men and women. J Appl Physiol 83:1660–1665
Sugimoto SI, Takenaka K, Hirano K, Miyake Y, Imaizumi T (1998) Analysis of blood pressure responses during exercise by logistic function curve in hypertension: effects of age, gender and physical training. Acta Physiol Scand 163:17–24
Christenfeld N, Glynn LM, Gerin W (2000) On the reliable assessment of cardiovascular recovery: an application of curve-fitting techniques. Psychophysiology 37:543–550
Head GA, Reid CM, Lukoshkova EV (2005) Nonsymmetrical double logistic analysis of ambulatory blood pressure recordings. J Appl Physiol 98:1511–1518
Wilkinson PL, Stowe DF, Glantz SA, Tyberg JV (1980) Heart rate-systemic blood pressure relationship in dogs during halothane anesthesia. Acta Anaesthesiol Scand 24:181–186
Leitch JW, Newling R, Nyman E, Cox K, Dear K (1997) Limited utility of the phenylephrine-nitroprusside sigmoid curve method of measuring baroreflex function after myocardial infarction. J Cardiovasc Risk 4:179–184
Vuyk J, Engbers FH, Burm AG, Vletter AA, Griever GE, Olofsen E, Bovill JG (1996) Pharmacodynamic interaction between propofol and alfentanil when given for induction of anesthesia. Anesthesiology 84:288–299
Calhoun DA, Zhu S (1999) Pretreatment with enalaprilat blunts nicardipine-induced sympathetic activation in spontaneously hypertensive and Wistar-Kyoto rats. J Hypertens 17:507–512
Acknowledgements
We would like to thank Ono Pharmaceutical Co Ltd, Osaka, Japan and Mr. Shinichi Kikawa for excellent advice and support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mizuno, J., Yoshiya, I., Yokoyama, T. et al. Age and sex-related differences in dose-dependent hemodynamic response to landiolol hydrochloride during general anesthesia. Eur J Clin Pharmacol 63, 243–252 (2007). https://doi.org/10.1007/s00228-006-0249-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-006-0249-1