Abstract
Objectives
The aims of this study were to identify and evaluate the frequency of drugs involved in adverse drug reactions (ADRs) for which recommendations of the Summary of Product Characteristics (SPC) had not been respected and to compare the percentages of drugs suspected of being the cause of ADRs when correctly and incorrectly used.
Methods
All ADRs reported to the Regional Pharmacovigilance Centre of Tours (RPC) over a period of 5 months were analysed to identify drugs used “incorrectly” defined by drug use beyond the recommendations of the SPC, i.e. drugs used when contra-indicated and/or drugs used for an off-label indication, and/or drugs used at an inappropriate dose, and/or inappropriate duration of treatment, and/or drugs used in the presence of a potentially or definitely interacting drug.
Results
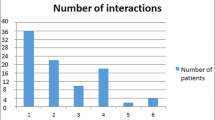
Included in the study were 182 ADRs involving 182 patients. Of 642 drugs, 169 (26%) were incorrectly used and for 81 patients (44.5%) ADRs involved at least one “incorrectly” used drug. These included 10% (64 of 642) drug interactions, 7.3% (47 of 642) off-licence indications, 5% (32 of 642) inadequate dosage, 3% (20 of 642) incorrect duration of treatment and 1% (6 of 642) contraindications. “Correctly” used drugs appeared to be less often the cause of the ADRs than “incorrectly” used drugs (59.4% versus 75%, P=0.0001).
Conclusion
“Incorrectly” used drugs were more often causally linked to ADR than correctly used drugs. A meaningful number of ADRs could probably be avoided if SPC guidelines for a safe and effective drug use are carefully adhered to.
Similar content being viewed by others
Notes
The summary of product characteristics on which the marketing authorisation is based should include: clinical indications, contraindications, adverse effects (frequency and seriousness), special precautions for use, recommendations on use in pregnancy, recommendations on use in lactation, interactions, dosage schedule and route of administration (discriminating between children, adults and the elderly), special warnings, any effects on the ability to drive or use machines and pharmaceutical incompatibilities
A serious adverse event or reaction is any untoward medical occurrence that at any dose:
-
Results in death
-
Requires inpatient hospitalisation or prolongation of existing hospitalisation
-
Results in persistent or significant disability/incapacity
-
Is life threatening
-
In the French method of imputability, the score is not continuous. The scores are:
-
Very probable (or certain for the Uppsala Monitoring Centre): a clinical event occurring in a plausible time relative to drug administration and which cannot be explained by concurrent disease. The response to withdrawal of the drug (dechallenge) should be clinically plausible, with a satisfactory rechallenge procedure if necessary.
-
Probable (or probable/likely for the Uppsala Monitoring Centre): a clinical event with a reasonable time sequence to administration of the drug, unlikely to be attributed to concurrent disease, and which follows a clinically reasonable response on withdrawal (dechallenge).
-
Possible (or possible for the Uppsala Monitoring Centre): a clinical event, with a reasonable time sequence to administrations of the drug, but which could also be explained by concurrent disease. Information on drug withdrawal may be lacking or unclear.
-
Doubtful (or unlikely for the Uppsala Monitoring Centre): a clinical event with a temporal relationship to drug administration which makes a causal relationship improbable, and in which underlying disease provides plausible explanations.
-
Yates F (1934) Contingency tables involving small numbers and the chi-square test. Journal of the Royal Statistical Society 1, Supplement, 217–235
“off label” = use of a medicine in a manner different from that recommended by the manufacturers in their product license: use in a different indication, dose, age, route or contraindication.
“unlicensed” = modifications to a licensed medicine; particular formulations (usually a suspension) manufactured under a “special” manufacturing license (such a medicine, although produced under the standards of good manufacturing practice, has not formally been tested in clinical trials); medicine used prior to the granting of a license and imported medicine.
Confidence interval at 95%
References
Bégaud B, Evreux JC, Jouglard J, Lagier G (1985) Imputabilité des effets inattendus ou toxiques des médicaments. Actualisation de la méthode utilisée en France. Therapie 40:111–118
Pouyanne P, Haramburu F, Imbs JL, Bégaud B (2000) Admissions to hospital caused by adverse drug reactions: cross sectional incidence study. BMJ 320:1036
Imbs JL, Pouyanne P, Haramburu F, Welsch M, Decker N, Blayac JP et al (1999) et le réseau des Centres régionaux de Pharmacovigilance (CRPV) Iatrogénie médicamenteuse: estimation de sa prévalence dans les hôpitaux publics français. Therapie 54:21–27
Lacost-Roussillon C, Pouyanne P, Haramburu F, Miremont G, Begaud B (2001) Incidence of serious adverse drug reactions in general practice: a prospective study. Clin Pharmacol Ther 69:458–462
Pearson TF, Pittman DG, Longley JM, Grapes ZT, Vigliotti DJ, Mullis SR (1994) Factors associated with preventable adverse drug reactions. Am J Hosp Pharm 51:2268–2272
Schumock GT, Thornton JP (1992) Focusing on preventability of adverse drug reactions. Hosp Pharm 27:538
Roughead EE, Gilbert LA, Primrose GJ, Sansom NL (1998) Drug-related hospital admissions: a review of Australian studies published 1988–1996. Med J Aust 168:405–408
Goettler M, Schneeweiss S, Hasford J (1997) Adverse drug reaction monitoring—cost and benefit considerations part II: cost and preventability of adverse drug reactions leading to hospital admission. Pharmacoepidemiol Drug Saf 6(Suppl 3):79–90
Lagnaoui R, Moore N, Fach J, Longy-Boursier M, Begaud B (2000) Adverse drug reactions in a department of systemic diseases-oriented internal medicine: prevalence, incidence, direct costs and avoidability. Eur J Clin Pharmacol 55:181–186
Olivier P, Boulbès O, Tubery M, Carles P, Montastruc JL, Lapeyre-Mestre M (2001) Evitabilité des effets indésirables dans un service d’admissions médicales. Therapie 56:275–278
Horen B, Montastruc JL, Lapeyre-Mestre M (2002) Adverse drug reactions and off-label drug use in paediatric outpatients. Br J Clin Pharmacol 54:665–670
Olivier P, Boulbes O, Tubery M (2002) Assessing the feasibility of using an adverse drug reaction preventability scale in clinical practice. Drug Saf 25:1035–1044
Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ et al (2004) Adverse drug reactions as cause of admission to hospital: prospective analysis of 18,820 patients. BMJ 329:15–19
Imbs JL, Pletan Y, Spriet A et les membres de la table ronde n°2 de Giens XIII (1998) Evaluation de la iatrogénèse médicamenteuse évitable: méthodologie. Therapie 53:365–370
Thomas EJ, Brennan TA (2000) Incidence and types of preventable adverse events in elderly patients: population based review of medical records. BMJ 320:741–744
Gurwitz JH, Field TS, Avorn J, McCormick D, Jain S, Eckler M et al (2000) Incidence and preventability of adverse drug events in nursing homes. Am J Med 109:87–94
Jankel AC, Fitterman KL (1993) Epidemiology of drug–drug interactions as a cause of hospital admissions. Drug Saf 9:51–59
Jankel AC, Speedie MS (1990) Detecting drug interactions: a review of the literature. DICP, Ann Pharmacother 24:982–989
Albaladejo P, Caillet B, Moine P, Vigué B, Decorps-Declère A, Benhamou D (2001) Prescription hors autorisation de mise sur le marché en réanimation chirurgicale adulte. Presse Med 30:1484–1488
Brosgart CL, Mitchell T, Charlebois E, Coleman R, Mehalko S, Young J, et al (1996) Off-label drug use in human immunodeficiency virus disease. J Acquir Immune Defic Syndr 12:56–62
Rayburn WF, Turnbull GL (1995) Off-label drug prescribing on a state university obstetric service. J Reprod Med 40:186–188
Poole SG, Dooley MG (2004) Off-label prescribing in oncology. Support Care Cancer 12:302–3055
Choonara I, Conroy S (2002) Unlicensed and off-label drug use in children—implications for safety. Drug Saf 25:1–5
Turner S, Nunn AJ, Fielding K, Choonara I (1999) Adverse drug reactions to unlicensed and off-label drugs on paediatric wards: a prospective study. Acta Paediatr 88:965–968
Gill AM, Leach HJ, Hughes J, Barker C, Nunn AJ, Choonara I (1995) Adverse drug reactions in a paediatric intensive care unit. Acta Paediatr 84:438–441
Clarkson A, Ingleby E, Choonara I, Bryan P, Arlett P (2001) A novel scheme for the reporting of adverse drugs reactions. Arch Dis Child 84:337–339
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jonville-Béra, A.P., Béra, F. & Autret-Leca, E. Are incorrectly used drugs more frequently involved in adverse drug reactions? A prospective study. Eur J Clin Pharmacol 61, 231–236 (2005). https://doi.org/10.1007/s00228-004-0881-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-004-0881-6