Abstract
Persistent symptoms after acute COVID-19 infection, termed post-COVID-19 fatigue, occur in 44–70% of patients. Characterizing fatigue in this population is vital to determine the etiology of post-COVID-19 fatigue symptoms and to assess the effectiveness of potential interventions. The purpose of this study was to assess differences in perceived and objective fatigability between people with post-COVID-19 symptoms (N = 29, 20 females) and people who had COVID-19 but are not experiencing persistent symptoms (N = 20, 12 females). Perceived fatigability, fatigue, pain, and quality of life were assessed with the Fatigue Severity Scale (FSS), Fatigue Assessment Scale (FAS), Visual Analog Scale for Pain (VAS), and the EQ-5D-5L, respectively. Objective fatigability was evaluated with torque and work fatigue indices (FI-T and FI-W), calculated via an isokinetic fatigue task. The results revealed that, the subjects with post-COVID-19 symptoms had significantly higher FAS (p < 0.01), FSS (p < 0.01), VAS (p < 0.01), and EQ-5D-5L VAS (p < 0.01) scores compared to subjects without post-COVID-19 symptoms, indicating greater fatigue and perceived fatigability, increased pain, and worse quality of life. However, there were no differences between the two groups for the FI-Ts (all p ≥ 0.07) or FI-W (all p ≥ 0.08), indicating no differences in objective fatigability. This study found that people with post-COVID-19 symptoms have increased fatigue and perceived fatigability, but not objective fatigability, compared to subjects without post-COVID-19 symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As of October 2022, over 96 million cases of coronavirus disease 2019 (COVID-19) have been documented in the United States (Centers for Disease Control and Prevention (CDC)). Despite the high (> 90%) survival rate of the acute illness, a proportion of patients continue to experience persistent symptoms (World Health Organization (WHO)). Importantly, post-COVID-19 condition is characterized as symptoms that last for at least two months after an acute COVID-19 illness (WHO). However, these symptoms have been reported to last over six months in some patients (Huang et al. 2021). Post-COVID-19 symptoms include anosmia, ageusia, myalgia, cognitive issues (e.g., memory or concentration), and, importantly, fatigue (WHO).
Persistent fatigue is one of the most common symptoms, occurring in 44–70% of patients, independent of the severity of the initial infection (i.e., hospitalized vs. non-hospitalized) (Huang et al. 2020; Wang et al. 2020; Xu et al. 2020; Schulze et al. 2022). Wijeratne et al. (Wijeratne and Crewther 2021) reported that, despite complete recovery after infection, 71–87% of people with COVID-19 report fatigue 2–3 months after initial infection. Interestingly, rates of persistent symptoms after COVID-19, particularly fatigue, have been thought to be higher in females than males (Bechmann et al. 2022; Ceban et al. 2022; Fernandez-de-Las-Penas et al. 2022). Although fatigue is a frequent and disabling symptom by people with various neurological disorders (e.g., multiple sclerosis (Krupp 2006) and Parkinson Disease (Friedman et al. 2007)), it remains not well understood, perhaps because there are several potential contributing factors (i.e., central, peripheral, and psychological factors) (Rudroff et al. 2020). In general, fatigue describes the feelings of tiredness, lack of energy, low motivation, and difficulty in concentrating and can only be measured by self-report (Enoka et al. 2021). Fatigability, on the other hand, is a measure of physical or cognitive work capacity. Specifically, perceived fatigability subjectively estimates past or future work capacity whereas objective fatigability determines the magnitude of the change in a performance metric after completing a prescribed task (Enoka et al. 2021).
There are several potential mechanisms underlying the persistent fatigue in people with post-COVID-19. Neurological dysfunctions as a result of viral encephalitis (Hoffman and Vilensky 2017), neuro-inflammation (Rogers et al. 2020; Nalbandian et al. 2021), hypoxia (Ceban et al. 2022), and cerebrovascular disease (Higgins et al. 2021; Komaroff and Lipkin 2021; Nalbandian et al. 2021) have been hypothesized. This is in line with studies on severe acute respiratory syndrome (SARS), another coronavirus, which showed persistent fatigue symptoms in survivors (Caldaria et al. 2020), potentially due to the virus invading tissues in the central and peripheral nervous systems (He et al. 2003; Glass et al. 2004). Therefore, it has been suggested that post-COVID-19 may be a neurological disorder due to the overlap in symptoms and underlying mechanisms. However, studies linking pathophysiological findings with post-COVID-19 symptoms are scarce. Douaud et al. (2022) investigated brain changes pre- and post-COVID-19 and found increased markers of tissue damage and a reduction in gray matter thickness, global brain size, and performance on cognitive tasks in people who became infected with COVID-19 (Douaud et al. 2022). Similarly, Guedj et al. (2021) demonstrated that bilateral hypo-metabolism in various brain regions was significantly associated with post-COVID-19 symptoms, including cognitive impairment, pain, and insomnia (Guedj et al. 2021). On the other hand, other studies found that neurological deficits or significant MRI abnormalities were rarely objectified in people with post-COVID-19 and, if present, could be attributed to other neurological disorders in most cases (Fleischer et al. 2022; Kachaner et al. 2022). In line with this, Dressing et al. (2022) demonstrated no significant changes in cerebral glucose metabolism in post-COVID-19 subjects with self-reported cognitive impairment and fatigue (Dressing et al. 2022).
Most studies that aimed to characterize symptoms in people with post-COVID-19 symptoms used self-report questionnaires to evaluate fatigue and/or perceived fatigability, but no studies have assessed objectively determined performance fatigability. However, comparing these domains of fatigue is vital to determine the etiology of post-COVID-19 fatigue symptoms and to assess the effectiveness of potential interventions. This is important because perceived fatigability is often distinct and independent from objective fatigability. Specifically, it has been suggested that these domains of fatigue are not correlated or only have a moderate association in most conditions (DeLuca et al. 2008; Kluger et al. 2013). For example, in people with multiple sclerosis, several studies have failed to demonstrate a consistent association between perceived fatigability and behavioral performance (Jennekens-Schinkel et al. 1988; Johnson et al. 1997; Beatty et al. 2003; Genova et al. 2013). Moreover, it is theorized that some clinical population may be able to perform a task as well as healthy controls (i.e., same objective fatigability), but they perceive the task as more difficult (i.e., increased perceived fatigability) (DeLuca et al. 2008; Kohl et al. 2009).
The primary aim of this study was to characterize fatigue in people with post-COVID-19 symptoms. Specifically, we assessed differences in fatigue as well as perceived and objective fatigability between people with post-COVID-19 symptoms and people who had COVID-19, but are not experiencing persistent symptoms (i.e., people without post-COVID-19 symptoms). We hypothesized that people with post-COVID-19 symptoms would have greater fatigue and perceived fatigability, according to self-report questionnaires, but not objective, performance fatigability, as assessed by fatigue tests, compared to subjects without post-COVID-19 symptoms.
Methods
Subjects
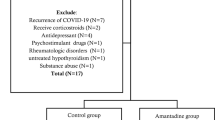
29 subjects (20 females) with post-COVID-19 and 20 (12 females) subjects without post-COVID-19 symptoms (people who had a confirmed diagnosis of COVID-19 but are not experiencing persistent symptoms) were recruited from the University of Iowa Hospitals and Clinics via mass email to university students, staff, faculty, and alumni between January 2021 and June 2022. Only patients who meet CDC guidelines for discontinuation of home isolation were recruited. Subject characteristics are displayed in Table 1. Inclusion criteria were: (1) between the ages of 18–80 years old, (2) previous positive COVID-19 test (confirmed via medical record), (3) at least 6 weeks post quarantine, (3) experiencing or not experiencing post-COVID-19 symptoms (depending on group assignment), based on the Chalder Fatigue Scale CFQ-11 score (post-COVID-19 fatigue ≥ 5 (Chalder et al. 1993)) and the COVID-19 Yorkshire Rehab Screen (C19-YRS) (O'Connor et al. 2022), (4) have no current or past medical conditions that would make the completing the protocol dangerous for the subject, (5) demonstrated an understanding of the study protocol during screening phone call, and (6) fluent in English. Exclusion criteria included: (1) the presence of any medical conditions that are contraindications to exercising training (e.g., major renal, pulmonary, hepatic, or cardiovascular disorders), (2) being diagnosed with any condition that may exacerbate fatigue (e.g., anemia, hypothyroidism, B12 deficiency, major sleep disorder, major depressive disorder, stress, anxiety), (3) history of significant traumatic brain injury or hydrocephalus, or 4) pregnancy. This study was approved by the Institutional Review Board at the University of Iowa (IRB #202,009,381) and was performed in accordance with the Declaration of Helsinki.
Experimental protocol
Subjects completed one experimental session to assess fatigue as well as perceived and objectively determined fatigability. During this session, subjects were consented, then completed questionnaires to assess their fatigue and perceived fatigability, followed by an isokinetic fatigue test.
Measurements
Fatigue, perceived fatigability, pain, and quality of life assessments
The Fatigue Assessment Scale (FAS) contains 10 statements to evaluate fatigue (Michielsen et al. 2003). Subjects rated each statement on a 5-point scale (1 = “never”–5 = “always”), depending on how appropriate they felt the statement applied to them. A low value indicates that the statement does not apply to them, whereas a high value indicates high agreement with the statement. The scores from the statements are summed, with statements 4 and 10 “reverse-scored.” Total scores range from 10 (lowest level of fatigue) to 50 (highest level of fatigue).
The Fatigue Severity Scale (FSS) contains nine statements to assess perceived fatigability (Krupp et al. 1989; Enoka et al. 2021). Subjects rated each statement on a 7-point scale, depending on how appropriate they felt the statement applied to them over the preceding week. A low value indicates that the statement does not apply to them, whereas a high value indicates high agreement with the statement. This questionnaire is scored by calculating the average response to the statements. A score ≥ 4 indicates a clinically significant level of fatigue severity and a change of 0.5–0.89 points is considered the minimally clinically important difference (Rooney et al. 2019).
The Visual Analog Scale for Pain (VAS) asks subjects to indicate on a scale from 0 (no pain) to 100 (pain as bad as it could be) how much pain, on average, they experienced over the past 24 h.
EQ-5D-5L questionnaire assesses quality of life on a 5-component scale including mobility, self-care, usual activities, pain/discomfort, and anxiety/depression (Janssen et al. 2013). Subjects rated each component by indicating which statement best describes the degree of problems that they are experiencing in that area (e.g., “I have no problems walking” to “I am unable to walk”). Subjects are then asked to rate their current overall health on a scale from 0 (worst health imaginable) to 100 (best health imaginable).
Objective fatigability assessments
The isokinetic fatigue test consisted of 40 consecutive maximal effort contractions of the knee extensors and flexors (120°/s, concentric/concentric) performed on an isokinetic dynamometer (HUMAC NORM, CSMi, Stoughton, MA). Prior to the fatigue test, subjects completed a 10-repetition warm-up (60°/s, concentric/concentric). The right leg fatigue test was performed first, followed by the left leg. Visual (i.e., per rep work bars) and verbal encouragement was provided to ensure a maximal effort performance from the subjects. Peak torque and total work for each repetition were retained for analysis. The first two repetitions of the fatigue task were considered adaptions and removed from subsequent analyses. Two fatigue indices were calculated: a torque-derived fatigue index (FI-T) and a work-derived fatigue index (FI-W). The peak torque from each repetition was used to calculate the FI-T as follows: ([mean of first five repetitions–mean of last five repetitions]/mean of first five repetitions) × 100 (Lambert et al. 2001; Workman et al. 2020b). A high FI-T indicates increased fatigability, as the subject was not able to produce a similar torque during the first and last five repetitions. The total work from each repetition was used to calculate the FI-W as follows: (total work performed in last half of the fatigue task/total work performed in the first half of the fatigue task) × 100 (Janssen et al. 2013; Rooney et al. 2019). A low FI-W indicates increased fatigability, as the subject was unable to produce a similar amount of work in the second half of the fatigue test as compared to the first half.
Statistical analysis
Unpaired t tests were used to evaluate differences between the people with and without post-COVID-19 symptoms on each outcome variable. Normality and linearity assumptions for the t tests were investigated via histograms, skewness and kurtosis statistics, and Q–Q plots of the residuals of the outcome variables. One-way ANOVAs were used to assess sex differences between the subgroups, stratified by sex and fatigue status (females with post-COVID-19 symptoms, females without post-COVID-19 symptoms, males with post-COVID-19 symptoms, and males without post-COVID-19 symptoms). Normality and homogeneity assumptions for the ANOVA were assessed with Q–Q plots and Levene’s test for Homogeneity of Variances, respectively. Cohen’s d was calculated to clarify any significant differences. Significance was accepted at p ≤ 0.05, after a Tukey correction, and analyses were performed using GraphPad Prism 9 (GraphPad Software, San Diego, CA, USA).
Results
All subjects completed all experimental tasks. Table 1 shows the subject characteristics. Data are reported as mean ± SD in the text and mean ± SEM in the figures.
The results of the unpaired t tests revealed that, the subjects with post-COVID-19 symptoms had significantly higher FAS (Without Post-COVID-19 symptoms: 15.10 ± 4.02, with post-COVID-19 symptoms: 28.35 ± 7.70, p < 0.01, d = 2.16, Fig. 1A) and FSS scores compared to subjects without post-COVID-19 symptoms (Without Post-COVID-19 symptoms: 2.06 ± 0.57, with post-COVID-19 symptoms: 4.71 ± 1.41, p < 0.01, d = 2.46, Fig. 1B), indicating increased fatigue and perceived fatigability.
A Fatigue Assessment Scale (FAS) scores stratified by group (With post-COVID-19 symptoms vs. without Post-COVID-19 symptoms). Females are shown in red while males are shown in blue. *Indicates significantly increased fatigue in the post-COVID-19 group (p < 0.01). B Fatigue Severity Scale (FSS) scores stratified by group (With post-COVID-19 symptoms vs. without Post-COVID-19 symptoms). Females are shown in red while males are shown in blue. *Indicates significantly increased fatigue in the subjects with post-COVID-19 symptoms (p < 0.01)
The subjects with post-COVID-19 symptoms also reported higher pain compared to the people without post-COVID-19 symptoms, according to their VAS scores (Without Post-COVID-19 symptoms: 4.30 ± 11.46, with post-COVID-19 symptoms: 25.34 ± 21.42, p < 0.01, d = 1.22), and lower quality of life, as indicated by their EQ-5D-5L VAS scores (Without Post-COVID-19 symptoms: 86.08 ± 8.39, with post-COVID-19 symptoms: 68.90 ± 18.43, p < 0.01, d = 1.20, Fig. 2).
The Visual Analog Scale for quality of life (EQ-5D-5L VAS) scores stratified by group (With post-COVID-19 symptoms vs. without Post-COVID-19 symptoms). Females are shown in red while males are shown in blue. *Indicates significantly lower quality of life in the subjects with post-COVID-19 symptoms (p < 0.01)
The results of the unpaired t tests for the FI-T of the right knee extensors (Without Post-COVID-19 symptoms: 59.71 ± 10.98, with post-COVID-19 symptoms: 59.51 ± 12.23, p = 0.95, d = 0.02, Fig. 3A) left knee extensors (Without Post-COVID-19 symptoms: 58.69 ± 10.50, with post-COVID-19 symptoms: 59.48 ± 12.10, p = 0.81, d = 0.07), right knee flexors (Without Post-COVID-19 symptoms: 40.89 ± 11.09, with post-COVID-19 symptoms: 44.59 ± 12.63, p = 0.30, d = 0.31), and left knee flexors (Without Post-COVID-19 symptoms: 42.93 ± 10.39, with post-COVID-19 symptoms: 35.95 ± 13.67, p = 0.07, d = 0.57) showed no significant differences in fatigability between subjects with and without post-COVID-19 symptoms. Similarly, the FI-W of the right knee extensors (Without Post-COVID-19 symptoms: 53.78 ± 9.30, with post-COVID-19 symptoms: 52.39 ± 10.88, p = 0.65, d = 0.14, Fig. 3B), left knee extensors (Without Post-COVID-19 symptoms: 57.88 ± 9.44, with post-COVID-19 symptoms: 55.99 ± 10.41, p = 0.52, d = 0.19), right knee flexors (Without Post-COVID-19 symptoms: 65.63 ± 8.61, with post-COVID-19 symptoms: 63.66 ± 10.41, p = 0.49, d = 0.21), and left knee flexors (Without Post-COVID-19 symptoms: 70.37 ± 9.68, with post-COVID-19 symptoms: 65.63 ± 7.96, p = 0.08, d = 0.53) revealed no significant differences between people with and without post-COVID-19 symptoms.
A Fatigue index derived from the torque data for the right knee extensors stratified by group (With post-COVID-19 symptoms vs. without Post-COVID-19 symptoms). Females are shown in red while males are shown in blue. There were no significant differences between the groups (p = 0.95). B Fatigue index derived from the work data for the right knee extensors stratified by group (With post-COVID-19 symptoms vs. without Post-COVID-19 symptoms). Females are shown in red while males are shown in blue. There were no significant differences between the groups (p = 0.65)
The results of the one-way ANOVAs for the FAS, FSS, VAS, and EQ-5D-5L revealed significant differences between subgroups (all F (3, 45) ≤ 22.01, p < 0.01). However, post hoc testing revealed no significant differences between females with post-COVID-19 symptoms and males with post-COVID-19 symptoms (all p ≥ 0.34) or females without post-COVID-19 symptoms and males without post-COVID-19 symptoms (all p = 0.93) for all of the questionnaires.
Discussion
To our knowledge, this is the first study to assess differences in fatigue as well as perceived and objectively fatigability in people with post-COVID-19 symptoms and people who had COVID-19 but are not experiencing post-COVID-19 persistent symptoms. The main findings were that subjects with post-COVID-19 symptoms reported higher levels of fatigue and perceived fatigability than subjects without post-COVID-19 symptoms, but there were no differences in objective fatigability between the groups. Furthermore, people with post-COVID-19 symptoms reported worse fatigue-related factors, such as increased pain and decreased quality of life, which has been demonstrated in other studies in people with post-COVID-19 symptoms (Haider et al. 2022; Peterson et al. 2022) and is common in other neurological disorders (e.g., multiple sclerosis and chronic fatigue syndrome) (Harrison et al. 2015; Heitmann et al. 2016; Workman et al. 2020a, 2020c). These findings support our hypothesis regarding perceived and objectively determined fatigability.
Discrepancies between fatigue as well as perceived and objective fatigability have been demonstrated in other patient populations, such as people with multiple sclerosis (PwMS). For example, DeLuca and colleagues indicated that these domains of fatigue are often not correlated or have no more than a moderate association in PwMS (DeLuca et al. 2008). Studies in PwMS and people with traumatic brain injuries (TBI) suggest that, although these clinical populations may be able to perform a task at comparable levels to healthy controls (i.e., same objective fatigability), their increased perception of fatigability may reflect an increase in the amount of cerebral resources needed to do so (DeLuca et al. 2008; Kohl et al. 2009). However, the pathophysiology of fatigue and perceived fatigability in people with post-COVID-19 remains vague. Previous studies have assessed structural damage to the central nervous system (CNS) using advanced MRI techniques, such as diffusion tensor imaging (DTI) in PwMS and failed to find a significant association between perceived fatigability and structural alterations (Codella et al. 2002a, 2002b). Similarly, recent studies in people with post-COVID-19 symptoms found no significant differences in MRI findings between subjects with and without cognitive impairments and fatigue after acute infection (Hellgren et al. 2021; Huang et al. 2022). Moreover, despite several studies detecting changes in brain microstructure of people with post-COVID-19 with structural MRI (Colonna et al. 2020; Freeman et al. 2021; Hixon et al. 2021; Nuzzo et al. 2021; Cecchini et al. 2022) and DTI (Liu et al. 2019; Tian et al. 2020; Qin et al. 2021), no correlations with fatigue symptoms have been reported. Other recent studies found that post-COVID-19 symptoms were rarely associated with damage of the central or peripheral nervous system (Fleischer et al. 2022) or alterations in regional cerebral glucose metabolism (Dressing et al. 2022). Moreover, the Fleischer and colleagues concluded that psychosomatic mechanisms, such as somato-sensoric amplification may play a role in the pathogenesis of post-COVID-19 symptoms (Fleischer et al. 2022).
As mentioned previously (Rudroff et al. 2020), fatigue and perceived fatigability also depend on other factors, such as mood, stress, pain, depression and anxiety. Specifically in people with post-COVID-19 symptoms, Calabria et al. (2022) found that increased levels of neuropsychiatric symptoms were important predictors of fatigue (Calabria et al. 2022), and a systematic review found that depression and anxiety was reported in 32% and 34% of subjects with post-COVID-19 symptoms, respectively (Jennings et al. 2021). However, Schulze and colleagues demonstrated that fatigue was not associated with symptoms of anxiety or depression in males and females with post-COVID-19 symptoms (Schulze et al. 2022). Moreover, Peterson et al. demonstrated that conditioned pain modulation was impaired in people who had symptomatic acute COVID-19 (Peterson et al. 2022) and Haider et al. found that pain levels in people with post-COVID-19 symptoms are comparable to people with fibromyalgia and chronic fatigue syndrome (Haider et al. 2022), which is line with the results of the current study. Additionally, it has been suggested that self-reporting post-COVID-19 symptoms may be influenced by one’s perception of the COVID-19 pandemic and apprehension about developing post-COVID-19 symptoms (Engelmann et al. 2022; Matta et al. 2022). Therefore, it is warranted that future research characterizes how psychosomatic factors contribute to the pathophysiology of post-COVID-19 fatigue.
Functional neuroimaging techniques to study fatigue, such as positron emission tomography with the glucose analog 18F-fluorodeoxyglucose (FDG-PET), may provide more information about the underlying mechanisms of post-COVID-19 fatigue symptoms. A review by Rudroff et al. (Rudroff et al. 2021) summarized studies in people with post-COVID-19 that showed FDG-PET hypo-metabolism in a variety of brain regions and associations with symptoms (Fleischer et al. 2022). For example, Guedj et al. (Guedj et al. 2021) found hypo-metabolism in the bilateral rectal/orbital gyrus (including the olfactory gyrus), hippocampus, temporal lobe (including the amygdala), bilateral pons/medulla brainstem, thalamus, and the bilateral cerebellum using FDG-PET in people with post-COVID-19 symptoms (Guedj et al. 2021). Importantly, this hypo-metabolism was associated with the patients’ symptoms (e.g., hyposmia/anosmia, cognitive impairment, pain and insomnia) (Guedj et al. 2021). Similarly, Sollini et al. (Sollini et al. 2021) demonstrated an association between brain hypo-metabolism in the thalamus as well as the right para-hippocampal gyrus and persistent symptoms (e.g., fatigue and anosmia/ageusia) in people with post-COVID-19 (Sollini et al. 2021). These findings are in line with the model fatigue suggested by Chaudhuri & Behan (Chaudhuri and Behan 2000), which hypothesized that perceived fatigue is associated with impairment of the non-motor functions within the basal ganglia, which in turn negatively impacts the striatal-thalamic-frontal cortical system (Chaudhuri and Behan 2000). Similarly, in PwMS, pathology of the striatum, thalamus, superior frontal gyrus and inferior parietal gyrus has been associated with increased levels of perceived fatigue (Roelcke et al. 1997; Tellez et al. 2008; Calabrese et al. 2010; Pardini et al. 2010). However, more work is needed to establish a fatigue network specific to people with post-COVID-19.
Interestingly, the results of the current study demonstrated no sex differences between women and men with post-COVID-19 symptoms, which contradicts previous studies. There are several contributing factors to potential sex differences in fatigue, pain, and quality of life including biological (e.g., levels of fluctuating hormones) and social (e.g., gender norms) (Bensing et al. 1999; Rudroff et al. 2022). These factors were not addressed by the questionnaires used to assess fatigue and perceived fatigability and, therefore, may not be sensitive enough to examine sex differences. Moreover, the sample size in current study may not be large enough to determine sex differences, although they may have affected the results.
Limitations and future studies
There are several limitations in this study. First, although there were no significant differences between the groups. There is a large variation in the time since COVID-19 diagnosis within each group. This is important because symptom severity may decrease as more time passes after acute illness (Sandler et al. 2021). Similarly, although there were no differences between the groups, there is a large age range of the subjects in each group, which may influence both perceived and objective fatigability. Additionally, the cohort of subjects in this study is young and the results may not generalize to older people with post-COVID-19 symptoms. Moreover, although potential subjects were excluded if they had a condition known to exacerbate fatigue, we did not assess additional factors that may influence fatigue, such as psychological stress or levels of anxiety and depression. Lastly, a larger sample size may be needed to thoroughly evaluate sex differences in people with post-COVID-19 symptoms. No power calculation was performed and the study should be seen as a preliminary investigation, conducted with the aim of informing further research, not providing any definitive conclusions.
Future studies should further characterize and establish a clinical definition of fatigue and perceived fatigability in people with post-COVID-19 symptoms, which will allow for the development of reliable and valid approaches to diagnose these domains of fatigue in this patient population. These studies should assess other factors that may influence fatigue, such as levels of depression, stress, sleep quality, physical activity levels, pain, and anxiety as well as various factors that may contribute to the development of post-COVID-19 symptoms, including time since acute illness, the variant in which subjects were infected with, and vaccination status. Moreover, future studies should compare people who have not had COVID-19 in addition to people with and without post-COVID-19 symptoms. Importantly, future research should evaluate underlying physiological and psychological mechanisms of fatigue and perceived fatigability to determine risk factors for post-COVID-19 fatigue and evaluate the effectiveness of potential interventions. For example, determining alterations in glucose metabolism in the brain via FDG-PET may lead to the establishment of a “Post-COVID-19 Fatigue Network,” which may establish target structures for neurophysiological treatments.
Summary
This study found that people with post-COVID-19 symptoms have significantly increased fatigue and perceived fatigability, but not objective fatigability compared to people who had COVID-19, but are not experiencing post-COVID-19 persistent symptoms. However, more research with larger sample sizes is needed before any conclusions can be made. Furthermore, it is suggested that future research should take into account psychosomatic factors as possible triggers for post-COVID-19 fatigue. Moreover, there were no differences in perceived fatigability between males and females, which also requires further investigation. This research is highly significant, especially regarding treatment of symptoms and the development of assessments to distinguish between perceived and objective fatigability in people with post-COVID-19 fatigue.
Data availability
The data that support the findings of this study are available on request to the corresponding author.
References
Beatty WW, Goretti B, Siracusa G, Zipoli V, Portaccio E, Amato MP (2003) Changes in neuropsychological test performance over the workday in multiple sclerosis. Clin Neuropsychol 17:551–560. https://doi.org/10.1076/clin.17.4.551.27942
Bechmann N, Barthel A, Schedl A et al (2022) Sexual dimorphism in COVID-19: potential clinical and public health implications. Lancet Diabetes Endocrinol 10:221–230. https://doi.org/10.1016/S2213-8587(21)00346-6
Bensing JM, Hulsman RL, Schreurs KM (1999) Gender differences in fatigue: biopsychosocial factors relating to fatigue in men and women. Med Care 37:1078–1083. https://doi.org/10.1097/00005650-199910000-00011
Calabrese M, Mattisi I, Rinaldi F et al (2010) Magnetic resonance evidence of cerebellar cortical pathology in multiple sclerosis. J Neurol Neurosurg Psychiatry 81:401–404. https://doi.org/10.1136/jnnp.2009.177733
Calabria M, Garcia-Sanchez C, Grunden N et al (2022) Post-COVID-19 fatigue: the contribution of cognitive and neuropsychiatric symptoms. J Neurol 269:3990–3999. https://doi.org/10.1007/s00415-022-11141-8
Caldaria A, Conforti C, Di Meo N et al (2020) COVID-19 and SARS: differences and similarities. Dermatol Ther 33:e13395. https://doi.org/10.1111/dth.13395
Ceban F, Ling S, Lui LMW et al (2022) Fatigue and cognitive impairment in Post-COVID-19 Syndrome: a systematic review and meta-analysis. Brain Behav Immun 101:93–135. https://doi.org/10.1016/j.bbi.2021.12.020
Cecchini MP, Brozzetti L, Cardobi N et al (2022) Persistent chemosensory dysfunction in a young patient with mild COVID-19 with partial recovery 15 months after the onset. Neurol Sci 43:99–104. https://doi.org/10.1007/s10072-021-05635-y
Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright D, Wallace EP (1993) Development of a fatigue scale. J Psychosom Res 37:147–153. https://doi.org/10.1016/0022-3999(93)90081-p
Chaudhuri A, Behan PO (2000) Fatigue and basal ganglia. J Neurol Sci 179:34–42. https://doi.org/10.1016/s0022-510x(00)00411-1
Codella M, Rocca MA, Colombo B, Martinelli-Boneschi F, Comi G, Filippi M (2002a) Cerebral grey matter pathology and fatigue in patients with multiple sclerosis: a preliminary study. J Neurol Sci 194:71–74. https://doi.org/10.1016/s0022-510x(01)00682-7
Codella M, Rocca MA, Colombo B, Rossi P, Comi G, Filippi M (2002b) A preliminary study of magnetization transfer and diffusion tensor MRI of multiple sclerosis patients with fatigue. J Neurol 249:535–537. https://doi.org/10.1007/s004150200060
Colonna S, Sciume L, Giarda F, Innocenti A, Beretta G, Dalla Costa D (2020) Case report: postacute rehabilitation of guillain-barre syndrome and cerebral vasculitis-like pattern accompanied by SARS-CoV-2 infection. Front Neurol 11:602554. https://doi.org/10.3389/fneur.2020.602554
DeLuca J, Genova HM, Hillary FG, Wylie G (2008) Neural correlates of cognitive fatigue in multiple sclerosis using functional MRI. J Neurol Sci 270:28–39. https://doi.org/10.1016/j.jns.2008.01.018
Douaud G, Lee S, Alfaro-Almagro F et al (2022) SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 604:697–707. https://doi.org/10.1038/s41586-022-04569-5
Dressing A, Bormann T, Blazhenets G et al (2022) Neuropsychologic profiles and cerebral glucose metabolism in neurocognitive long COVID syndrome. J Nucl Med 63:1058–1063. https://doi.org/10.2967/jnumed.121.262677
Engelmann P, Lowe B, Brehm TT et al (2022) Risk factors for worsening of somatic symptom burden in a prospective cohort during the COVID-19 pandemic. Front Psychol 13:1022203. https://doi.org/10.3389/fpsyg.2022.1022203
Enoka RM, Almuklass AM, Alenazy M, Alvarez E, Duchateau J (2021) Distinguishing between fatigue and fatigability in multiple sclerosis. Neurorehabil Neural Repair 35:960–973. https://doi.org/10.1177/15459683211046257
Fernandez-de-Las-Penas C, Martin-Guerrero JD, Pellicer-Valero OJ et al (2022) Female sex is a risk factor associated with long-term post-covid related-symptoms but not with COVID-19 symptoms: the LONG-COVID-EXP-CM multicenter study. J Clin Med. https://doi.org/10.3390/jcm11020413
Fleischer M, Szepanowski F, Tovar M et al (2022) Post-COVID-19 syndrome is rarely associated with damage of the nervous system: findings from a prospective observational cohort study in 171 patients. Neurol Ther. https://doi.org/10.1007/s40120-022-00395-z
Freeman CW, Masur J, Hassankhani A, Wolf RL, Levine JM, Mohan S (2021) Coronavirus Disease (COVID-19)-related disseminated leukoencephalopathy: a retrospective study of findings on brain MRI. AJR Am J Roentgenol 216:1046–1047. https://doi.org/10.2214/AJR.20.24364
Friedman JH, Brown RG, Comella C et al (2007) Fatigue in Parkinson’s disease: a review. Mov Disord 22:297–308. https://doi.org/10.1002/mds.21240
Genova HM, Rajagopalan V, Deluca J et al (2013) Examination of cognitive fatigue in multiple sclerosis using functional magnetic resonance imaging and diffusion tensor imaging. PLoS ONE 8:e78811. https://doi.org/10.1371/journal.pone.0078811
Glass WG, Subbarao K, Murphy B, Murphy PM (2004) Mechanisms of host defense following severe acute respiratory syndrome-coronavirus (SARS-CoV) pulmonary infection of mice. J Immunol 173:4030–4039. https://doi.org/10.4049/jimmunol.173.6.4030
Guedj E, Campion JY, Dudouet P et al (2021) (18)F-FDG brain PET hypometabolism in patients with long COVID. Eur J Nucl Med Mol Imaging 48:2823–2833. https://doi.org/10.1007/s00259-021-05215-4
Haider S, Janowski AJ, Lesnak JB et al (2022) A comparison of pain, fatigue, and function between post-COVID-19 condition, fibromyalgia, and chronic fatigue syndrome: a survey study. Pain. https://doi.org/10.1097/j.pain.0000000000002711
Harrison AM, McCracken LM, Bogosian A, Moss-Morris R (2015) Towards a better understanding of MS pain: a systematic review of potentially modifiable psychosocial factors. J Psychosom Res 78:12–24. https://doi.org/10.1016/j.jpsychores.2014.07.008
He L, Ding YQ, Che XY et al (2003) Expression of the monoclonal antibody against nucleocapsid antigen of SARS-associated coronavirus in autopsy tissues from SARS patients. Di Yi Jun Yi Da Xue Xue Bao 23:1128–1130
Heitmann H, Biberacher V, Tiemann L et al (2016) Prevalence of neuropathic pain in early multiple sclerosis. Mult Scler 22:1224–1230. https://doi.org/10.1177/1352458515613643
Hellgren L, Birberg Thornberg U, Samuelsson K, Levi R, Divanoglou A, Blystad I (2021) Brain MRI and neuropsychological findings at long-term follow-up after COVID-19 hospitalisation: an observational cohort study. BMJ Open 11:e055164. https://doi.org/10.1136/bmjopen-2021-055164
Higgins V, Sohaei D, Diamandis EP, Prassas I (2021) COVID-19: from an acute to chronic disease? Potential long-term health consequences. Crit Rev Clin Lab Sci 58:297–310. https://doi.org/10.1080/10408363.2020.1860895
Hixon AM, Thaker AA, Pelak VS (2021) Persistent visual dysfunction following posterior reversible encephalopathy syndrome due to COVID-19: Case series and literature review. Eur J Neurol 28:3289–3302. https://doi.org/10.1111/ene.14965
Hoffman LA, Vilensky JA (2017) Encephalitis lethargica: 100 years after the epidemic. Brain 140:2246–2251. https://doi.org/10.1093/brain/awx177
Huang C, Wang Y, Li X et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395:497–506. https://doi.org/10.1016/S0140-6736(20)30183-5
Huang C, Huang L, Wang Y et al (2021) 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 397:220–232. https://doi.org/10.1016/S0140-6736(20)32656-8
Huang Y, Ling Q, Manyande A, Wu D, Xiang B (2022) Brain Imaging Changes in Patients Recovered From COVID-19: A Narrative Review. Front Neurosci 16:855868. https://doi.org/10.3389/fnins.2022.855868
Janssen MF, Pickard AS, Golicki D et al (2013) Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res 22:1717–1727. https://doi.org/10.1007/s11136-012-0322-4
Jennekens-Schinkel A, Sanders EA, Lanser JB, Van der Velde EA (1988) Reaction time in ambulant multiple sclerosis patients. Part I. Influence of prolonged cognitive effort. J Neurol Sci 85:173–186. https://doi.org/10.1016/0022-510x(88)90154-2
Jennings G, Monaghan A, Xue F, Mockler D, Romero-Ortuno R (2021) A systematic review of persistent symptoms and residual abnormal functioning following acute ongoing symptomatic phase vs post-COVID-19 syndrome. J Clin Med. https://doi.org/10.3390/jcm10245913
Johnson SK, Lange G, DeLuca J, Korn LR, Natelson B (1997) The effects of fatigue on neuropsychological performance in patients with chronic fatigue syndrome, multiple sclerosis, and depression. Appl Neuropsychol 4:145–153. https://doi.org/10.1207/s15324826an0403_1
Kachaner A, Lemogne C, Dave J, Ranque B, de Broucker T, Meppiel E (2022) Somatic symptom disorder in patients with post-COVID-19 neurological symptoms: a preliminary report from the somatic study (Somatic Symptom Disorder Triggered by COVID-19). J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp-2021-327899
Kluger BM, Krupp LB, Enoka RM (2013) Fatigue and fatigability in neurologic illnesses: proposal for a unified taxonomy. Neurology 80:409–416. https://doi.org/10.1212/WNL.0b013e31827f07be
Kohl AD, Wylie GR, Genova HM, Hillary FG, Deluca J (2009) The neural correlates of cognitive fatigue in traumatic brain injury using functional MRI. Brain Inj 23:420–432. https://doi.org/10.1080/02699050902788519
Komaroff AL, Lipkin WI (2021) Insights from myalgic encephalomyelitis/chronic fatigue syndrome may help unravel the pathogenesis of postacute COVID-19 syndrome. Trends Mol Med 27:895–906. https://doi.org/10.1016/j.molmed.2021.06.002
Krupp L (2006) Fatigue is intrinsic to multiple sclerosis (MS) and is the most commonly reported symptom of the disease. Mult Scler 12:367–368. https://doi.org/10.1191/135248506ms1373ed
Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD (1989) The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol 46:1121–1123. https://doi.org/10.1001/archneur.1989.00520460115022
Lambert CP, Archer RL, Evans WJ (2001) Muscle strength and fatigue during isokinetic exercise in individuals with multiple sclerosis. Med Sci Sports Exerc 33:1613–1619. https://doi.org/10.1097/00005768-200110000-00001
Liu M, Fan S, Xu Y, Cui L (2019) Non-invasive brain stimulation for fatigue in multiple sclerosis patients: A systematic review and meta-analysis. Multiple Sclero Related Dis. https://doi.org/10.1016/j.msard.2019.08.017
Matta J, Wiernik E, Robineau O et al (2022) Association of self-reported COVID-19 infection and SARS-CoV-2 serology test results with persistent physical symptoms among french adults during the COVID-19 pandemic. JAMA Intern Med 182:19–25. https://doi.org/10.1001/jamainternmed.2021.6454
Michielsen HJ, De Vries J, Van Heck GL (2003) Psychometric qualities of a brief self-rated fatigue measure: the fatigue assessment scale. J Psychosom Res 54:345–352. https://doi.org/10.1016/s0022-3999(02)00392-6
Nalbandian A, Sehgal K, Gupta A et al (2021) Post-acute COVID-19 syndrome. Nat Med 27:601–615. https://doi.org/10.1038/s41591-021-01283-z
Nuzzo D, Cambula G, Bacile I et al (2021) Long-term brain disorders in post Covid-19 neurological syndrome (PCNS) Patient. Brain Sci. https://doi.org/10.3390/brainsci11040454
O’Connor RJ, Preston N, Parkin A et al (2022) The COVID-19 yorkshire rehabilitation scale (C19-YRS): application and psychometric analysis in a post-COVID-19 syndrome cohort. J Med Virol 94:1027–1034. https://doi.org/10.1002/jmv.27415
Pardini M, Bonzano L, Mancardi GL, Roccatagliata L (2010) Frontal networks play a role in fatigue perception in multiple sclerosis. Behav Neurosci 124:329–336. https://doi.org/10.1037/a0019585
Peterson JA, Bemben MG, Larson RD, Pereira H, Crowson HM, Black CD (2022) Symptomatic but not asymptomatic COVID-19 impairs conditioned pain modulation in young adults. J Pain 23:1923–1932. https://doi.org/10.1016/j.jpain.2022.06.010
Qin Y, Wu J, Chen T et al (2021) Long-term microstructure and cerebral blood flow changes in patients recovered from COVID-19 without neurological manifestations. J Clin Invest. https://doi.org/10.1172/JCI147329
Roelcke U, Kappos L, Lechner-Scott J et al (1997) Reduced glucose metabolism in the frontal cortex and basal ganglia of multiple sclerosis patients with fatigue: a 18F-fluorodeoxyglucose positron emission tomography study. Neurology 48:1566–1571. https://doi.org/10.1212/wnl.48.6.1566
Rogers JP, Chesney E, Oliver D et al (2020) Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 7:611–627. https://doi.org/10.1016/S2215-0366(20)30203-0
Rooney S, McFadyen DA, Wood DL, Moffat DF, Paul PL (2019) Minimally important difference of the fatigue severity scale and modified fatigue impact scale in people with multiple sclerosis. Mult Scler Relat Disord 35:158–163. https://doi.org/10.1016/j.msard.2019.07.028
Rudroff T, Fietsam AC, Deters JR, Bryant AD, Kamholz J (2020) Post-COVID-19 Fatigue: Potential Contributing Factors. Brain Sci. https://doi.org/10.3390/brainsci10121012
Rudroff T, Workman CD, Ponto LLB (2021) (18)F-FDG-PET Imaging for Post-COVID-19 Brain and Skeletal Muscle Alterations. Viruses. https://doi.org/10.3390/v13112283
Rudroff T, Workman CD, Bryant AD (2022) potential factors that contribute to post-COVID-19 fatigue in women. Brain Sci. https://doi.org/10.3390/brainsci12050556
Sandler CX, Wyller VBB, Moss-Morris R et al (2021) Long COVID and post-infective fatigue syndrome: a review. Open Forum Infect. https://doi.org/10.1093/ofid/ofab440
Schulze H, Charles James J, Trampe N et al (2022) Cross-sectional analysis of clinical aspects in patients with long-COVID and post-COVID syndrome. Front Neurol 13:979152. https://doi.org/10.3389/fneur.2022.979152
Sollini M, Morbelli S, Ciccarelli M et al (2021) Long COVID hallmarks on [18F]FDG-PET/CT: a case-control study. Eur J Nucl Med Mol Imaging 48:3187–3197. https://doi.org/10.1007/s00259-021-05294-3
Tellez N, Alonso J, Rio J, Tintore M, Nos C, Montalban X, Rovira A (2008) The basal ganglia: a substrate for fatigue in multiple sclerosis. Neuroradiology 50:17–23. https://doi.org/10.1007/s00234-007-0304-3
Tian Y, Tu X, Zhou X et al (2020) Wearing a N95 mask increases rescuer’s fatigue and decreases chest compression quality in simulated cardiopulmonary resuscitation. Am J Emerg Med. https://doi.org/10.1016/j.ajem.2020.05.065
Wang D, Hu B, Hu C et al (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323:1061–1069. https://doi.org/10.1001/jama.2020.1585
Wijeratne T, Crewther S (2021) COVID-19 and long-term neurological problems: Challenges ahead with Post-COVID-19 Neurological Syndrome. Aust J Gen Pract. https://doi.org/10.31128/AJGP-COVID-43
Workman CD, Fietsam AC, Rudroff T (2020a) Associations of lower limb joint asymmetry with fatigue and disability in people with multiple sclerosis. Clin Biomech (bristol, Avon) 75:104989. https://doi.org/10.1016/j.clinbiomech.2020.104989
Workman CD, Kamholz J, Rudroff T (2020b) Increased leg muscle fatigability during 2 mA and 4 mA transcranial direct current stimulation over the left motor cortex. Exp Brain Res 238:333–343. https://doi.org/10.1007/s00221-019-05721-w
Workman CD, Kamholz J, Rudroff T (2020c) Transcranial direct current stimulation (tDCS) for the treatment of a Multiple Sclerosis symptom cluster. Brain Stimul 13:263–264. https://doi.org/10.1016/j.brs.2019.09.012
Xu XW, Wu XX, Jiang XG et al (2020) Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ 368:m606. https://doi.org/10.1136/bmj.m606
Acknowledgements
The authors would like to thank the study participants for their time and effort.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Conceptualization, A.C.F. and T.R.; methodology, A.C.F. and T.R.; formal analysis, A.C.F.; writing—original draft preparation, A.C.F. and T.R., writing—review and editing A.C.F., A.D. B., and T.R. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Institutional review board statement
This study was performed per the Declaration of Helsinki, approved by the University of Iowa Institutional Review Board (IRB #202009381).
Additional information
Communicated by Bill J Yates.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fietsam, A.C., Bryant, A.D. & Rudroff, T. Fatigue and perceived fatigability, not objective fatigability, are prevalent in people with post-COVID-19. Exp Brain Res 241, 211–219 (2023). https://doi.org/10.1007/s00221-022-06518-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-022-06518-0