Abstract
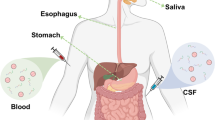
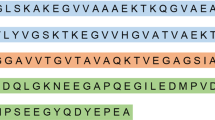
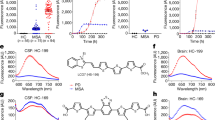
Parkinson’s disease is a health-threatening neurodegenerative disease of the elderly with clinical manifestations of motor and non-motor deficits such as tremor palsy and loss of smell. Alpha-synuclein (α-Syn) is the pathological basis of PD, it can abnormally aggregate into insoluble forms such as oligomers, fibrils, and plaques, causing degeneration of nigrostriatal dopaminergic neurons in the substantia nigra in the patient’s brain and the formation of Lewy bodies (LBs) and Lewy neuritis (LN) inclusions. As a result, achieving α-Syn aggregate detection in the early stages of PD can effectively stop or delay the progression of the disease. In this paper, we provide a brief overview and analysis of the molecular structures and α-Syn in vivo and in vitro detection methods, such as mass spectrometry, antigen–antibody recognition, electrochemical sensors, and imaging techniques, intending to provide more technological support for detecting α-Syn early in the disease and intervening in the progression of Parkinson’s disease.
Graphical abstract







Similar content being viewed by others
References
Benadiba M, Luurtsema G, Wichert-Ana L, Buchpigel CA, Busatto FG. New molecular targets for PET and SPECT imaging in neurodegenerative diseases. Braz J Psychiatry. 2012;34(2):125–48. https://doi.org/10.1016/j.rbp.2012.07.002.
O’ Hara DM, Kalia SK, Kalia LV. Methods for detecting toxic α-Synuclein species as a biomarker for Parkinson’s disease. Crit Rev Clin Lab Sci. 2020;57(5):291–307. https://doi.org/10.1080/10408363.2019.1711359.
Kundel F, Tosatto L, Whiten DR, Wirthensohn DC, Horrocks MH, Klenerman D. Shedding light on aberrant interactions-a review of modern tools for studying protein aggregates. FEBS J. 2018;285(19):3604–30. https://doi.org/10.1111/febs.14409.
Cao KJ, Yang J. Translational opportunities for amyloid-targeting fluorophores. Chem Commun (Camb). 2018;54(66):9107–18. https://doi.org/10.1039/C8CC03619E.
Han D, Zheng W, Wang X, Chen Z. Proteostasis of α-Synuclein and its role in the pathogenesis of Parkinson’s disease. Front Cell Neurosci. 2020;14(45). https://doi.org/10.3389/fncel.2020.00045.
Fricova D, Harsanyiova J, Kralova TA. Alpha-synuclein in the gastrointestinal tract as a potential biomarker for early detection of Parkinson’s disease. Int J Mol Sci. 2020;21(22):8666. https://doi.org/10.3390/ijms21228666.
Rietdijk CD, Perez-Pardo P, Garssen J, van Wezel RJ, Kraneveld AD. Exploring Braak’s hypothesis of Parkinson’s disease. Front Neurol. 2017; 8(37). https://doi.org/10.3389/fneur.2017.00037.
Sulatskaya AI, Rodina NP, Sulatsky MI, Povarova OI, Antifeeva IA, Kuznetsova IM, Turoverov KK. Investigation of α-Synuclein amyloid fibrils using the fluorescent probe thioflavin-T. Int J Mol Sci. 2018;19(9):2486. https://doi.org/10.3390/ijms19092486.
Ghosh S, Sakshi, Swain BC, Chakraborty R, Tripathy U, Chattopadhyay K. A novel tool to investigate the early and late stages of α-synuclein aggregation. ACS Chem Neurosci. 2020;11(11):1610–1619. https://doi.org/10.1021/acschemneuro.0c00068.
Granado N, Gómez-Benito M, García-Sanz P, Michel A, Dumoulin M, Moratalla R. Modeling Parkinson’s disease with the alpha-synuclein protein. Front Pharmacol. 2020;11:356. https://doi.org/10.3389/fphar.2020.00356.
Sidhu A, Vaneyck J, Blum C, Segers-Nolten I, Subramaniam V. Polymorph-specific distribution of binding sites determines thioflavin-T fluorescence intensity in α-synuclein fibrils. Amyloid. 2018;25(3):189–96. https://doi.org/10.1080/13506129.2018.1517736.
Uzuegbunam BC, Librizzi D, Hooshyar YB. PET radiopharmaceuticals for Alzheimer’s disease and Parkinson’s disease diagnosis, the current and future landscape. Molecules. 2020;25(4):977. https://doi.org/10.3390/molecules25040977.
Avidan-Shpalter C, Gazit E. The early stages of amyloid formation: biophysical and structural characterization of human calcitonin pre-fibrillar assemblies. Amyloid. 2006;13(4):216–25. https://doi.org/10.1080/13506120600960643.
Tavassoly O, Nokhrin S, Dmitriev OY, Lee JS. Cu (II) and dopamine bind to α-synuclein and cause large conformational changes. FEBS J. 2014;281(12):2738–53. https://doi.org/10.1111/febs.12817.
Rekas A, Lo V, Gadd GE, Cappai R, Yun SI. PAMAM dendrimers as potential agents against fibrillation of alpha-synuclein, a Parkinson’s disease-related protein. Macromol Biosci. 2009;9(3):230–8. https://doi.org/10.1002/mabi.200800242.
Li X, Dong C, Hoffmann M, Garen CR, Cortez LM, Petersen NO. Woodside MT. Early stages of aggregation of engineered α-synuclein monomers and oligomers in solution. Sci Rep. 2019;11;9(1):1734. https://doi.org/10.1038/s41598-018-37584-6.
Flynn JD, Jiang Z, Lee JC. Segmental 13C-labeling and raman microspectroscopy of α-synuclein amyloid formation. Angew Chem Int Ed Engl. 2018;57(52):17069–72. https://doi.org/10.1002/anie.201809865.
Canale C, Torre B, Ricci D, Braga PC. Recognizing and avoiding artifacts in atomic force microscopy imaging. Methods Mol Biol. 2011;736:31–43. https://doi.org/10.1007/978-1-61779-105-5_3.
McAllister C, Karymov MA, Kawano Y, Lushnikov AY, Mikheikin A, Uversky VN, Lyubchenko YL. Protein interactions and misfolding analyzed by AFM force spectroscopy. J Mol Biol. 2005;354(5):1028–42. https://doi.org/10.1016/j.jmb.2005.10.012.
Campioni S, Carret G, Jordens S, Nicoud L, Mezzenga R, Riek R. The presence of an air-water interface affects formation and elongation of α-Synuclein fibrils. J Am Chem Soc. 2014;136(7):2866–75. https://doi.org/10.1021/ja412105t.
Taylor CG, Meisl G, Horrocks MH, Zetterberg H, Knowles TPJ, Klenerman D. Extrinsic amyloid-binding dyes for detection of individual protein aggregates in solution. Anal Chem. 2018;90(17):10385–93. https://doi.org/10.1021/acs.analchem.8b02226.
Beveridge R, Phillips AS, Denbigh L, Saleem HM, MacPhee CE, Barran PE. Relating gas phase to solution conformations: lessons from disordered proteins. Proteomics. 2015;15(16):2872–83. https://doi.org/10.1002/pmic.201400605.
Bhattacharjee P, Öhrfelt A, Lashley T, Blennow K, Brinkmalm A, Zetterberg H. Mass spectrometric analysis of Lewy body-enriched α-Synuclein in Parkinson’s disease. J Proteome Res. 2019;18(5):2109–20. https://doi.org/10.1021/acs.jproteome.8b00982.
Prakash A, Rezai T, Krastins B, Sarracino D, Athanas M, Russo P, Zhang H, Tian Y, Li Y, Kulasingam V, Drabovich A, Smith CR, Batruch I, Oran PE, Fredolini C, Luchini A, Liotta L, Petricoin E, Diamandis EP, Chan DW, Nelson R, Lopez MF. Interlaboratory reproducibility of selective reaction monitoring assays using multiple upfront analyte enrichment strategies. J Proteome Res. 2012;11(8):3986–95. https://doi.org/10.1021/pr300014s.
Pryor NE, Moss MA, Hestekin CN. Unraveling the early events of amyloid-β protein (Aβ) aggregation: techniques for the determination of Aβ aggregate size. Int J Mol Sci. 2012;13(3):3038–72. https://doi.org/10.3390/ijms13033038.
Zhang C, Woolfork AG, Suh K, Ovbude S, Bi C, Elzoeiry M, Hage DS. Clinical and pharmaceutical applications of affinity ligands in capillary electrophoresis: a review. J Pharm Biomed Anal. 2020;177:112882. https://doi.org/10.1016/j.jpba.2019.112882.
Pero-Gascon R, Benavente F, Minic Z, Berezovski MV, Sanz-Nebot V. On-line aptamer affinity solid-phase extraction capillary electrophoresis-mass spectrometry for the analysis of blood α-Synuclein. Anal Chem. 2020;92(1):1525–33. https://doi.org/10.1021/acs.analchem.9b04802.
Tiwari S, Atluri V, Kaushik A, Yndart A, Nair M. Alzheimer’s disease: pathogenesis, diagnostics, and therapeutics. Int J Nanomedicine. 2019;14:5541–54. https://doi.org/10.2147/IJN.S200490.
Karanth S, Nelson PT, Katsumata Y, Kryscio RJ, Schmitt FA, Fardo DW, Cykowski MD, Jicha GA, Van Eldik LJ, Abner EL. Prevalence and clinical phenotype of quadruple misfolded proteins in older adults. JAMA Neurol. 2020;77(10):1299–307. https://doi.org/10.1001/jamaneurol.2020.1741.
PP Liu, Xie Y, Meng XY, Kang JS. History and progress of hypotheses and clinical trials for Alzheimer’s disease. Signal Transduct Target Ther. 2019;4:29. https://doi.org/10.1038/s41392-019-0063-8.
Ruffmann C, Parkkinen L. Gut feelings about α-synuclein in gastrointestinal biopsies: biomarker in the making? Mov Disord. 2016;31(2):193–202. https://doi.org/10.1002/mds.26480.
Ruffmann C, Bengoa-Vergniory N, Poggiolini I, Ritchie D, Hu MT. Alegre-Abarrategui J, Parkkinen L. Detection of alpha-synuclein conformational variants from gastro-intestinal biopsy tissue as a potential biomarker for Parkinson’s disease. Neuropathol Appl Neurobiol. 2018;44(7):722-736. https://doi.org/10.1111/nan.12486.
Hawkes CH, Del Tredici K, Braak H. Parkinson’s disease: the dual hit theory revisited. Ann N Y Acad Sci. 2009;1170:615–22. https://doi.org/10.1111/j.1749-6632.2009.04365.x.
Beach TG, Adler CH, Sue LI, Vedders L, Lue L, White Iii CL, Akiyama H, Caviness JN, Shill HA, Sabbagh MN, Walker DG. Arizona Parkinson’s Disease Consortium. Multi-organ distribution of phosphorylated alpha-synuclein histopathology in subjects with Lewy body disorders. Acta Neuropathol. 2010;119(6):689–702. https://doi.org/10.1007/s00401-010-0664-3.
Melli G, Vacchi E, Biemmi V, Galati S, Staedler C, Ambrosini R, Kaelin-Lang A. Cervical skin denervation associates with alpha-synuclein aggregates in Parkinson disease. Ann Clin Transl Neurol. 2018;5(11):1394–407. https://doi.org/10.1002/acn3.669.
Zange L, Noack C, Hahn K, Stenzel W, Lipp A. Phosphorylated α-synuclein in skin nerve fibres differentiates Parkinson’s disease from multiple system atrophy. Brain. 2015;138(8):2310–21. https://doi.org/10.1093/brain/awv138.
Kuzkina A, Schulmeyer L, Monoranu CM, Volkmann J, Sommer C, Doppler K. The aggregation state of α-synuclein deposits in dermal nerve fibers of patients with Parkinson’s disease resembles that in the brain. Parkinsonism Relat Disord. 2019;64:66–72. https://doi.org/10.1016/j.parkreldis.2019.03.003.
Spinelli KJ, Taylor JK, Osterberg VR, Churchill MJ, Pollock E, Moore C, Meshul CK, Unni VK. Presynaptic alpha-synuclein aggregation in a mouse model of Parkinson’s disease. J Neurosci. 2014;34(6):2037–50. https://doi.org/10.1523/JNEUROSCI.2581-13.2014.
Doppler Doppler K, Ebert S, Uçeyler N, Trenkwalder C, Ebentheuer J, Volkmann J, Sommer C. Cutaneous neuropathy in Parkinson’s disease: a window into brain pathology. Acta Neuropathol. 2014;128(1):99–109. https://doi.org/10.1007/s00401-014-1284-0.
Liu X, Yang J, Yuan Y, He Q, Gao Y, Jiang C, Li L, Xu Y. Optimization of the detection method for phosphorylated α-synuclein in Parkinson disease by skin biopsy. Front Neurol. 2020; 11: 569446. https://doi.org/10.3389/fneur.2020.569446.
Antunes L, Frasquilho S, Ostaszewski M, Weber J, Longhino L, Antony P, Baumuratov A, Buttini M, et al. Similar α-synuclein staining in the colon mucosa in patients with Parkinson’s disease and controls. Movement Disord. 2016;31(10):1567–70. https://doi.org/10.1002/mds.26702.
Gold A, Turkalp ZT, Munoz DG. Enteric alpha-synuclein expression is increased in Parkinson’s disease but not Alzheimer’s disease. Movement Disord. 2013;28(2):237–41. https://doi.org/10.1002/mds.25298.
Veys L, Vandenabeele M, Ortuno-Lizaran I, Baekelandt V, Cuenca N, Moons L, De Groef L. Retinal alpha-synuclein deposits in Parkinson’s disease patients and animal models. Acta Neuropathol. 2019;137(3):379–95. https://doi.org/10.1007/s00401-018-01956-z.
Leger F, Fernagut PO, Canron MH, Leoni S, Vital C, Tison F, Bezard E, Vital A. Protein aggregation in the aging retina. J Neuropathol Exp Neurol. 2011;70(1):63–8. https://doi.org/10.1097/NEN.0b013e31820376cc.
Nakai M, Fujita M, Waragai M, Sugama S, Wei J, Akatsu H, Ohtaka-Maruyama C, Okado H, et al. Expression of α-synuclein, a presynaptic protein implicated in Parkinson’s disease, in erythropoietic lineage. Biochem Bioph Res Co. 2007;358(1):104–10. https://doi.org/10.1016/j.bbrc.2007.04.108.
Abd ES, Grigoletto J, Poli M, Arosio P, Arkadir D, Sharon R. alpha-Synuclein in blood cells differentiates Parkinson’s disease from healthy controls. Ann Clin Transl Neurol. 2019;6(12):2426–36. https://doi.org/10.1002/acn3.50944.
Katayama T, Sawada J, Takahashi K, Yahara O. Cerebrospinal fluid biomarkers in Parkinson’s disease: a critical overview of the literature and meta-analyses. Brain Sci. 2020;10(7):466. https://doi.org/10.3390/brainsci10070466.
Ning H, Wu Q, Han D, Yao T, Wang J, Lu W, Lv S, Jia Q, et al. Baseline concentration of misfolded α-synuclein aggregates in cerebrospinal fluid predicts risk of cognitive decline in Parkinson’s disease. Neuropath Appl Neuro. 2018;45(4):398–409. https://doi.org/10.1111/nan.12524.
Camporesi E, Nilsson J, Brinkmalm A, Becker B, Ashton NJ, Blennow K, Zetterberg H. Fluid biomarkers for synaptic dysfunction and loss. Biomarker Insights. 2020;15:2138511671. https://doi.org/10.1177/1177271920950319.
Cao Z, Wu Y, Liu G, Jiang Y, Wang X, Wang Z, Feng T. α-Synuclein in salivary extracellular vesicles as a potential biomarker of Parkinson’s disease. Neurosci Lett. 2018;696:114–20. https://doi.org/10.1016/j.neulet.2018.12.030.
Vivacqua G, Suppa A, Mancinelli R, Belvisi D, Fabbrini A, Costanzo M, Formica A, Onori P, et al. Salivary alpha-synuclein in the diagnosis of Parkinson’s disease and progressive supranuclear palsy. Parkinsonism Relat D. 2019;63:143–8. https://doi.org/10.1016/j.parkreldis.2019.02.014.
Ashton NJ, Ide M, Zetterberg H, Blennow K. Salivary biomarkers for Alzheimer’s disease and related disorders. Neurol Ther. 2019;8(Suppl 2):83–94. https://doi.org/10.1007/s40120-019-00168-1.
Nam D, Lee J, Lee M, Kim J, Seol W, Son I, Ho DH. Detection and assessment of α-synuclein oligomers in the urine of Parkinson’s disease patients. J Parkinsons Dis. 2020;10(3):981–91. https://doi.org/10.3233/JPD-201983.
Abd-Elhadi S, Basora M, Vilas D, Tolosa E, Sharon R. Total α-synuclein levels in human blood cells, CSF, and saliva determined by a lipid-ELISA. Anal Bioanal Chem. 2016;408(27):7669–77. https://doi.org/10.1007/s00216-016-9863-7.
Bryan T, Luo X, Forsgren L, Morozova-Roche LA, Davis JJ. The robust electrochemical detection of a Parkinson’s disease marker in whole blood sera. Chem Sci (Cambridge). 2012;3(12):3468–73. https://doi.org/10.1039/c2sc21221h.
Xu Q, Cheng H, Lehr J, Patil AV, Davis JJ. Graphene oxide interfaces in serum based autoantibody quantification. Anal Chem. 2014;87(1):346–50. https://doi.org/10.1021/ac503890e.
Taghdisi SM, Danesh NM, Nameghi MA, Ramezani M, Alibolandi M, Hassanzadeh-Khayat M, Emrani AS, Abnous K. A novel electrochemical aptasensor based on nontarget-induced high accumulation of methylene blue on the surface of electrode for sensing of α-synuclein oligomer. Biosens Bioelectron. 2018;123:14–8. https://doi.org/10.1016/j.bios.2018.09.081.
Wu Q, Tan R, Mi X, Tu Y. Electrochemiluminescent aptamer-sensor for alpha synuclein oligomer based on a metal-organic framework. Analyst. 2020;145(6):2159–67. https://doi.org/10.1039/D0AN00169D.
Ge CY, Rahman MM, Zhang W, Lopa NS, Jin L, Yoon S, Jang H, Xu GR et al. An electrochemical immunosensor based on a self-assembled monolayer modified electrode for label-free detection of alpha-synuclein. Sensors (Basel). 2020;20(3). https://doi.org/10.3390/s20030617.
Hassan Q, Li S, Ferrag C, Kerman K. Electrochemical biosensors for the detection and study of α-synuclein related to Parkinson’s disease – a review. Anal Chim Acta. 2019;1089:32–9. https://doi.org/10.1016/j.aca.2019.09.013.
Chan T, Chow AM, Tang DWF, Li Q, Wang X, Brown IR, Kerman K. Interaction of baicalein and copper with α-synuclein: electrochemical approach to Parkinson’s disease. J Electroanal Chem. 2010;648(2):151–5. https://doi.org/10.1016/j.jelechem.2010.07.015.
Sonuc KM, Sezginturk MK. Cerebrospinal fluid levels of alpha-synuclein measured using a poly-glutamic acid-modified gold nanoparticle-doped disposable neuro-biosensor system. Analyst. 2019;144(2):611–21. https://doi.org/10.1039/c8an01279b.
Eberling JL, Dave KD, Frasier MA. α-Synuclein imaging: a critical need for Parkinson’s disease research. J Parkinsons Dis. 2013;3(4):565–7. https://doi.org/10.3233/JPD-130247.
Xu MM, Ren WM, Tang XC, Hu YH, Zhang HY. Advances in development of fluorescent probes for detecting amyloid-beta aggregates. Acta Pharmacol Sin. 2016;37(6):719–30. https://doi.org/10.1038/aps.2015.155.
Goldberg JM, Batjargal S, Chen BS, Petersson EJ. Thioamide quenching of fluorescent probes through photoinduced electron transfer: mechanistic studies and applications. J Am Chem Soc. 2013;135(49):18651–8. https://doi.org/10.1021/ja409709x.
Naiki H, Higuchi K, Hosokawa M, Takeda T. Fluorometric determination of amyloid fibrils in vitro using the fluorescent dye, thioflavin-T1. Anal Biochem. 1989;177(2):244–9. https://doi.org/10.1016/0003-2697(89)90046-8.
Biancalana M, Koide S. Molecular mechanism of thioflavin-T binding to amyloid fibrils. Bba-Bioenergetics. 2010;1804(7):1405–12. https://doi.org/10.1016/j.bbapap.2010.04.001.
Celej MS, Jares-Erijman EA, Jovin TM. Fluorescent N-arylaminonaphthalene sulfonate probes for amyloid aggregation of α-synuclein. Biophys J. 208;94(12):4867–4879. https://doi.org/10.1529/biophysj.107.125211.
Pravin N, Kumar R, Tripathi S, Kumar P, Mohite GM, Navalkar A, Panigrahi R, Singh N, et al. Benzimidazole-based fluorophores for the detection of amyloid fibrils with higher sensitivity than thioflavin-T. J Neurochem. 2021;156(6):1003–19. https://doi.org/10.1111/jnc.15138.
Gaur P, Galkin M, Kurochka A, Ghosh S, Yushchenko DA, Shvadchak VV. Fluorescent probe for selective imaging of α-synuclein fibrils in living cells. Acs Chem Neurosci. 2021;12(8):1293–8. https://doi.org/10.1021/acschemneuro.1c00090.
Needham LM, Weber J, Varela JA, Fyfe JWB, Do DT, Xu CK, Tutton L, Cliffe R, et al. ThX-a next-generation probe for the early detection of amyloid aggregates. Chem Sci. 2020;11(18):4578–83. https://doi.org/10.1039/C9SC04730A.
Gorka F, Daly S, Pearson CM, Bulovaite E, Zhang YP, Handa A, Grant SGN, Snaddon TN, et al. A comparative study of high-contrast fluorescence lifetime probes for imaging amyloid in tissue. J Phys Chem B. 2021;125(50):13710–7. https://doi.org/10.1021/acs.jpcb.1c07762.
Needham LM, Weber J, Pearson CM, Do DT, Gorka F, Lyu G, Bohndiek SE, Snaddon TN, Lee SF. A comparative photophysical study of structural modifications of thioflavin T-inspired fluorophores. J Phys Chem Lett. 2020;11(19):8406–16. https://doi.org/10.1021/acs.jpclett.0c01549.
Shi S, Mitteregger-Kretzschmar G, Giese A, Kretzschmar HA. Establishing quantitative real-time quaking-induced conversion (qRT-QuIC) for highly sensitive detection and quantification of PrPSc in prion-infected tissues. Acta Neuropathol Commun. 2013;1:44. https://doi.org/10.1186/2051-5960-1-44.
Bongianni M, Catalan M, Perra D, Fontana E, Janes F, Bertolotti C, et al. Olfactory swab sampling optimization for α-synuclein aggregate detection in patients with Parkinson’s disease. Transl Neurodegener. 2022;11(1):37. https://doi.org/10.1186/s40035-022-00311-3.
Bhumkar A, Magnan C, Lau D, Jun ESW, Dzamko N, Gambin Y, Sierecki E. Single-molecule counting coupled to rapid amplification enables detection of α-synuclein aggregates in cerebrospinal fluid of Parkinson’s disease patients. Angew Chem Int Ed Engl. 2021;60(21):11874–83. https://doi.org/10.1002/anie.202014898.
Singh PK, Kotia V, Ghosh D, Mohite GM, Kumar A, Maji SK. Curcumin modulates α-synuclein aggregation and toxicity. Acs Chem Neurosci. 2013;4(3):393–407. https://doi.org/10.1021/cn3001203.
Bieschke J, Russ J, Friedrich RP, Ehrnhoefer DE, Wobst H, Neugebauer K, Wanker EE. EGCG remodels mature α-synuclein and amyloid-β fibrils and reduces cellular toxicity. Proc Natl Acad Sci. 2010;107(17):7710–5. https://doi.org/10.1073/pnas.0910723107.
Wagner J, Ryazanov S, Leonov A, Levin J, Shi S, Schmidt F, Prix C, Pan-Montojo F, et al. Anle138b: a novel oligomer modulator for disease-modifying therapy of neurodegenerative diseases such as prion and Parkinson’s disease. Acta Neuropathol. 2013;125(6):795–813. https://doi.org/10.1007/s00401-013-1114-9.
Needham LM, Weber J, Fyfe JWB, Kabia OM, Do DT, Klimont E, Zhang Y, Rodrigues M, Dobson CM, Ghandi S, Bohndiek SE, Snaddon TN, Lee SF. Correction to bifunctional fluorescent probes for detection of amyloid aggregates and reactive oxygen species. R Soc Open Sci. 2018;5(2):171399. https://doi.org/10.1098/rsos.180308.
Yu L, Cui J, Padakanti PK, Engel L, Bagchi DP, Kotzbauer PT, Tu Z. Synthesis and in vitro evaluation of α-synuclein ligands. Bioorgan Med Chem. 2012;20(15):4625–34. https://doi.org/10.1016/j.bmc.2012.06.023.
Kovalska VB, Losytskyy MY, Tolmachev OI, Slominskii YL, Segers-Nolten GMJ, Subramaniam V, Yarmoluk SM. Tri- and pentamethine cyanine dyes for fluorescent detection of α-synuclein oligomeric aggregates. J Fluoresc. 2012;22(6):1441–8. https://doi.org/10.1007/s10895-012-1081-x.
Paslawski W, Andreasen M, Nielsen SB, Lorenzen N, Thomsen K, Kaspersen JD, Pedersen JS, Otzen DE. High stability and cooperative unfolding of α-synuclein oligomers. Biochemistry-US. 2014;53(39):6252–63. https://doi.org/10.1021/bi5007833.
Lee J, Lee I, Choe Y, Kang S, Kim HY, Gai W, Hahn J, Paik SR. Real-time analysis of amyloid fibril formation of α-synuclein using a fibrillation-state-specific fluorescent probe of JC-1. Biochem J. 2009;418(2):311–23. https://doi.org/10.1042/BJ20081572.
Wang Y, Qiu Y, Sun A, Xiong Y, Tan H, Shi Y, Yu P, Roy G, et al. Dual-functional AIE fluorescent probes for imaging β-amyloid plaques and lipid droplets. Anal Chim Acta. 2020;1133:109–18. https://doi.org/10.1016/j.aca.2020.07.073.
Mei J, Leung NLC, Kwok RTK, Lam JWY, Tang BZ. Aggregation-induced emission: together we shine, united we soar. Chem Rev. 2015;115(21):11718–940. https://doi.org/10.1021/acs.chemrev.5b00263.
Marzano NR, Wray KM, Johnston CL, Paudel BP, Hong Y, van Oijen A, Ecroyd H. An α-cyanostilbene derivative for the enhanced detection and imaging of amyloid fibril aggregates. Acs Chem Neurosci. 2020;11(24):4191–202. https://doi.org/10.1021/acschemneuro.0c00478.
Leung CW, Guo F, Hong Y, Zhao E, Kwok RT, Leung NL, Chen S, Vaikath NN, El-Agnaf OM, Tang Y, Gai WP, Tang BZ. Detection of oligomers and fibrils of α-synuclein by AIE-gen with strong fluorescence. ChemComm (Camb). 2015;51(10):1866–9. https://doi.org/10.1039/C4CC07911F.
Benadiba M, Luurtsema G, Wichert-Ana L, Buchpigel CA, Busatto FG. New molecular targets for PET and SPECT imaging in neurodegenerative diseases. Rev Bras Psiquiatr. 2012;34(S2):S125–36. https://doi.org/10.1016/j.rbp.2012.07.002.
Brooks DJ. Imaging familial and sporadic neurodegenerative disorders associated with Parkinsonism. Neurotherapeutics. 2021;18(2):753–71. https://doi.org/10.1007/s13311-020-00994-4.
Cortes-Blanco A, Prieto-Yerro C, Martinez-Lazaro R, Zamora J, Jiménez-Huete A, Haberkamp M, Pohly J, Enzmann H, Zinserling J, Strassmann V, Broich K. Florbetapir (18F) for brain amyloid positron emission tomography: highlights on the European marketing approval. Alzheimers Dement. 2014;10(5 Suppl):S395–9. https://doi.org/10.1016/j.jalz.2013.09.007.
Rominger A, Brendel M, Burgold S, Keppler K, Baumann K, Xiong G, et al. Longitudinal assessment of cerebral β-amyloid deposition in mice overexpressing Swedish mutant β-amyloid precursor protein using 18F florbetaben PET. J Nucl Med. 2013;54:1127–34. https://doi.org/10.2967/jnumed.112.114660.
Barthel H, Sabri O. Florbetaben to trace amyloid-β in the Alzheimer brain by means of PET. J Alzheimers Dis. 2011;26(Suppl 3):117–21. https://doi.org/10.3233/JAD-2011-0068.
Martínez G, Vernooij RW, Fuentes Padilla P, Zamora J, Flicker L, Bonfill Cosp X. 18F PET with flutemetamol for the early diagnosis of Alzheimer’s disease dementia and other dementias in people with mild cognitive impairment (MCI). Cochrane Database Syst Rev. 2017; 11(11):CD012884. https://doi.org/10.1002/14651858.CD012884.
Skovronsky D, Dyrks T, Holl G, Krause S, Friebe M, Lehman L, Lindemann S, Dinkelborg LM, Masters CL, Villemagne VL. Imaging of amyloid beta in Alzheimer’s disease with 18F-BAY94-9172, a novel PET tracer: proof of mechanism. Lancet Neurol. 2008;7(2):129–35. https://doi.org/10.1016/S1474-4422(08)70001-2.
Shah M, Seibyl J, Cartier A, Bhatt R, Catafau AM. Molecular imaging insights into neurodegeneration: focus on alpha-synuclein radiotracers. J Nucl Med. 2014;55(9):1397–400. https://doi.org/10.2967/jnumed.113.136515.
Klunk WE, Engler H, Nordberg A, Wang Y, Blomqvist G, Holt DP, et al. Imaging brain amyloid in Alzheimer’s disease with pittsburgh compound-B. Ann Neurol. 2004;55(3):306–19. https://doi.org/10.1002/ana.20009.
Fodero-Tavoletti MT, Mulligan RS, Okamura N, Furumoto S, Rowe CC, Kudo Y, Masters CL, Cappai R, et al. In vitro characterisation of BF227 binding to α-synuclein/Lewy bodies. Eur J Pharmacol. 2009;617(1–3):54–8. https://doi.org/10.1016/j.ejphar.2009.06.042.
Josephson L, Stratman N, Liu Y, Qian F, Liang SH, Vasdev N, Patel S. The binding of BF-227-like benzoxazoles to human α-synuclein and amyloid β peptide fibrils. Mol Imaging. 2018;17:296472781. https://doi.org/10.1177/1536012118796297.
Koga S, Ono M, Sahara N, Higuchi M, Dickson DW. Fluorescence and autoradiographic evaluation of tau PET ligand PBB3 to α-synuclein pathology. Mov Disord. 2017;32(6):884–92. https://doi.org/10.1002/mds.27013.
Fujishiro H, Imamura AY, Lin WL, Uchikado H, Mark MH, Golbe LI, Markopoulou K, Wszolek ZK, et al. Diversity of pathological features other than Lewy bodies in familial Parkinson’s disease due to SNCA mutations. Am J Neurodegener Dis. 2013;2(4):266-275.
Bagchi DP, Yu L, Perlmutter JS, Xu J, Mach RH, Tu Z, Kotzbauer PT. Binding of the radioligand SIL23 to α-synuclein fibrils in Parkinson disease brain tissue establishes feasibility and screening approaches for developing a Parkinson disease imaging agent. PLoS ONE. 2013;8(2): e55031. https://doi.org/10.1371/journal.pone.0055031.
Zhang X, Jin H, Padakanti P, Li J, Yang H, Fan J, Mach R, Kotzbauer P, et al. Radiosynthesis and in vivo evaluation of two PET radioligands for imaging α-synuclein. Appl Sci. 2014;4(1):66–78. https://doi.org/10.3390/app4010066.
Chu W, Zhou D, Gaba V, Liu J, Li S, Peng X, et al. Design, synthesis, and characterization of 3-(Benzylidene) indolin-2-one derivatives as ligands for α-synuclein fibrils. J Med Chem. 2015;58:6002–17. https://doi.org/10.1021/acs.jmedchem.5b00571.
Yue X, Dhavale DD, Li J, Luo Z, Liu J, Yang H, Mach RH, Kotzbauer PT, Tu Z. Design, synthesis, and in vitro evaluation of quinolinyl analogues for α-synuclein aggregation. Bioorg Med Chem Lett. 2018;28(6):1011–9. https://doi.org/10.1016/j.bmcl.2018.02.031.
Maurer A, Leonov A, Ryazanov S, Herfert K, Kuebler L, Buss S, Schmidt F, Weckbecker D, et al. 11C Radiolabeling of anle253b: a putative PET tracer for Parkinson’s disease that binds to α-synuclein fibrils in vitro and crosses the blood-brain barrier. ChemMedChem. 2020;15(5):411–5. https://doi.org/10.1002/cmdc.201900689.
Hooshyar Yousefi B, Shi K, Reder S, Reder S, Herz M, Braeuer M, et al. First in vivo imaging and in vitro studies of 18F-DABTA in rat model with E46K alpha synuclein mutation. Eur J Nucl Med Mol Imaging. USA: SPRINGER. 2017;44(Suppl 2):161.
Fanti S, Bonfiglioli R, Decristoforo C. Highlights of the 30th annual congress of the EANM, Vienna 2017: “Yes we can–make nuclear medicine great again.” Eur J Nucl Med Mol I. 2018;45(10):1781–94. https://doi.org/10.1007/s00259-018-4029-9.
Clark CM, Schneider JA, Bedell BJ, Beach TG, Bilker WB, Mintun MA, et al. Use of florbetapir-PET for imaging beta-amyloid pathology. JAMA. 2011;305:275–83. https://doi.org/10.1001/jama.2010.2008.
Sabri O, Seibyl J, Rowe C, Barthel H. Beta-amyloid imaging with florbetaben. Clin Transl Imaging. 2015;3(1):13–26. https://doi.org/10.1007/s40336-015-0102-6.
Snellman A, Rokka J, Lopez-Picon FR, Eskola O, Wilson I, Farrar G, et al. Pharmacokinetics of [18F] flutemetamol in wild-type rodents and its binding to beta amyloid deposits in a mouse model of Alzheimer’s disease. Eur J Nucl Med Mol Imaging. 2012;39:1784–95. https://doi.org/10.1007/s00259-012-2178-9.
Klunk WE, Lopresti BJ, Ikonomovic MD, Lefterov IM, Koldamova RP, Abrahamson EE, et al. Binding of the positron emission tomography tracer Pittsburgh compound-B reflects the amount of amyloid-beta in Alzheimer’s disease brain but not in transgenic mouse brain. J Neurosci. 2005;25:10598–606. https://doi.org/10.1523/JNEUROSCI.2990-05.2005.
Levigoureux E, Lancelot S, Bouillot C, Chauveau F, Verdurand M, Verchere J, et al. Binding of the PET radiotracer [18F]BF227 does not reflect the presence of alpha-synuclein aggregates in transgenic mice. Curr Alzheimer Res. 2014;11:955–60.
Perez-Soriano A, Arena JE, Dinelle K, Miao Q, McKenzie J, Neilson N, Puschmann A, Schaffer P, Shinotoh H, Smith-Forrester J, Shahinfard E, Vafai N, Wile D, Wszolek Z, Higuchi M, Sossi V, Stoessl AJ. PBB3 imaging in Parkinsonian disorders: evidence for binding to tau and other proteins. Mov Disord. 2017;32(7):1016–24. https://doi.org/10.1002/mds.27029.
Aboagye E, Kraeber-Bodéré F. Highlights lecture EANM 2016: “Embracing molecular imaging and multi-modal imaging: a smart move for nuclear medicine towards personalized medicine.” Eur J Nucl Med Mol Imaging. 2017;44:1559–74. https://doi.org/10.1007/s00259-017-3704-6.
Yousaf T, Dervenoulas G, Politis M. Advances in MRI methodology. Int Rev Neurobiol. 2018;141:31–76. https://doi.org/10.1016/bs.irn.2018.08.008.
Cousins O, Yousaf T, Wilson H, Pagano G, Politis M. Molecular imaging of dementia with Lewy bodies. Int Rev Neurobiol. 2019;144:59–93. https://doi.org/10.1016/bs.irn.2018.10.007.
Politis M. Neuroimaging in Parkinson disease: from research setting to clinical practice. Nat Rev Neurol. 2014;10(12):708–22. https://doi.org/10.1038/nrneurol.2014.205.
Khairnar A, Ruda-Kucerova J, Szabó N, Drazanova E, Arab A, Hutter-Paier B, Neddens J, Latta P, Starcuk ZJ, Rektorova I. Early and progressive microstructural brain changes in mice overexpressing human α-synuclein detected by diffusion kurtosis imaging. Brain Behav Immun. 2017;61:197–208. https://doi.org/10.1016/j.bbi.2016.11.027.
Ding XB, Wang XB, Xia DH, Liu H, Tian HY, Fu Y, Chen YK, Qin C, Wang JQ, Xiang Z, Zhang ZX, Cao QC, Wang W, Li JY, Wu E, Tang BS, Ma MM, Teng JF, Wang XJ. Impaired meningeal lymphatic drainage in patients with idiopathic Parkinson’s disease. Nat Med. 2021;27(3):411–8. https://doi.org/10.1038/s41591-020-01198-1.
Acknowledgements
We thank Prof. Yanjun Zhang, Prof. Pengwei Zhuang, and Associate Prof. Hong Guo for their valuable comments and suggestions on this manuscript.
Funding
This study has been partially funded by the Tianjin Science and Technology Planning Project (21JCQNJC01350) and co-funded by the Tianjin University of Traditional Chinese Medicine Scientific Research Support Project and Tianjin University of Traditional Chinese Medicine twelfth College Students Science and Technology Innovation Fund (ZR19). The funders had no role in the study design or decision to publish this article.
Author information
Authors and Affiliations
Contributions
Dr. Mei-ling Chen and Dr. Yu-bo Li conceived the idea. Rui Wang, Jing-ya Li, Chan-lian Li, and Jun-miao Liu completed the work of literature retrieval. Dr. Shun-chao Pang and Rui Wang provided written input on the scientific content of drafts. Dr. Mei-ling Chen, Rui Wang, and Yu-ming Wang revised the manuscript and approved the final draft for submission. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
The authors mentioned have participated in this article.
Consent for publication
The authors approved the publication of this article.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, R., Pang, Sc., Li, Jy. et al. A review of the current research on in vivo and in vitro detection for alpha-synuclein: a biomarker of Parkinson’s disease. Anal Bioanal Chem 415, 1589–1605 (2023). https://doi.org/10.1007/s00216-023-04520-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-023-04520-1