Abstract
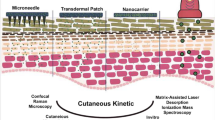
Study of skin penetration and distribution of the drug compounds in the skin is a major challenge in the development of topical drug products for treatment of skin diseases. It is crucial to have fast and efficacious screening methods which can provide information concerning the skin penetration and the distribution of the drug molecules in the region of the target. Mass spectrometry imaging (MSI) such as matrix-assisted laser desorption/ionization (MALDI)-MSI offers the opportunity to analyze the drug distribution at micrometer scale, but is a low throughput technique. Cassette dosing of drug molecules has been widely used for two decades as a high throughput screening tool for plasma pharmacokinetic analysis. The purpose of this study is to evaluate the utility of combining MALDI-MSI with cassette dosing to obtain a medium throughput screening technique for drug distribution in the skin directly from thin tissue sections. Excised fresh human skin was treated with two different formulation types containing both single drugs and a cassette with four drugs. Biopsies were taken and analyzed with traditional UHPLC-MS/MS and MALDI-MSI. The results reveal that skin penetration data of the four drugs administered together were in agreement with skin penetration data obtained when the molecules were administered individually. Furthermore, the MALDI-MSI data reveal different distribution profiles of the four drugs which were not possible to deduce from the UHPLC-MS/MS bioanalysis. These findings suggest that combination of MALDI-MSI and cassette dosing can be used as a medium throughput screening tool at an early stage in the drug discovery/development process.

Investigation of drug distribution in human skin explant by MALDI-MSI after cassette dosing








Similar content being viewed by others
References
Wilsmann-Theis D, Hagemann T, Jordan J, Bieber T, Novak N. Facing psoriasis and atopic dermatitis: are there more similarities or more differences? Eur J Dermatol. 2008;18:172–80.
Leite-Silva VR, de Almeida MM, Fradin A, Grice JE, Roberts MS. Delivery of drugs applied topically to the skin. Expert Rev Dermatol. 2012;7:383–97.
Schaefer H, Redelmeier TE. Skin barrier: principles of percutaneous absorption. New York: Karger; 1996.
Hadgraft J, Lane ME. Skin permeation: the years of enlightenment. Int J Pharm. 2005;305:2–12.
Marks R. The stratum corneum barrier: the final frontier. J Nutr. 2004;134:2017S–21S.
Choy YB, Prausnitz MR. The rule of five for non-oral routes of drug delivery: ophthalmic, inhalation and transdermal Pharm Res 2011;28:943–948.
Magnusson BM, Cross SE, Winckle G, Roberts MS. Percutaneous absorption of steroids: determination of in vitro permeability and tissue reservoir characteristics in human skin layers. Skin Pharmacol Physiol. 2006;19:336–42.
Zhang Q, Li P, Roberts MS. Maximum transepidermal flux for similar size phenolic compounds is enhanced by solvent uptake into the skin. J Control Release. 2011;154:50–7.
Zhang Q, Li P, Liu D, Roberts MS. Effect of vehicles on the maximum transepidermal flux of similar size phenolic compounds. Pharm Res. 2013;30:32–40.
Magnusson BM, Anissimov YG, Cross SE, Roberts MS. Molecular size as the main determinant of solute maximum flux across the skin. J Invest Dermatol. 2004;122:993–9.
Potts RO, Guy RH. A predictive algorithm for skin permeability: the effects of molecular size and hydrogen bond activity. Pharm Res. 1995;12:1628–33.
Pugh WJ, Degim IT, Hadgraft J. Epidermal permeability–penetrant structure relationships: 4,QSAR of permeant diffusion across human stratum corneum in terms of molecular weight, H-bonding and electronic charge. Int J Pharm. 2000;197:203–11.
Menczel E, Goldberg S. pH effect on the percutaneous penetration of lignocaine hydrochloride. Dermatologica. 1978;156:8–14.
Wiechers JW, Watkinson AC, Cross SE, Roberts MS. Predicting skin penetration of actives from complex cosmetic formulations: an evaluation of inter formulation and inter active effects during formulation optimization for transdermal delivery. Int J Cos Sci. 2012;34:525–35.
Lind M, Nielsen KT, Schefe LH, Nørremark K, Eriksson AH, Norsgaard H, et al. Supersaturation of Calcipotriene and betamethasone dipropionate in a novel aerosol foam formulation for topical treatment of psoriasis provides enhanced bioavailability of the active ingredients. Dermatol Ther. 2016;6:413–25.
Cilurzo F, Gasiraghi A, Selmin F, Minghetti P. Supersaturation as a tool for skin penetration enhancement. Curr Pharm Design. 2015;21:2733–44.
Kondo S, Yamasaki-Konishi H, Sugimoto I. Enhancement of transdermal delivery by superfluous thermodynamic potential. II. In vitro–in vivo correlation of percutaneous Nifedipine transport. J Pharmacobio-Dyn. 1987;10:587–94.
Coldman MF, Poulsen BJ, Higuchi T. Enhancement of percutaneous absorption by the use of volatile: nonvolatile systems as vehicles. J Pharm Sci. 1969;58:1098–102.
Higuchi T. Physical chemical analysis of percutaneous absorption process from creams and ointments. J Soc Cos Chem. 1960;11:85–97.
Zai H, Maibach HI. Effects of skin occlusion on percutaneous absorption: an overview. Skin Pharmacol Appl Ski Physiol. 2001;14:1–10.
Franz TJ. Percutaneous absorption. On the relevance of in vitro data. J Invest Dermatol. 1975;64:190–5.
Kligman AM, Christophers E. Preparation of isolated sheets of human stratum corneum. Arch Dermatol. 1963;88:702–5.
Sjövall P, Greve T, Clausen SK, Moller K, Eirefelt S, Johansson B, et al. Imaging of distribution of topically applied drug molecules in mouse skin by combination of time-of-flight secondary ion mass spectrometry and scanning electron microscopy. Anal Chem. 2014;86:3443–52.
Prideaux B, Atkinson SJ, Carolan VA, Morton J, Clench MR. Sample preparation and data interpretation procedures for the examination of xenobiotic compounds in skin by indirect imaging MALDI-MS. J Mass Spectrom. 2007;260:243–51.
Turker SD, Dunn WB, Wilkie J. MALDI-MS of drugs: profiling, imaging, and steps towards quantitative analysis. App Spec Rev. 2016;52:73–99.
Castellino S, Groseclose MR, Wagner D. MALDI imaging mass spectrometry: bridging biology and chemistry in drug development. Bioanalysis. 2011;3:2427–42.
Wenande E, Olesen UH, Nielsen MMB, Janfelt C, Hansen SH, Anderson RR, et al. Fractional laser-assisted topical delivery leads to enhanced, accelerated and deeper cutaneous 5-fluorouracil uptake. Expert Opin Drug Del. 2017;14:307–17.
Taudorf EH, Lerche C, Vissing A, Philipsen PA, Hannibal J, D'Alvise UJC, et al. Topically applied methotrexate is rapidly delivered into skin by fractional laser ablation. Expert Opin Drug Del. 2015;12:1059–69.
D’Alvise J, Mortensen RW, Hansen SH, Janfelt C. Detection of follicular transport of Lidocaine and metabolism in adipose tissue in pig ear skin by DESI mass spectrometry imaging. Anal Bioanal Chem. 2014;406:3735–42.
Nilson A, Goodwin RJA, Shariatgorji M, Vallianatou T, Webborn PJH, Andrèn A. Mass spectrometry imaging in drug development. Anal Chem. 2015;87:1437–55.
White RE, Manitpisitkul P. Pharmacokinetic theory of cassette dosing in drug discovery screening. ASPET. 2001;29:957–66.
Berman J, Halm K, Adkison K, Shaffer J. Preclinical drug metabolism in the age of high-throughput screening: an industrial perspective. J Med Chem. 1997;40:827–9.
Fick LW, Adkison KL, Wells-Knecht KJ, Woolard P, Higton DM. Cassette dosing: rapid in vivo assessment of pharmacokinetics. Pharm Sci Technol To. 1998;1:12–8.
Allen MC, Shah TS, Day WW. Rapid determination of oral pharmacokinetics and plasma free fraction using cocktail approaches: methods and application. Pharm Res. 1998;15:93–7.
Poksch JW, Ward KW. Cassette dosing pharmacokinetic studies for evaluation of ophthalmic drugs for posterior ocular diseases. J Pharm Sci. 2008;97:3411–21.
Seto Y, Inoue R, Ochi M, Gandy G, Ymada S, Onoue S. Combined use of in vitro phototoxic assessments and cassette dosing pharmacokinetic study for phototoxicity characterization of Fluoroquinolones. AAPS J. 2011;13:482–92.
Ohtake H, Suzuki Y, Kato M, Seto Y, Onoue S. Photosafety testing of dermally-applied chemicals based on photochemical and cassette-dosing pharmacokinetic data. Asian J Pharm Sci. 2016;11:237–8.
Seto Y, Ohtake H, Kato M, Onoue S. Phototoxic risk assessments on benzophenone derivatives: photobiochemical assessments and dermal cassette-dosing pharmacokinetic study. J Pharmacol Exp Ther. 2015;354:195–202.
Felding J, Sørensen MD, Poulsen TD, Larsen J, Anderson C, Refer P, et al. Discovery and early clinical development of 2-{6-[2-(3,5-dichloro-4-pyridyl)acetyl]-2,3-dimethoxyphenoxy}-N-propylacetamide (LEO 29102), a soft-drug inhibitor of phosphodiesterase 4 for topical treatment of atopic dermatitis. J Med Chem. 2014;57:5893–903.
LEO 29102 Single and Multiple Dose Study By Dermal Application, NCT00891709. http://www.ClinicalTrials.gov
LEO 29102 Cream in the Treatment of Atopic Dermatitis, NCT01037881. http://www.ClinicalTrials.gov
Gutfreund K, Bienias W, Szewczyk A, Kaszuba A. Topical calcineurin inhibitors in dermatology. Part I: properties, method and effectiveness of drug use. Postep Derm Alergol. 2013;30:165–9.
Tafacitinib. DrugsRD. 2010;10:271–84.
Bachelez H, van de Kerkhof PCM, Strohal R, Kubanov A, Valenzuela F, Lee JH, et al. Tofacitinib versus etanercept or placebo in moderate-to-severe chronic plaque psoriasis: a phase 3 randomised non-inferiority trial. Lancet. 2015;386:552–61.
Mesa RA, Yasothan U, Kirkpatrick P. Ruxolitinib. Nat Rev Drug Disc. 2012;11:103–4.
Kofoed K, Skov L, Zachariae C. New drugs and treatment targets in psoriasis. Acta Derm Venereol. 2015;95:133–9.
Williams AC, Barry BW. Penetration enhancers. Adv Drug Deliv Rev. 2012;64:128–37.
Bouschen W, Schulz O, Eikel D, Spengler B. Matrix vapor deposition/recrystallization and dedicated spray preparation for high-resolution scanning microprobe matrix-assisted laser desorption/ionization imaging mass spectrometry (SMALDI-MS) of tissue and single cells. Rapid Commun Mass Spectrom. 2010;24:355–64.
Schramm T, Hester A, Klinkert I, Both JP, Heeren RMA, Brunelle A, et al. imzML—a common data format for the flexible exchange and processing of mass spectrometry imaging data. J Proteome. 2012;75:5106–10.
Robichaud G, Garrard KP, Barry JA, Muddiman DC. MSiReader: an open-source interface to view and analyze high resolving power MS imaging files on Matlab platform. J Am Soc Mass Spectrom. 2013;24:718–21.
Lipinski C, Lombardo F, Dominy BW, Feeney PJ. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv Drug Deliv Rev. 1997;23:3–25.
Acknowledgements
We acknowledge Tina Leonhardt Hjort for her expert technical assistance with skin penetration studies, Ida Seeger for her expert technical assistance with the production of the formulations, Liselotte Saustrup Kirk and Karina Juul Kristensen for their expert technical assistance with the UHPLC-MS/MS bioanalysis of the biopsies and the culture media, and Christa Ancher Marvig for determination of the log D values.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
The study involved anonymized human skin samples from abdominoplasty surgery acquired from Biopredic International, France upon written informed consent of the donor.
Ethical approval
According to the Danish Committee Act section 14.3, anonymous human biological material used in health research projects shall not seek ethical approval as long as the collected human biological material has been collected lawfully in the country of origin which is the case. The supplier of the human biological material holds a permit granted by the French Ministry of Higher Education and Research for the acquisition, transformation, sales, and export of human biological material to be used in research, and is furthermore in compliance with the French law CSP1245-2
Electronic supplementary material
ESM 1
(PDF 317 kb)
Rights and permissions
About this article
Cite this article
Sørensen, I.S., Janfelt, C., Nielsen, M.M.B. et al. Combination of MALDI-MSI and cassette dosing for evaluation of drug distribution in human skin explant. Anal Bioanal Chem 409, 4993–5005 (2017). https://doi.org/10.1007/s00216-017-0443-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-017-0443-2