Abstract
Summary
Bone material properties were assessed using impact microindentation in patients with high-energy trauma fractures. Compared to patients with low-energy trauma fractures, bone material strength index was significantly higher in patients with high-energy trauma fractures, and did not differ between patients with osteopenia and those with osteoporosis within each trauma group.
Introduction
Impact microindentation (IMI) is a technique to assess tissue-level properties of bone at the tibia. Bone material strength index (BMSi), measured by IMI, is decreased in patients with low-energy trauma fractures, independently of areal bone mineral density (aBMD), but there is no information about BMSi in patients with high-energy trauma fractures. In the present study, we evaluated tissue-level properties of bone with IMI in patients with high-energy trauma fractures.
Methods
BMSi was measured 3.0 months (IQR 2.0–5.8) after the fracture in 40 patients with high-energy trauma and 40 age- and gender-matched controls with low-energy trauma fractures using the OsteoProbe® device.
Results
Mean age of high- and low-energy trauma patients was 57.7 ± 9.1 and 57.2 ± 7.7 years, respectively (p = 0.78). Fracture types were comparable in high- vs low-energy trauma patients. Lumbar spine (LS)-aBMD, but not femoral neck (FN)-aBMD, was higher in high- than in low-energy trauma patients (LS 0.96 ± 0.13 vs 0.89 ± 0.13 g/cm2, p = 0.02; FN 0.75 ± 0.09 vs 0.72 ± 0.09 g/cm2, p = 0.09). BMSi was significantly higher in high- than in low-energy trauma patients (84.4 ± 5.0 vs 78.0 ± 4.6, p = 0.001), also after adjusting for aBMD (p = 0.003). In addition, BMSi did not differ between patients with osteopenia and those with osteoporosis within each trauma group.
Conclusion
Our data demonstrate that BMSi and LS-aBMD, but not FN-aBMD, are significantly higher in high-energy trauma patients compared to matched controls with similar fractures from low-energy trauma. Further studies of non-osteoporotic patients with high-energy trauma fracture with measurements of BMSi are warranted to determine whether IMI might help in identifying those with reduced bone strength.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures following severe physical trauma are typically excluded from most studies of the prevalence or the incidence of osteoporotic fractures or from efficacy outcomes in clinical intervention trials of subjects at increased risk for fractures [1,2,3]. However, observational studies reported that subjects with prior high-energy trauma fractures had similar areal bone mineral density (aBMD) values as subjects with prior low-energy trauma fractures and lower aBMD values than subjects without fractures [4, 5]. This raised the possibility of a common, aBMD-related, pathogenetic mechanism of high- and low-energy trauma fractures. It was recommended that classification of fractures as high or low-trauma and fragility — or any other terms that suggest a rating of trauma — should be abandoned, and all types of fractures should be evaluated and treated without regard to trauma [5, 6].
In an analysis of two large prospective cohorts of women and men [6], the risk of a future high-energy trauma fracture was increased only among individuals with osteoporosis (baseline aBMD T-score ≤ − 2.5 SD) but not among women or men with osteopenia (baseline aBMD T-score between − 1.0 SD and − 2.5 SD), and the rate of future high-energy trauma fractures was considerably lower than that of low-energy trauma fractures. In addition, high-energy trauma fractures were, contrary to low-energy trauma fractures, not associated with increasing age or mortality [6]. These findings suggest that determinants of bone fragility other than aBMD may be different between subgroups of subjects with high-energy trauma fractures and also between subjects with high- and subjects with low-energy trauma fractures.
Fractures occur when the loads applied to bone exceed its strength which is determined by the amount of bone (i.e., size or mass), the spatial distribution of bone mass (i.e., shape and architecture), and the intrinsic properties of the materials that comprise the bone [7]. Bone microarchitecture (both cortical and trabecular) can be assessed in vivo by high-resolution peripheral computed tomography (HR-pQCT) [8]. A recent large, prospective study of women and men at least 40 years of age reported that indices measured by HR-pQCT improved prediction of fractures beyond femoral neck aBMD and the fracture risk assessment tool FRAX [9]. Fractures included in this report were, however, mostly low-energy trauma (67%), but traumatic fractures (19%) were also included.
Bone material properties are the least understood and hardest to evaluate determinant of bone strength. Impact microindentation (IMI) is a relatively new reference point indentation technique that measures tissue-level properties of bone in humans in vivo [10]. IMI is performed with the handheld device OsteoProbe® that imparts a single impact load to the bone surface and is approved for use at the tibia. By driving the probe into the bone surface, the resistance of bone tissue to a given mechanical challenge can be measured as bone material strength index (BMSi) [11]. Although measured at a cortical site, low BMSi was associated with increased bone fragility at all relevant skeletal sites, vertebral, non-vertebral, and hip sites, in individuals with low-energy trauma fractures [12,13,14]. There is, however, no information about bone material properties in patients with high-energy trauma fractures. The aim of this study was to evaluate bone material properties, measured by IMI, in subjects with high-energy trauma fractures to test the hypothesis that BMSi might differ between subjects with high- and subjects with low-energy trauma fractures.
Patients and methods
Patients
This was a cross-sectional study of women and men, aged 40 to 85 years, with high-energy trauma fractures recruited from the fracture liaison service (FLS) and the outpatient clinic of the Center for Bone Quality of the Leiden University Medical Center who consented to measurement of BMSi by OsteoProbe®. Subjects were matched for gender and age with patients with low-energy trauma fragility fractures investigated in the same center during the same period who served as controls; aBMD, measured by dual-energy X-ray absorptiometry (DXA), was not a selection criterion in either group of subjects with fractures. Exclusion criteria for both groups were a metabolic bone disease other than osteoporosis, use of any treatment affecting bone metabolism except calcium and vitamin D, immobilization, and inability to provide informed consent. Patients were also excluded if there was a contraindication for IMI measurement (systemic infection, severe obesity, or allergy to local anesthetic used). If there was local skin or bone lesions of the tibia, prior fracture of the tibia or local edema, the contralateral tibia, if free of problems, was used [15]. The study was approved by the Medical Ethics Committee of the LUMC, and written informed consent was obtained from all study participants.
Methods
Full medical history, clinical risk factors for fracture, and details of the conditions associated with the presenting fracture were documented in all studied subjects. A high-energy trauma fracture was defined as any fracture caused by major trauma (e.g., fall from height > 2 m, motor vehicle accidents, high-speed biking, and skiing injuries). A low-energy trauma fracture was defined as any fracture following a fall from standing height or less. All fractures were radiographically confirmed; of the vertebral fractures, only grade 2 or higher [16] was considered.
The 10-year probability (FRAX) for a major osteoporotic fracture and for a hip fracture was calculated using reference values for the Dutch population [17]. Presenting fractures were not included as previous fractures in the calculation of the FRAX.
Laboratory measurements
Serum calcium (albumin-corrected) and creatinine concentrations and alkaline phosphatase activity were measured by semiautomated techniques. Plasma intact parathyroid hormone (PTH) was measured by the IMMULITE 2500 (Siemens Diagnostics, Breda, the Netherlands) and serum 25-hydroxyvitamin D (25-OH D) concentrations by the 25-OH-vitamin D TOTAL assay (DiaSorin D.A./N.V., Brussels, Belgium).
Bone mineral density
Areal BMD was measured at the lumbar spine (L1-L4) and at the left and right hip by DXA with Hologic QDR Discovery A (Hologic, Bedford, MA, USA). Average aBMD values of the hip were used in the analysis. NHANES III reference values compatible with reference values of the Dutch population were used to calculate T-scores [18]. Osteopenia and osteoporosis were diagnosed according to the World Health Organisation (WHO) criteria with osteopenia defined as a T-score of < − 1.0 SD but > − 2.5 SD at either the lumbar spine or femoral neck and osteoporosis as a T-score of ≤ − 2.5 SD below the young female adult mean [19].
Impact microindentation
Bone material strength index was measured in all patients by impact microindentation using the handheld microindenter device (OsteoProbe® RUO, Active Life Scientific, CA, USA) on the midshaft of the tibia as previously described [20]. In brief, the patient was placed in supine position with the tibia in external rotation to orient the flat surface of the medial tibia diaphysis in a horizontal position. The measurement site was defined as the mean distance between the medial malleolus and the distal apex of the patella. Following disinfection of the area and local anesthesia of the skin and periosteum with lidocaine 1%, the test probe was gently inserted in the skin (without skin incision) until the bone surface was reached. Usually, one skin piercing is enough to perform all indentations without pulling the indenter out of the skin. In the very rare occasion that the skin is tough (for instance in young individuals), a second skin piercing may be necessary to prevent the probe from suffering lateral tension by the skin itself that might interfere with the measurement. Each time the skin is pierced, the new first measurement is discarded. After at least five adequate measurements, five additional measurements were performed on a polymethylmethacrylate (PMMA) calibration phantom [12, 20,21,22,23]. BMSi was calculated by the corresponding computer software. Measurements were performed by three experienced operators. The intra-observer and interobserver coefficient of variation (CV) was 2.2% and 1.6%, respectively.
Statistical analysis
Data were tested for normality using Shapiro–Wilk test and visually with histograms. A paired t-test was used to test between-group differences in BMSi and aBMD. Between-group differences in baseline characteristics were assessed using a paired t-test or Wilcoxon signed-rank test and McNemar’s test for normally and not normally distributed continuous and for categorical variables, respectively. Correlations between BMSi and aBMD values or patients’ parameters were examined by Pearson’s and Spearman’s tests for normally and not normally distributed variables, respectively. Conditional logistic regression was used to assess BMSi values adjusted for aBMD to compare BMSi values between high- and low-energy trauma patients. Analysis of variance models with BMSi as outcome variable adjusted for age were used to compare BMSi values between high-energy trauma patients with different DXA diagnoses (normal aBMD, osteopenia, and osteoporosis). Assuming a standard deviation of 5.0 and a difference in BMSi of 3.5 based on an earlier study from our group in patients with and without fragility fractures [12], the sample size to detect a clinically significant difference in BMSi between groups with a power of 0.8 at a significance level of 0.05 is 33. A p-value < 0.05 was considered to be statistically significant. All analyses were performed using SPSS software for Windows (version 25.0; SPSS Inc., Chicago, IL, USA), and graphs were constructed with GraphPad Prism (version 8.0; GraphPad software Inc., La Jolla, CA, USA).
Results
Forty patients (70.0% men) with high-energy trauma fractures and 40 control patients (70.0% men) with low-energy trauma fractures were included in the study. Median time to inclusion after sustaining a high- or a low-energy trauma fracture was comparable between both groups [3.0 months (IQR (interquartile range) 2.0–5.8 months) and 3.0 months (IQR 1.0–5.8 months), respectively (p = 0.899)]. Mechanisms of injury in high-energy trauma patients were high-speed biking injury (n = 14), fall from height > 2 m (n = 11), car crash (n = 9), and skiing injury (n = 5); one patient fractured his forearm by a heavy industrial machine.
Patients’ characteristics and laboratory measurements are shown in Table 1. By design, there were no differences in age and gender between the two groups, and BMI values were comparable. Multiple fractures were more common in high-energy trauma patients (n = 16 versus n = 5 in low-energy trauma patients, p = 0.005), but the sites of fracture in individual patients were similar: clinical vertebral fracture, 10 high- versus 11 low-trauma patients, p = 0.799; hip fracture, 3 high- versus 4 low-trauma patients, p = 1.00; and non-hip non-vertebral fracture, 31 high- versus 25 low-trauma patients, p = 0.143.
Lumbar spine aBMD (LS-aBMD), but not femoral neck aBMD (FN-aBMD), was significantly higher in high-energy trauma patients (Table 1). In this group, 10 patients (25%) had normal aBMD values, 23 (57.5%) had osteopenia, and 7 (17.5%) had osteoporosis. The corresponding numbers in the low-energy trauma group were 3 (7.5%), 23 (57.5%), and 14 (35.0%). Thus, significantly more patients in the high-energy trauma group had normal aBMD values (p = 0.047), but the number of patients with a diagnosis of osteoporosis/osteopenia did not differ between the two groups (osteoporosis p = 0.075, osteopenia p = 1.00).
BMSi values of all patients studied were not different between men and women (81.1 ± 6.3 vs 81.3 ± 4.2, p = 0.932) but did negatively correlate with FRAX (without aBMD) for both major and a hip fracture (r = − 0.257, p = 0.022, and r = − 0.308, p = 0.006, respectively) and with age (r = − 0.277, p = 0.013; r = − 0.362, p = 0.022 in high-energy trauma patients only). There was no significant relationship between BMSi values and LS-aBMD (r = 0.093, p = 0.413; r = − 0.269, p = 0.097 in high-energy trauma patients only), FN-aBMD (r = 0.079, p = 0.489; r = 0.045, p = 0.781 in high-energy trauma patients only), or BMI (r = − 0.205, p = 0.068).
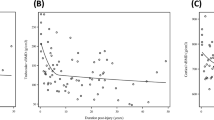
High-energy trauma patients had significantly higher BMSi values compared with low-energy trauma patients, 84.4 ± 5.0 versus 78.0 ± 4.6, p = 0.001 (Fig. 1A), also after adjusting for aBMD (p = 0.003). BMSi values did not differ between patients with osteopenia and those with osteoporosis within high-energy trauma patients (Fig. 1B). In addition, BMSi values did not differ between patients with osteopenia and those with osteoporosis within low-energy trauma patients, being constantly lower in low- than in high-energy trauma patients (Table 2), also after adjusting for age (osteopenia p < 0.001, osteoporosis p = 0.002). In the high-energy trauma group, there was no difference in BMSi values between patients with multiple fractures (range 2 to 13 fractures, n = 16) and those with only one fracture (n = 24), 84.4 ± 4.8 versus 85.0 ± 5.1, p = 0.733. In the low-energy trauma group, the number of patients with multiple fractures was too small for a similar statistical analysis.
Bone material strength index (BMSi) in A patients with high-energy trauma and low-energy trauma fractures and B in high-energy trauma patients with a dual-energy x-ray absorptiometry diagnosis of osteoporosis, osteopenia, and normal aBMD. Data are shown in box-whisker plots, and statistical differences are displayed for BMSi. Boxes indicate median and interquartile range. Bars indicate minimum and maximum values. *p = 0.001
Discussion
We show that BMSi values, measured by IMI, are significantly higher in subjects with high-energy trauma fractures than in gender- and age-matched subjects with low-energy trauma fractures and comparable with those previously reported in subjects without fracture [12, 21]. The design and size of our study allowed precise evaluation of the severity of injury, and we included only subjects with documented severe trauma in the high-energy trauma group; notably, aBMD was not a selection criterion or a prerequisite for inclusion in the study. More men than women were studied, but there was no difference in BMSi values between males and females. Moreover, the sites of fractures, including the spine and the hip, were similar between subjects with high- and low-energy trauma, but multiple fractures were more common in subjects with high-energy trauma.
To date, this is the first study that addresses the question of the effects of loads on bone material properties and fragility in humans in vivo by evaluating BMSi in subjects with high-energy trauma fractures and comparing them to those of subjects with low-energy trauma fractures. Studies comparing BMSi values between subjects with low-energy trauma fractures and subjects without fractures have generally shown significantly lower values in the former [12, 13, 21, 24]. Different from these observations, however, a Swedish cohort of women aged 75 to 80 years reported similar BMSi values in women with and without fractures [25]. In that study, all fractures irrespective of trauma type were included, and information about fractures was obtained retrospectively. In view of the results of the present study, inclusion of subjects with high-energy trauma fractures, and presumably higher BMSi values, may have contributed to the lack of difference in BMSi between the two groups in that analysis.
The finding that BMSi values were not decreased in most subjects with high-energy trauma fractures raises questions about the mechanism of fracture in such subjects. Fractures occur when the load applied to bone exceeds its strength. The major measurable determinants of bone strength in humans in vivo are the amount of bone mineral and mass, the bone size, geometry and architecture, and the bone material composition [26]. Recent studies of the relationship between BMSi values and bone material properties that affect bone strength — measured by microspectroscopy (Raman, FITRI) in bone biopsies obtained concurrently with BMSi measurements — showed that BMSi assesses material properties of cortical bone [27, 28]. BMSi values are strongly associated with the mineral to matrix ratio (MM), the most widely measured bone material property, that, differently from other measurements of mineral density, directly measures and accounts for the amount of organic matrix in the volume analyzed [29]. In rodents, MM correlates with ash weight and is directly proportional to bending stiffness and failure moment being superior to total mineral density, measured by micro CT, in predicting bone strength [30, 31]. As reported here, material properties of cortical bone are negatively related with age and the 10-year fracture probability assessed by FRAX (without aBMD) [32]. Thus, our results showing that bone tissue properties are not impaired in subjects with fractures due to high-energy trauma suggest that the excessive load applied to bone is likely responsible for most of the fractures under these conditions. This is further supported by our finding that BMSi values were comparable between patients with multiple fractures and those with a single fracture. In order, however, to better define the contribution of bone material properties to the susceptibility to high-energy trauma fractures, it is necessary to put this conclusion in context with the known important determinants of fracture risk, aBMD, and age.
In agreement with some, but not all, reports [4,5,6], subjects with high-energy trauma fractures had significantly higher LS-, but not FN-aBMD, and more subjects had normal aBMD values compared to those with low-energy trauma fractures. In addition, and consistent with earlier reports [12, 21], we found no association between BMSi and aBMD values but between BMSi and age. These findings were also present in the group of high-energy trauma patients. Furthermore, BMSi values were similar in subjects with osteopenia and osteoporosis within each trauma group. Observational studies of large cohorts of women and men have shown that subjects with incident fractures had, as expected, lower aBMD values than non-fractured controls that were, however, not different between subjects with high- and those with low-energy trauma fractures [4,5,6]. Together with difficulties to quantify the force of trauma in clinical practice, these observations led to the recommendation to stop classifying fractures as high- and low-energy trauma and care for all patients with fractures in the same way and independently of the severity of the injury associated with the fracture [33]. Mackey et al. [6] showed that among men and women ≥ 65 years of two large prospective US cohorts (Study of Osteoporotic Fractures (SOF) and Osteoporotic Fractures in Men Study (MrOs)), the incidence of high-energy trauma nonspine fractures increased significantly in subjects with osteoporosis (aBMD T-scores ≤ − 2.5 SD), and prevalence of osteoporosis was similar between subjects with high- and low-energy trauma fractures (36.2% vs 36.6% in women and 12.8% vs 14.8% in men). Therefore, subjects with osteoporosis were at high risk of fracture independently of the initiating trauma underscoring the importance of aBMD measurements in the assessment of all patients presenting with nonspine fractures. Although the prevalence of osteoporosis in our study needs to be interpreted with caution due to the small sample size, our findings are in line with this conclusion as 17.5% of subjects (predominantly men, approximately 20 years younger than those of the study of Mackey et al.) with high-energy trauma fractures had osteoporosis, a prevalence much higher than would have been expected in individuals of the same age in the general population [34]. Thus, a substantial number of relatively younger individuals (mean age 57 years) with high-energy trauma fractures was osteoporotic. In contrast, however, to the findings of the SOF and MrOs studies, the prevalence of osteoporosis in subjects with low-energy trauma fractures in our study was significantly higher (35%). Moreover, in the study of Mackey et al. in both men and women with osteopenia (T-scores between < − 1 SD and > − 2.5 SD), the adjusted incidence of traumatic fractures was not elevated compared to that of non-fractured subjects whereas the incidence of low-energy trauma fractures was. The incidence of traumatic fractures was further not related with age as was the case in subjects with low-energy trauma fractures. These observations combined raise questions about the effects of differences among subjects included in studies of different designs on clinical outcomes, but also of prevalent bone-related factors, other than aBMD, that affect bone fragility; such differences should be considered before generalizing reported results to all subjects with high-energy trauma fractures.
A study conducted in trauma units in Austria reported the frequency of low- and high-energy trauma nonspine fractures over 13 years in more than 400,000 individuals of all ages [35]. The frequency of high-energy trauma fractures was much higher in the young and decreased with aging, while low-energy trauma fractures were much more frequent in older individuals. Importantly, the age at which an equal frequency of high- and low-energy trauma fractures was observed was 54 years in women and 70 years in men. In the absence of studies of fracture frequency following high-energy trauma, results of that study suggest that most observational studies tend to underestimate the frequency of high-energy trauma fractures particularly in younger individuals. Alternatively, differences in bone material properties may have contributed to observed differences in frequency of high- and low-energy trauma fractures particularly in subjects without osteoporosis, who constitute by far the largest number of fractures [36]. These hypotheses need, however, to be tested in prospective studies.
Related to these considerations is the important observation that a previous high-energy trauma fracture increases the risk of a new incident fracture in the same way as a low-energy trauma fracture does [5, 6, 37, 38]. Incident fractures after a high-energy trauma fracture represent, however, a minority of subsequent fractures (5.5% in the study of Leslie et al.). In addition, they occur mainly in older individuals, more likely to have osteoporosis, but not in individuals younger than 65 years in whom only a previous low-energy trauma fracture increased significantly the risk of subsequent fractures.
Our study, the first to report IMI results in patients with fractures due to high-energy trauma, has strengths and limitations. Main strengths are the inclusion of treatment-naive subjects, the precise definition of the injury, and the a priori matching of the groups with high- and low-energy trauma fractures. Limitations include its cross-sectional design, the low number of participants that did not allow subgroup analyses, and the lack of a control group without fractures following a high-energy trauma. An additional limitation is a possible selection bias in the high- and low-energy trauma group. The former group might — due to the rapid and high loading event leading to such a fracture — more often be engaging in sporting activities and therefore reflect a more active population. A study by Sundh et al. suggested that exercise can increase BMSi [39]; thus, this group might have improved bone material properties compared to the general population. However, we did not include an activity questionnaire in the evaluation of subjects participating in the study, and this therefore can only be speculated.
In conclusion, our results demonstrate that bone material properties of patients with high-energy trauma fractures are higher than those of patients with low-energy trauma fractures and comparable with those previously reported in subjects without fractures. Further investigation in the measurement of BMSi in non-osteoporotic high-energy trauma fracture patients is warranted to determine whether IMI might help in identifying those with reduced bone strength.
Availability of data
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C, Trial F (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361:756–765
Bone HG, Dempster DW, Eisman JA, Greenspan SL, McClung MR, Nakamura T, Papapoulos S, Shih WJ, Rybak-Feiglin A, Santora AC, Verbruggen N, Leung AT, Lombardi A (2015) Odanacatib for the treatment of postmenopausal osteoporosis: development history and design and participant characteristics of LOFT, the Long-Term Odanacatib Fracture Trial. Osteoporos Int 26:699–712
Black DM, Thompson DE, Bauer DC, Ensrud K, Musliner T, Hochberg MC, Nevitt MC, Suryawanshi S, Cummings SR, Fracture IT (2000) Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. FIT Research Group. J Clin Endocrinol Metab 85:4118–4124
Sanders KM, Pasco JA, Ugoni AM, Nicholson GC, Seeman E, Martin TJ, Skoric B, Panahi S, Kotowicz MA (1998) The exclusion of high trauma fractures may underestimate the prevalence of bone fragility fractures in the community: the Geelong Osteoporosis Study. J Bone Miner Res 13:1337–1342
Leslie WD, Schousboe JT, Morin SN, Martineau P, Lix LM, Johansson H, McCloskey EV, Harvey NC, Kanis JA (2020) Fracture risk following high-trauma versus low-trauma fracture: a registry-based cohort study. Osteoporos Int. https://doi.org/10.1007/s00198-019-05274-2
Mackey DC, Lui LY, Cawthon PM, Bauer DC, Nevitt MC, Cauley JA, Hillier TA, Lewis CE, Barrett-Connor E, Cummings SR, Study of osteoporotic F, osteoporotic fractures in men study research G (2007) High-trauma fractures and low bone mineral density in older women and men. JAMA 298:2381–2388
Bouxsein ML (2005) Determinants of skeletal fragility. Best Pract Res Clin Rheumatol 19:897–911
Whittier DE, Boyd SK, Burghardt AJ, Paccou J, Ghasem-Zadeh A, Chapurlat R, Engelke K, Bouxsein ML (2020) Guidelines for the assessment of bone density and microarchitecture in vivo using high-resolution peripheral quantitative computed tomography. Osteoporos Int 31:1607–1627
Samelson EJ, Broe KE, Xu H, Yang L, Boyd S, Biver E, Szulc P, Adachi J, Amin S, Atkinson E, Berger C, Burt L, Chapurlat R, Chevalley T, Ferrari S, Goltzman D, Hanley DA, Hannan MT, Khosla S, Liu CT, Lorentzon M, Mellstrom D, Merle B, Nethander M, Rizzoli R, Sornay-Rendu E, Van Rietbergen B, Sundh D, Wong AKO, Ohlsson C, Demissie S, Kiel DP, Bouxsein ML (2019) Cortical and trabecular bone microarchitecture as an independent predictor of incident fracture risk in older women and men in the Bone Microarchitecture International Consortium (BoMIC): a prospective study. Lancet Diabetes Endocrinol 7:34–43
Schoeb M, Hamdy NAT, Malgo F, Winter EM, Appelman-Dijkstra NM (2020) Added value of impact microindentation in the evaluation of bone fragility: a systematic review of the literature. Front Endocrinol (Lausanne) 11:15
Bridges D, Randall C, Hansma PK (2012) A new device for performing reference point indentation without a reference probe. Rev Sci Instrum 83:044301
Malgo F, Hamdy NAT, Papapoulos SE, Appelman-Dijkstra NM (2017) Bone material strength index as measured by impact microindentation is low in patients with fractures irrespective of fracture site. Osteoporos Int 28:2433–2437
Sosa DD, Eriksen EF (2017) Reduced bone material strength is associated with increased risk and severity of osteoporotic fractures. An Impact Microindentation Study. Calcif Tissue Int 101:34–42
Rozental TD, Walley KC, Demissie S, Caksa S, Martinez-Betancourt A, Parker AM, Tsai JN, Yu EW, Bouxsein ML (2018) Bone material strength iindex as measured by impact microindentation in postmenopausal women with distal radius and hip fractures. J Bone Miner Res 33:621–626
Diez-Perez A, Bouxsein ML, Eriksen EF, Khosla S, Nyman JS, Papapoulos S, Tang SY (2016) Technical note: recommendations for a standard procedure to assess cortical bone at the tissue-level in vivo using impact microindentation. Bone Rep 5:181–185
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Lalmohamed A, Welsing PM, Lems WF, Jacobs JW, Kanis JA, Johansson H, De Boer A, De Vries F (2012) Calibration of FRAX (R) 3.1 to the Dutch population with data on the epidemiology of hip fractures. Osteoporos Int 23:861–869
Looker ACOE, Johnston CC Jr, Lindsay RL, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP (1997) Prevalence of low femoral bone density in older U.S. adults from NHANES III. J Bone Miner Res 12:1761–1768
Kanis JA (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. Osteoporos Int 4:368–381
Schoeb M, Malgo F, Peeters JJM, Winter EM, Papapoulos SE, Appelman-Dijkstra NM (2020) Treatments of osteoporosis increase bone material strength index in patients with low bone mass. Osteoporos Int 31:1683–1690
Malgo F, Hamdy NA, Papapoulos SE, Appelman-Dijkstra NM (2015) Bone material strength as measured by microindentation in vivo is decreased in patients with fragility fractures independently of bone mineral density. J Clin Endocrinol Metab 100:2039–2045
Malgo F, Hamdy NA, Rabelink TJ, Kroon HM, Claessen KM, Pereira AM, Biermasz NR, Appelman-Dijkstra NM (2017) Bone material strength index as measured by impact microindentation is altered in patients with acromegaly. Eur J Endocrinol 176:339–347
Malgo F, Hamdy NA, Papapoulos SE, Appelman-Dijkstra NM (2017) Impact microindentation: consistency of serial measurements and alterations in patients with Paget’s disease of the tibia. J Bone Miner Res 32:2375–2380
Rufus-Membere P, Holloway-Kew KL, Diez-Perez A, Kotowicz MA, Pasco JA (2019) Associations between bone impact microindentation and clinical risk factors for fracture. Endocrinology. https://doi.org/10.1210/en.2019-00415:en.2019-00415
Rudang R, Zoulakis M, Sundh D, Brisby H, Diez-Perez A, Johansson L, Mellstrom D, Darelid A, Lorentzon M (2016) Bone material strength is associated with areal BMD but not with prevalent fractures in older women. Osteoporos Int 27:1585–1592
Seeman E, Delmas PD (2006) Bone quality–the material and structural basis of bone strength and fragility. N Engl J Med 354:2250–2261
Rokidi S, Bravenboer N, Gamsjaeger S, Misof B, Blouin S, Chavassieux P, Klaushofer K, Paschalis E, Papapoulos S, Appelman-Dijkstra N (2020) Impact microindentation assesses subperiosteal bone material properties in humans. Bone 131:115110
Rokidi S, Bravenboer N, Gamsjaeger S, Chavassieux P, Zwerina J, Paschalis E, Papapoulos S, Appelman-Dijkstra N (2020) Impact microindentation measurements correlate with cortical bone material properties measured by Fourier transform infrared imaging in humans. Bone 137:115437
Paschalis EP, Gamsjaeger S, Klaushofer K (2017) Vibrational spectroscopic techniques to assess bone quality. Osteoporos Int 28:2275–2291
Donnelly E, Chen DX, Boskey AL, Baker SP, van der Meulen MC (2010) Contribution of mineral to bone structural behavior and tissue mechanical properties. Calcif Tissue Int 87:450–460
Boskey AL (1992) Mineral-matrix interactions in bone and cartilage. Clin Orthop Relat Res (281):244–74
Morgan EF, Unnikrisnan GU, Hussein AI (2018) Bone mechanical properties in healthy and diseased states. Annu Rev Biomed Eng 20:119–143
Cummings SR, Eastell R (2020) Stop (mis)classifying fractures as high- or low-trauma or as fragility fractures. Osteoporos Int. https://doi.org/10.1007/s00198-020-05325-z
Looker AC, Orwoll ES, Johnston CC Jr, Lindsay RL, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP (1997) Prevalence of low femoral bone density in older U.S. adults from NHANES III. J Bone Miner Res 12:1761–1768
Muschitz C, Kocijan R, Baierl A, Dormann R, Feichtinger X, Haschka J, Szivak M, Muschitz GK, Schanda J, Pietschmann P, Resch H, Dimai HP (2017) Preceding and subsequent high- and low-trauma fracture patterns-a 13-year epidemiological study in females and males in Austria. Osteoporos Int 28:1609–1618
Siris ES, Chen YT, Abbott TA, Barrett-Connor E, Miller PD, Wehren LE, Berger ML (2004) Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med 164:1108–1112
Johnell O, Oden A, Caulin F, Kanis JA (2001) Acute and long-term increase in fracture risk after hospitalization for vertebral fracture. Osteoporos Int 12:207–214
Melton LJ 3rd, Atkinson EJ, Cooper C, O’Fallon WM, Riggs BL (1999) Vertebral fractures predict subsequent fractures. Osteoporos Int 10:214–221
Sundh D, Nilsson M, Zoulakis M, Pasco C, Yilmaz M, Kazakia GJ, Hellgren M, Lorentzon M (2018) High-impact mechanical loading increases bone material strength in postmenopausal women-a 3-month intervention study. J Bone Miner Res 33:1242–1251
Acknowledgements
The authors thank R. Tsonaka, PhD, Department of Medical Statistics and Bioinformatics, Leiden University Medical Center, for her help in the statistical analysis of the results.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Medical Ethical Committee of the LUMC. All procedures performed were in accordance with the ethical standards of the Institutional Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Written informed consent was obtained from all individual participants included in the study.
Conflict of interest
Manuela Schoeb, Elizabeth M. Winter, Frank Malgo, Inger B. Schipper, and Robert J.P. van der Wal declare that they have no conflict of interest or disclosures. Socrates E. Papapoulos and Natasha M. Appelman-Dijkstra are unpaid members of the Scientific Board of Active Life Scientific, manufacturer of OsteoProbe®.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Schoeb, M., Winter, E.M., Malgo, F. et al. Bone material strength index as measured by in vivo impact microindentation is normal in subjects with high-energy trauma fractures. Osteoporos Int 33, 1511–1519 (2022). https://doi.org/10.1007/s00198-022-06368-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06368-0