Abstract
Summary
We estimated and characterized the imminent fracture risk (1–2 years) of high-risk fracture patients through a multinational (UK, Spain, Denmark) cohort study. Older individuals with newly diagnosed osteoporosis and individuals who had a fracture while on treatment with a bisphosphonate were at a high risk of imminent fracture.
Purpose
To characterize and estimate 1- to 2-year fracture risk in high-risk fracture patients.
Methods
Multi-cohort study in (database/study period) UK (CPRD/1995–2017), Spain (SIDIAP/2006–2016) and Denmark (DHR/1995–2016) including individuals ≥ 50 years old in NDO (newly diagnosed osteoporosis), OFx (incident osteoporotic fracture), BP (incident oral bisphosphonates use) or FWOT (fracture while on treatment with bisphosphonates). Outcomes (ICD-10/READ): hip, clinical spine, non-hip, non-spine and hip/humerus/distal forearm fracture. Follow-up: from cohort entry until death, migration/transfer or end of the study. Statistics: baseline characteristics and incidence rate (IR per 1000 persons).
Results (1-year IR)
NDO included 69,899 (UK), 37,901 (Spain) and 158,191 (Denmark) individuals. Spanish-IR was lowest for hip (4.7), clinical spine (2.5) and major osteoporotic fracture (MOF) (17.3) and highest in Denmark (74.2, 26.0 and 120.1, respectively). OFx included 83,514 (UK), 51,044 (Spain) and 509,551 (Denmark) individuals. IR in Denmark was highest for hip (24.1) and MOF (47.2), in Spain was highest for the clinical spine (9.4) and lowest for hip (9.5) and in the UK was lowest for the clinical spine (2.8) and MOF (20.7). BP included 148,507 (UK), 52,037 (Spain) and 204,010 (Denmark) individuals. Spanish-IR was lowest for hip (5.0) and MOF (21.1) and highest in Denmark (20.3 and 48.6, respectively). FWOT included 28,930 (UK), 1,865 (Spain) and 31,882 (Denmark) individuals. Clinical spine-IR was highest for Spain (12.0). Hip-IR was lowest for Spain (7.6) and highest for Denmark (33.6). Comparing young subjects, those who have FWOT started with an increased fracture rate.
Conclusion
OFx and FWOT individuals experience higher re-fracture incidence rates than those with osteoporosis with or without treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporotic fractures entail a social and economic burden for populations and health care systems worldwide [1]. Costs reached €37 billion in Europe already by 2010 [2]. In addition to societal costs, there is also the question of the individual implications of these fractures, such as an increased disability and mortality of the individuals affected [1]. Effective management centred on high fracture risk patients would improve outcomes and reduce the burden of fragility fractures.
In this context, the identification of the population at greater risk of fracture has been the focus of extensive research in the last decades. In recent years, particular attention has been drawn to the analysis of the imminent risk of fracture, defined as the markedly increased risk in the 2-year period that follows a fragility fracture [3,4,5,6,7,8,9].
Many risk factors for fracture have been identified; however, while some of them appear to confer an increased risk at any time (age [3,4,5, 7], previous falls [4, 8, 9], low bone mineral density [10], previous fractures and most specifically vertebral fractures [3, 5, 8, 9]), others (comorbidities [3,4,5], use of benzodiazepines [4, 5] or nitrates [8]) seem to have a significant impact in the short term.
Fracture risk can be quantified with risk assessment tools such as FRAX [11] and QFracture [12]. However, these tools focus on the 5- or 10-year future risk and are untested for imminent risk of fracture. Scaling risk to a different time period is more challenging than it may seem at first—risk factors might not remain constant over a 10-year period, with a higher risk of fracture during the first year after the index fracture. A population-based study carried out in postmenopausal women found a higher relative risk of fracture in the first year with a further decrease in the following years [13]. To design effective preventive strategies and help the early post-fracture management of affected individuals, it is therefore important to accurately identify the population with an imminent risk of fracture.
In this context, we aimed to characterize patients at high imminent risk of fracture and to estimate their 1- and 2-year risk of fracture. We considered a number of scenarios with an increased risk of fracture and selected appropriate cohorts for assessment. In the cohort of newly diagnosed osteoporosis, we sought to identify rates of imminent fracture in patients following their first assignment of an osteoporosis diagnosis. In the cohort of incident osteoporosis fracture, we focused on patients experiencing their first incident osteoporotic fracture and again focused on subsequent event rates for new fractures. In the cohort of incident oral bisphosphonates, we included incident users of oral bisphosphonate therapy, and in the cohort of incident fracture while on treatment with bisphosphonates, we selected patients with an incident fracture while using bisphosphonate treatment.
Materials and methods
We conducted a retrospective cohort study using data from three European electronic health care databases from the United Kingdom (UK), Denmark and Spain. The databases used were as follows:
-
(1)
The Clinical Practice Research Datalink (CPRD) from the UK, which contains anonymized and computerized primary care outpatient records for a representative sample of the UK population (> 7 million patients, approximately 8% of UK population) in addition to demographic information, medication prescriptions, clinical events, referrals and hospital admissions. Previous reports have demonstrated the availability and quality of CPRD [14]. For completeness and improved data quality, we linked CPRD to the Hospital Episode Statistics Admitted Patient Care, which contains clinical diagnoses during hospital admissions in England, to the Office for National Statistics mortality records and to the Index of Multiple Deprivation dataset.
-
(2)
The Sistema d’informació per al desenvolupament de la investigació en Atenció primaria (SIDIAP) which comprises primary health care anonymised electronic medical records for a representative > 80% of the population of Catalonia, as well as demographic information, clinical events (ICD10 codes), prescriptions and community pharmacy dispensations. Previous reports have demonstrated the availability and quality data of SIDIAP [15]. In order to avoid incomplete fracture records, we linked SIDIAP to regional hospital admissions data available for those hospitals part of the same trust/health care provider covering around 30% of the Catalan population (CMBD-AH ICS for its acronym in the Catalan language).
-
(3)
The Danish Health Registry (Lægemiddel-registret) [16], which contains all filled prescriptions in the country, is linked to the National Hospital Discharge Register (Landspatientsregistret—all diagnosis codes and treatments for inpatients and outpatients) and to the National Cause of Death Register (Dødsårsagsregistret). It represents the total Danish population, and previous reports have demonstrated the validity of the DHR database for epidemiological studies [17].
Participants
The source population for this study included individuals aged at least 50 years old at cohort entry, with at least 1 year of patient records available prior to inclusion.
The study period for CPRD was from 1 January 1995 to 31 January 2017; for SIDIAP from 1 January 2006 to 31 December 2016 and for DHR from 1 January 1995 to 31 December 2016. The study population included cohorts of individuals at potentially high fracture risk, as identified from the literature, divided into 4 cohorts (Online Resource 1).
Cohorts (non-exclusive)
-
(1)
NDO (newly diagnosed osteoporosis) patients with an incident recorded diagnosis of osteoporosis which might include those with or without a fracture (diagnosed through read codes or ICD-10 codes).
-
(2)
OFx (osteoporotic fracture) patients with a first incident fracture (all except face, skull and digits), diagnosed either through read codes or ICD-10 codes and without fracture coded at the same anatomical site in the prior 6 months.
-
(3)
BP (oral bisphosphonates use) incident users of oral bisphosphonates (ATC 05B*) without bisphosphonate use in the prior year.
-
(4)
FWOT (fracture while on treatment) patients with an incident fracture (as in the osteoporotic fracture cohort) while on treatment with oral bisphosphonates. This cohort was defined by a fracture diagnosed after bisphosphonate initiation and during continued therapy (with a gap of 90 days between dispensations allowed) and without fracture at the same site in the prior 6 months.
For a given individual, the date of entry into a cohort was defined as the index date (Table S2). Participants could potentially be present in more than one of the cohorts earlier, with different index dates.
Exclusion criteria
Individuals with Paget disease of bone and those with a history of breast or prostate cancer (at any time before the index date) were excluded. Furthermore, those with the use of any anti-osteoporotic drug (except Calcium and Vitamin D supplements) in the previous year were also excluded from the BP cohort.
Exposures, outcomes and covariates
All study variables (exposures, outcomes and covariates) were identified using pre-specified lists of diagnosis codes (ICD10, READ and ICD9) and medication codes (ATC and BNF/Prodcodes) (Online Resource 2).
The main study outcome was the first fracture of the hip, clinical spine, non-hip, non-spine and hip/humerus/distal forearm during the first and second years of follow-up. Any two fractures of the same bone/site coded within 6 months of each other were considered duplicate records, and the one recorded the latest was dismissed in regard to the primary outcome.
The aim of the aforementioned groups of outcomes is to capture all types of fractures; however, for clinical purposes, these groups are not practical. For this reason, we grouped the outcomes considered as ‘major osteoporotic fractures’ (MOF), which included fractures at the hip/humerus/distal forearm and clinical spine.
For each study outcome, patients were followed from the index date until the earliest of the study outcome, death, migration/transfer out and end of the study period (based on data availability at extraction date), whichever came first.
Covariates of interest included risk factors of fracture studied in the literature and those included in the QFracture [12] and FRAX [11] risk score calculators: age, sex, ethnicity, smoking status, alcohol drinking, diabetes mellitus, family history of osteoporosis/hip fracture, residence in a nursing/care home, previous history of distal forearm/spine/hip/shoulder fracture, history of falls, dementia, cancer, asthma or COPD, ischaemic heart disease, chronic liver disease, chronic kidney disease (stage 4+), Parkinson’s disease, rheumatoid arthritis or SLE, malabsorption and endocrine problems including thyrotoxicosis, hyperparathyroidism, Cushing’s, epilepsy or use of anticonvulsants, use of antidepressants, steroid tablets use, use of oestrogen or hormone replacement therapy body mass index, weight, height, any previous fracture, secondary osteoporosis, recent fracture (in the previous 6 months and 1 year), use of proton pump inhibitors, vitamin D deficiency, previously described predictors of imminent fracture and comorbidities: ankylosing spondylitis, anxiety disorders, Charlson co-morbidity index and medication: previous anti-osteoporosis drug use, heparin, beta-blockers, nitrates and calcium channel blockers.
In terms of the look-back period, we considered all medical history, e.g. if diabetes mellitus was ever diagnosed, it was coded ‘yes’. For smoking, drinking, BMI, nursing home, falls and medication, a look-back period of 1 year was used, given that the most recent recorded status would be the most correct at baseline. For fractures, a look-back period of 6 months, 1 year and ever before the index date (baseline) were all included.
Statistical analysis
Baseline demographics were reported. These included socio-economics, medical history and fracture risk factors stratified by cohort and country.
For each outcome, the 1-year and 2-year incidence rates were calculated. The incidence rate was defined as the number of events of the outcome of interest divided by the summation of patient years contributed by all patients in the cohort. Plots of the 1- and 2-year cumulative incidence (95% CI) function were also produced for each outcome.
Sub-group analysis
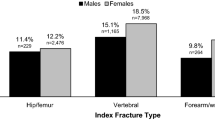
One-year incidence rates were also calculated for each of the following sub-groups: age groups, type of index fracture (hip and clinical spine fracture); and for the OBP cohort only, previous fracture history.
A common data dictionary was used to extract variables from all three databases, and a single R script was used to run the analyses in all three databases; all analyses were performed using RStudio version 1.1.380.
Results
NDO: newly diagnosed osteoporosis patients (with or without a fracture)
The NDO cohort consisted of a total of 69,899 from the CPRD database, 37,901 from the SIDIAP database and 158,191 individuals from the DHR database (Fig. 1).
Baseline characteristics of the population included are reported in Table 1. The proportion of men among these newly diagnosed patients was low, especially in Spain (8.6%). There were also pronounced differences in comorbidity between the countries with Denmark having the lowest proportion of individuals with > 3 points in the Charlson Comorbidity Index.
Overall, 1-year incidence rates of all individual fracture categories (Table 2) were highest in Denmark and lowest in Spain. The difference between the countries was observed for all fracture types but most pronounced for hip fractures, ranging from 4.7 to 74.2 per 1000 persons-years in Spain and Denmark, respectively.
The major osteoporotic fracture was created by adding the incidence rate of hip/humerus/distal forearm and clinical spine. The 1-year incidence rate of major osteoporotic fracture was highest for Denmark, followed by the UK and Spain (127.8, 33.4 and 17.3 per 1000 persons-year, respectively). One-year incidence rate per sex is depicted in the supplemental data (Online Resource 6); incidence rate of major osteoporosis fracture was greater in women in CPRD (16.3 vs 9.1 per 1000 persons-year in women and men, respectively) and in men in DHR (123.3 vs 150.1 per 1000 persons-year in women and men, respectively) with no significant differences found in SIDIAP.
The age-specific 1-year incidence of major osteoporotic fractures is reported in Fig. 2. While all three countries showed an increase in rates with increasing age, there were nation-specific differences, with the highest rates for Denmark compared to the UK and Spain. These differences were more pronounced between the youngest (subjects between 50 and 60 years old) and the oldest (subjects over 90 years old). Young Danish subjects had a double risk of suffering a fracture compared to subjects the same age in the UK or Spain, and the oldest Danish individuals had higher incidence rates of fracture (over 400 per 1000 persons-year) compared to the UK (75) and Spain (57).
The 2-year incidence rate of fracture is reported in Table 3. Incidence rates of all fracture categories remained highest for Denmark followed by the UK and Spain but were still lower than those found for the 1st year; the greatest reduction was found for Denmark, with approximately a 40% decrease in the incidence rates of hip and clinical spine fracture. The same was observed when grouping by major osteoporotic fracture (IR of 84.5, 28.8 and 15.4 for Denmark, the UK and Spain, respectively).
OFx: patients with a first incident fracture at osteoporotic sites
The OFx cohort consisted of a total of 83,514 from the CPRD database, 51,044 from the SIDIAP database and 509,551 individuals from the DHR database (Fig. 1).
UK individuals were on average 8 and 6 years older than the Danish and Spanish individuals, and there were fewer men (around 1 in 5 participants) compared to Denmark or Spain (about 1/3 in both); 9.6%, 15.7% and 4.5% patients in the UK, Spain and Denmark had an osteoporosis diagnosis.
Compared to the newly diagnosed osteoporosis cohort, individuals with an incident osteoporosis fracture had lower use of steroids and bisphosphonates and had an overall worse health status (Table 1).
The incidence rate for hip fracture was highest in Denmark (24.1 per 1000 persons-years) followed by the UK (18.1) and Spain (9.5); however, the opposite was found for clinical spine fractures which rates were highest in Spain (9.4 per 1000 persons-years) followed by Denmark (5.1) and the UK (2.8). The incidence rate of major osteoporotic fracture was highest for Denmark, followed by Spain and the UK (42.7, 38.3 and 20.7, respectively). The 1-year incidence rate of major osteoporosis fracture per sex is depicted in the supplemental data (Online Resource 6); incidence rate (per 1000 persons-year) was greater in women in SIDIAP (41.4 vs 30.8) and DHR (44.35 vs 36.8 in women and men, respectively) with no significant differences found in CPRD.
Age-specific 1-year incidence rates of major osteoporotic fracture (Fig. 3) increased similarly in Spain and Denmark and were both higher than the ones found for the UK, whose individuals had lower incidence rates in all age bands.
Regarding 2-year incidence rates of fracture (Table 3), overall, it was highest in Denmark, followed by the UK and Spain. Major osteoporotic fracture followed the same trend with incidence rates of 41, 30 and 24.9 in Denmark, Spain and the UK, respectively. Of note is the slight increase in the UK from the 1st year to the 2nd year (incidence rate of 20.3 to 24.9).
BP: new users of oral bisphosphonates
The BP cohort was formed by a total of 148,507 individuals from the CPRD database, 52,037 individuals from the SIDIAP database and 204,010 individuals from the DHR database (Fig. 1).
Danish and Spanish individuals in this cohort were 3 and 4 years younger than the UK individuals, and Spanish individuals had a lower proportion of steroid users compared to the other countries (Table 1); 16.3%, 25.4% and 34.0% patients in the UK, Spain and Denmark had an osteoporosis diagnosis. The mean time to fracture from index date was 181 days, 144 days and 141 days for the UK, Spain and Danish individuals, respectively.
The 1-year incidence rates of individual fracture categories were highest in Denmark followed by the UK and lowest in Spain (Table 2). When considering hip fractures, both the UK and Denmark had higher rates than the ones experienced by Spanish individuals. The incidence rate of clinical spine fractures in Denmark (8.3 per 1000 persons-year) doubled the ones found in the UK or Spain (4.3 in both countries). Overall, the 1-year rates of major osteoporotic fractures were highest for Denmark, followed by the UK and Spain (48.6, 31.3 and 21.1, respectively). The 1-year incidence rate of major osteoporosis fracture per sex is depicted in the supplemental data (Online Resource 6); incidence rate (per 1000 persons-year) was greater in women in SIDIAP (22.7 vs 14.1) and DHR (49.8 vs 43.4 in women and men, respectively) with no significant differences found in CPRD.
The age-specific 1-year risk of major osteoporotic fracture showed increasing IR with age and higher rates for Denmark followed by the UK and Spain (Fig. 3).
When stratifying this cohort depending on their previous fracture history (Online Resource 3), those who had a previous fracture had high incidence rates of major osteoporotic fracture in all countries and for subjects in the UK and Denmark higher incidence rates of the hip compared to clinical spine fracture.
Two-year IR (Table 3) of major osteoporotic fracture group was highest in Denmark and the UK than in Spain (40.1, 26.9 and 16.6 in Denmark, the UK and Spain, respectively).
FWOT: patients with incident fracture while on treatment with oral bisphosphonates
The FWOT study cohort composed a total of 28,930 from the CPRD database, 1,865 from the SIDIAP database and 31,882 individuals from the DHR database (Fig. 1).
As with the other three cohorts, Spanish patients were the youngest and had a lower proportion of men. Compared to Denmark, Spain and UK individuals had poorer health status, with 17% and 13% of individuals with a Charlson index 3+ respectively (Table 1); 47.8%, 52.9% and 50% of patients in the UK, Spain and Denmark had an osteoporosis diagnosis. The mean duration of bisphosphonate use from index date to incident fracture was 100.8, 43.7 and 61 days for the UK, Spain and Denmark, respectively.
As in subjects with an incident osteoporotic fracture, the 1-year incidence rate of hip fracture was higher in Denmark and lowest in Spain; however, this was not true for the clinical spine, where Spain had the highest incidence rates in this population. One-year IR of major osteoporotic fracture was highest in the UK followed by Denmark and Spain (51.9, 49.5 and 40.8, respectively). The 1-year incidence rate of major osteoporosis fracture per sex is depicted in the supplemental data (Online Resource 6); incidence rate (per 1000 persons-year) did not show significant differences between men and women.
The age-specific major osteoporotic fracture rates were very similar for all three countries up to the age of 90 years old, over which the Spanish individuals suffer a drop in their incidence rates reaching the lowest levels in this cohort probably influenced by the low number of individuals included in this age band (Fig. 3). Interestingly, the risk appeared much higher than in previous cohorts among the younger groups of 50 to 60 years of age: from 37 (Spain) to 44 per 1000 persons-years (UK and Denmark) for major osteoporotic fracture (Fig. 3).
Two-year incidence rates (Table 3) of hip fracture were highest in Denmark followed by the UK and Spain. However, similar rates of clinical spine fracture were demonstrated in all three countries.
Site of index fracture (OFx and FWOT)
OFx: incident osteoporotic fracture cohort
When analyzing data by the site of index fracture, in all countries, those who had an index hip fracture (Online Resource 4) or clinical spine fracture (Online Resource 5) had higher incidence rates of major osteoporotic fracture than of hip or clinical spine fractures.
Incidence rates of hip fracture were higher among individuals with an index clinical spine fracture compared with those with an index hip fracture.
FWOT: fracture while on treatment with bisphosphonates cohort
As in the incident osteoporotic fracture cohort, those who had index hip fracture had more frequently a subsequent major osteoporotic fracture and among these a second hip fracture (Online Resource 4). Those who had an index clinical spine fracture had more frequently a hip fracture in the UK and Denmark but had higher rates of clinical spine fracture in Spain (Online Resource 5).
Discussion
In this large multi-database and multinational cohort study, we report 1-year and 2-year fracture risk in four different cohorts: (1) newly diagnosed osteoporosis, (2) incident osteoporotic fracture, (3) incident use of oral bisphosphonates and (4) fractures while on treatment with oral bisphosphonates. The study highlights that at the end of the 1st and 2nd years, patients who fracture while on treatment are particularly prone to further major osteoporotic fractures; this is true for two of the three databases (SIDIAP and CPRD). For DHR, individuals at greater risk of major osteoporotic fractures are those with newly diagnosed osteoporosis. In accordance with the global epidemiology of osteoporosis, we consistently found an increased risk of fracture with increasing age, with relatively little difference in the age-risk gradient between the different cohorts. Of particular note is the highly elevated risk of fracture found especially among the younger individuals (50–60 years old) included in the fracture while on treatment cohort, which was twice that found in the same age category in the incident osteoporotic fracture cohort.
Fractures in Spain
The SIDIAP database is a primary health care population-based database. Overall, Spanish individuals were diagnosed and treated for osteoporosis at younger ages compared to the other countries.
Individuals who fractured while on treatment were older than the rest of cohorts in this country (mean age of 73 years) and had, as for the incident osteoporotic fracture cohort, poorer health status with a higher proportion of individuals with > 3 points in the Charlson Comorbidity Index (13.4% and 13.3% in the fracture while on treatment and incident osteoporotic fracture cohort, respectively). The majority of the index fractures in these cohorts were non-hip, non-spine.
In Spain, individuals who experienced the highest 1-year incidence rate of fracture and therefore at greater risk of major osteoporotic fractures were those who fractured while on treatment (40.8 per 1000 persons-year) followed by those who had had an incident osteoporotic fracture (38.3 per 1000 persons-year). The same is seen at the end of the 2nd year.
Fractures in the UK
The CPRD database is a primary health care population database. Individuals with an incident fracture and those who fractured while on treatment were older than the rest of the cohorts (mean age of 78–79 years old) and had poorer health status, with a higher proportion of individuals with > 3 points in the Charlson Comorbidity Index (17.6% and 11.9% for those who fractured while on treatment and the incident osteoporotic fracture cohort, respectively).
Regarding the previous fractures, 15.2% of the individuals with an incident diagnose of osteoporosis already had a fracture, and 8.3% of the individuals in the incident osteoporotic fracture cohort had already a previous fracture which is due to difficulties in accurately dating the history of previous fractures with the read codes used in CPRD.
When analysing the distribution of the index fractures in the incident osteoporotic fracture and fracture while on treatment cohort, 67.6% were hip in the incident osteoporotic fracture, while the majority of the index fractures in the fracture while on treatment cohort were non-hip, non-spine (65.5%).
In the UK, the highest 1 year incidence rates of major osteoporotic fractures are found among those who fractured while on treatment followed by those who had a new diagnose of osteoporosis (51.9 and 33.4 per 1000 py, respectively). The same is seen at the end of the 2nd year.
Fractures in Denmark
As in Spain and the UK, individuals who fractured while on treatment were older than the rest of the cohorts (mean age of 75 years old) and had poorer health status with a higher proportion of individuals with > 3 points in the Charlson Comorbidity Index, which was true for those with incident osteoporotic fracture and for those who fractured while on treatment but was especially relevant in this last group (2.9% and 2.2% for the fractures while on treatment and incident osteoporotic fracture cohort, respectively). The majority of the index fractures in the incident osteoporotic fracture and in the fracture while on treatment cohort were non-hip, non-spine. Incidence rates of fracture in Denmark were higher than in the two other countries, and as will be discussed in the succeeding text, the highest incidence rate of major osteoporotic fracture was found for those individuals with a newly diagnosed osteoporosis (127.8 per 1000 persons-year); this was true for the 1st- and 2nd-year IR.
Interpretation and comparison with other studies
The increased rate of fracture found, in all the countries, among individuals with a previous fracture (incident osteoporotic fracture and fracture while on treatment cohort) has been already described, regardless of the bisphosphonate adherence [18], and even among highly adherent individuals included in some randomized controlled trials of bisphosphonates [19, 20]. Fewer are the studies using real-world data; in 2014, a study based on the SIDIAP database reported an increased risk of fracture among bisphosphonate users (3.4% of these individuals fractured every year) with older age and previous fractures identified as risk factors [21], and another carried out in Denmark in 2016 found a higher incidence of subtrochanteric and femoral shaft fractures among highly adherent alendronate users after 13 years of treatment; however, further analysis justified this increase by the worse profile of risk factors among the older population rather than by a detrimental effect of alendronate [22]. As in these previous studies, in our study, individuals who fractured while on treatment in all the countries were older than the rest with poorer health status and higher comorbidity which could have contributed to the increased risk of fracture.
The difference in the rates of major osteoporotic fractures—highest in Denmark and lowest in Spain—likely reflect the already known geographical worldwide variation of fracture incidence with greater incidence rates of fracture in Northern Europe [23]. The reasons for this remain elusive and are beyond the scope of this paper but may include genetic differences including differences in body height and obesity, socio-economic differences, lifestyle habits, nutrition and even intrinsic differences in bone quality and bone geometry [24,25,26].
Age is an already known risk factor for fracture, and it is unsurprising that this also affects the immediate risk of major osteoporotic fractures [3, 4, 19, 27]. We found age-specific major osteoporotic fractures rates very similar between all the countries; however, we found that our youngest population, those aged 50–60 years old, started with an overall increased fracture rate (5 and 10 per 1000 per year). Nevertheless, these incident rates are still lower than what was found in a study carried out in Norway on this same age band (35 to 50 per 1000 persons-year) [28].
In the last years, there is a growing awareness of the importance of fracture prevention in the imminent fracture risk period. Our results show that the imminent fracture risk increased with age in all patients included (with or without a fracture) but was especially pronounced in those who had already fractured while on treatment with bisphosphonates. These subjects even those at younger ages were twice as likely to fracture compared to the rest of the cohorts; therefore, focusing the preventive strategies on these patients could help optimize the health care resources in each country. Future studies are needed to stratify the results per sex, or the Charlson Comorbidity Index and multivariate models’ analysis to assess the association between the imminent fracture risk and baseline characteristics in each of the cohorts would contribute to more accurately define the population at risk.
Strengths and limitations
To our knowledge, this is the first multinational and multi-database study that analyses the imminent risk of fracture in four different groups of individuals at risk using real-world data. The large number of individuals included and given the data gathered (routinely collected in primary care with hospital linkage) enables us to easily extrapolate our results. However, this study must also be interpreted in light of some limitations. First, there are differences in the number of individuals provided by each database for each cohort; in the incident osteoporotic fracture cohort, the DHR database contributed with 509,551 individuals, which is over sixfold higher compared to CPRD (83,514) and over ninefold higher compared to SIDIAP (55,304). Second, the different nature of the databases (Online resource 6), with CPRD and SIDIAP from primary care and DHR from hospital bases, renders comparison between them difficult. The DHR is a hospital-based database coupled with a nationwide prescription register that includes primary practice, compared to the primary care database of CPRD and SIDIAP. In some respects, it affects cohort definitions only as regards the newly diagnosed osteoporosis cohort where a small number of patients will be given an osteoporosis code in hospitals compared that with primary practice, selecting for a smaller and more severely affected population. This can also be reflected in the proportion of patients with a higher Charlson Comorbidity Index (> 3) which is similar in the newly diagnosed osteoporosis, in the fracture while on treatment with bisphosphonates and in the incident osteoporosis fracture cohort in Denmark suggesting a possible selection bias of a more severely affected population at baseline compared to what is found in the other countries, which would attenuate or confound the differences between the cohorts found with regard to fracture risk. As a minimum, the database differences will also affect the threshold for contacts with the health service, given that patients, in general, will have more contacts with primary practice than with hospital clinics, so the same patient is likely to achieve a higher Charlson score in a general practice database than in a hospital system database since some conditions do not require referral to specialists. By contrast and critical to the epidemiological value of the study, all three databases capture hospital-treated fractures, and all three databases are able to accurately capture initiation of osteoporosis treatment.
Third, among the incident fracture cohort, incident fractures were, as defined, the first fracture sustained in all Danish patients and in almost all patients in Spain. However, approximately 8% of the UK patients experienced a fracture previous to the inclusion in the cohort (Table 1); these patients’ fractures were found to be related to historical coding and were dismissed from the analysis. Fourth, the duration of the treatment of bisphosphonates in the incident bisphosphonate treatment cohort was not assessed, and therefore, we cannot exclude that the fracture rates reported could be partly due to a previous baseline risk of the patient (before the maximum effect of the bisphosphonate treatment). However, evidence suggests that the anti-fracture efficacy starts at the beginning of the treatment and reaches its maximum of 3 months after the initiation of the bisphosphonates [29]. In the worst-case, fracture rates in this cohort would be slightly lower, unlikely to affect our conclusions. Moreover, potential unknown discrepancies in coding could have taken place, leading to an under or overestimation of the fracture rates. There are also potential analytical discrepancies, which were minimized by the use of a single standardized and double-checked (by two analysts) script across all three databases. At last, the stratified results could not be driven by the strata definition itself but underlying differences; hence, multivariate models are required to truly identify the patients with high risk.
Conclusions
Individuals who already have sustained an initial fracture and especially those who suffer a fracture while on treatment with bisphosphonates experience higher re-fracture incidence rates than those with a newly diagnosed osteoporosis with or without treatment. Spanish individuals demonstrated an overall lower risk of major osteoporotic fractures except for those individuals who re-fractured, where the incident rate was found even higher than in the UK. Similar age-specific major osteoporotic fractures were seen for all three countries; however, the risk was much higher among the younger patients (50–60 years old).
Data availability
The lead author (SK) affirms that the manuscript is an honest, accurate and transparent account of the study being reported. No important aspects of the study have been omitted, and any discrepancies from the study as planned (and, if relevant, registered) have been explained. Regarding data sharing, there is no additional data available.
Code availability
No additional code is available.
References
Dyer SM, Crotty M, Fairhall N, Magaziner JS, Beaupre LA, Cameron I, Sherrington C (2017) A critical review of the long-term disability outcomes following hip fracture. Innov Aging 1(1):736. https://doi.org/10.1093/geroni/igx004.2656
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8(1–2):136. https://doi.org/10.1007/s11657-013-0136-1
Banefelt J, Åkesson KE, Spångéus A, Ljunggren O, Karlsson L, Ström O, Ortsäter G, Libanati C, Toth E (2019) Risk of imminent fracture following a previous fracture in a Swedish database study. Osteoporos Int 30(3):601–609. https://doi.org/10.1007/s00198-019-04852-8
Bonafede M, Shi N, Barron R, Li X, Crittenden DB, Chandler D (2016) Predicting imminent risk for fracture in patients aged 50 or older with osteoporosis using US claims data. Arch Osteoporos 11(1):26. https://doi.org/10.1007/s11657-016-0280-5
Balasubramanian A, Zhang J, Chen L, Wenkert D, Daigle SG, Grauer A, Curtis JR (2019) Risk of subsequent fracture after prior fracture among older women. Osteoporos Int 30(1):79–92. https://doi.org/10.1007/s00198-018-4732-1
Kanis JA, Johansson H, Odén A, Harvey NC, Gudnason V, Sanders KM, Sigurdsson G, Siggeirsdottir K, Fitzpatrick LA, Borgström F, McCloskey EV (2018) Characteristics of recurrent fractures. Osteoporos Int 29(8):1747–1757. https://doi.org/10.1007/s00198-018-4502-0
Johansson H, Siggeirsdóttir K, Harvey NC, Odén A, Gudnason V, McCloskey E, Sigurdsson G, Kanis JA (2017) Imminent risk of fracture after fracture. Osteoporos Int 28(3):775–780. https://doi.org/10.1007/s00198-016-3868-0
Hannan MT, Weycker D, McLean RR, Sahni S, Bornheimer R, Barron R, Travison TG, Kiel DP (2019) Predictors of imminent risk of nonvertebral fracture in older, high-risk women: the Framingham Osteoporosis Study. JBMR Plus 3(6):e10129. https://doi.org/10.1002/jbm4.10129
Bliuc D, Alarkawi D, Nguyen TV, Eisman JA, Center JR (2015) Risk of subsequent fractures and mortality in elderly women and men with fragility fractures with and without osteoporotic bone density: the Dubbo Osteoporosis Epidemiology Study. J Bone Miner Res 30(4):637–646. https://doi.org/10.1002/jbmr.2393
Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, Eisman J, Fujiwara S, Garnero P, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35(2):375–382. https://doi.org/10.1016/j.bone.2004.03.024
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19(4):385–397. https://doi.org/10.1007/s00198-007-0543-5
Hippisley-Cox J, Coupland C (2012) Derivation and validation of updated QFracture algorithm to predict risk of osteoporotic fracture in primary care in the United Kingdom: prospective open cohort study. BMJ 344:e3427. https://doi.org/10.1136/bmj.e3427
van Geel TA, van Helden S, Geusens PP, Winkens B, Dinant GJ (2009) Clinical subsequent fractures cluster in time after first fractures. Ann Rheum Dis 68(1):99–102. https://doi.org/10.1136/ard.2008.092775
Hippisley-Cox J, Coupland C, Brindle P (2014) The performance of seven QPrediction risk scores in an independent external sample of patients from general practice: a validation study. BMJ Open 4(8):e005809. https://doi.org/10.1136/bmjopen-2014-005809
García-Gil Mdel M, Hermosilla E, Prieto-Alhambra D, Fina F, Rosell M, Ramos R, Rodriguez J, Williams T, Van Staa T, Bolíbar B (2011) Construction and validation of a scoring system for the selection of high-quality data in a Spanish population primary care database (SIDIAP). Inform Prim Care 19(3):135–145. https://doi.org/10.14236/jhi.v19i3.806
Pottegård A, Schmidt SAJ, Wallach-Kildemoes H, Sørensen HT, Hallas J, Schmidt M (2017) Data resource profile: the Danish National Prescription Registry. Int J Epidemiol 46(3):798–798f. https://doi.org/10.1093/ije/dyw213
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT (2015) The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 7:449–490. https://doi.org/10.2147/CLEP.S91125
Imel EA, Eckert G, Modi A, Li Z, Martin J, de Papp A, Allen K, Johnston CC, Hui SL, Liu Z (2016) Proportion of osteoporotic women remaining at risk for fracture despite adherence to oral bisphosphonates. Bone 83:267–275. https://doi.org/10.1016/j.bone.2015.11.021
Black DM, Thompson DE, Bauer DC, Ensrud K, Musliner T, Hochberg MC, Nevitt MC, Suryawanshi S, Cummings SR, Fracture Intervention Trial (2000) Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial: FIT Research Group. J Clin Endocrinol Metab 85(11):4118–4124. https://doi.org/10.1210/jcem.85.11.6953
Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, Chesnut CH 3rd, Brown J, Eriksen EF, Hoseyni MS, Axelrod DW, Miller PD (1999) Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial: Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. JAMA 282(14):1344–1352. https://doi.org/10.1001/jama.282.14.1344
Prieto-Alhambra D, Pagès-Castellà A, Wallace G, Javaid MK, Judge A, Nogués X, Arden NK, Cooper C, Diez-Perez A (2014) Predictors of fracture while on treatment with oral bisphosphonates: a population-based cohort study. J Bone Miner Res 29(1):268–274. https://doi.org/10.1002/jbmr.2011
Abrahamsen B, Eiken P, Prieto-Alhambra D, Eastell R (2016) Risk of hip, subtrochanteric, and femoral shaft fractures among mid and long term users of alendronate: nationwide cohort and nested case-control study. BMJ 353:i3365. https://doi.org/10.1136/bmj.i3365
Dhanwal DK, Dennison EM, Harvey NC, Cooper C (2011) Epidemiology of hip fracture: worldwide geographic variation. Indian J Orthop 45(1):15–22. https://doi.org/10.4103/0019-5413.73656
Curtis EM, Moon RJ, Harvey NC, Cooper C (2017) Reprint of the impact of fragility fracture and approaches to osteoporosis risk assessment worldwide. Int J Orthop Trauma Nurs 26:7–17. https://doi.org/10.1016/j.ijotn.2017.04.004
Duarte SD, Vilaplana L, Güerri R, Nogués X, Wang-Fagerland M, Diez-Perez A, Eriksen FE (2015) Are the high hip fracture rates among Norwegian women explained by impaired bone material properties? J Bone Miner Res 30(10):1784–1789. https://doi.org/10.1002/jbmr.2537
Fajar JK, Taufan T, Syarif M, Azharuddin A (2018) Hip geometry and femoral neck fractures: a meta-analysis. J Orthop Translat 13:1–6. https://doi.org/10.1016/j.jot.2017.12.002
Brozek W, Reichardt B, Zwerina J, Dimai HP, Klaushofer K, Zwettler E (2016) Antiresorptive therapy and risk of mortality and refracture in osteoporosis-related hip fracture: a nationwide study. Osteoporos Int 27(1):387–396. https://doi.org/10.1007/s00198-015-3415-4
Ahmed LA, Center JR, Bjørnerem A, Bluic D, Joakimsen RM, Jørgensen L, Meyer HE, Nguyen ND, Nguyen TV, Omsland TK, Størmer J, Tell GS, van Geel TA, Eisman JA, Emaus N (2013) Progressively increasing fracture risk with advancing age after initial incident fragility fracture: the Tromsø study. J Bone Miner Res 28(10):2214–2221. https://doi.org/10.1002/jbmr.1952
Drake MT, Clarke BL, Khosla S (2008) Bisphosphonates: mechanism of action and role in clinical practice. Mayo Clin Proc 83(9):1032–1045. https://doi.org/10.4065/83.9.1032
Acknowledgements
The authors would like to acknowledge Paloma Doherty for project management; CPRD, SIDIAP and DHR for their support; and UCB Pharma for funding this study.
Funding
This study received funding from UCB Pharma.
Author information
Authors and Affiliations
Contributions
Study design: DPA, BA and ET. Data analysis: SK, DPA and ME. Data interpretation: SK, DPA, BA, ET, CL, CC and CR. Drafting manuscript: SK, DPA and CR. Revising manuscript content: all co-authors. Approving final version of manuscript: all authors. DPA takes responsibility for the integrity of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
BA reports grants from UCB, during the conduct of the study, personal fees from UCB, grants from Novartis, personal fees from Amgen, personal fees from Eli-Lilly and personal fees from Pharmacosmos, outside the submitted work. ME reports institutional grants from UCB, during the conduct of the study. CL reports being an employee and stockholder of UCB Pharma. DPA reports grants and others from AMGEN; grants, non-financial support and others from UCB Biopharma; and grants from Les Laboratoires Servier, outside the submitted work; Janssen, on behalf of IMI-funded EHDEN and EMIF consortiums, and Synapse Management Partners have supported training programmes organized by DPA’s department and open for external participants. ET is an employee of UCB Pharma, who sponsored the study. AD, SK and CR have no conflicts to declare.
Consent to participate
Consent to participate was not required as only anonymised retrospective data was used for this study, and no patient or GP contact was required.
Consent for publication
All authors have given their consent for the publication.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees of each country (Spain, UK and Denmark) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. More specifically, for the UK, the study was approved by the Independent Scientific Advisory Committee (ISAC 17_128R); for Spain, the study was approved by the IDIAP J Gol Clinical Research Ethics Committee (P17_152); and for Denmark, the study was approved by Statistics Denmark (Reference 706638).
Informed consent
Informed consent was not required as only anonymised retrospective data was used for this study, and no patient or GP contact was required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Khalid, S., Reyes, C., Ernst, M. et al. One- and 2-year incidence of osteoporotic fracture: a multi-cohort observational study using routinely collected real-world data. Osteoporos Int 33, 123–137 (2022). https://doi.org/10.1007/s00198-021-06077-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-06077-0