Abstract
Summary
Our aim was to explore change in kyphosis and vertebral fracture incidence following 8 months of high-intensity resistance and impact training (HiRIT) or machine-based isometric axial compression (IAC) training in men with osteopenia and osteoporosis. HiRIT and IAC improved posture. HiRIT participants did not experience progression or incident vertebral fracture. IAC participants did experience progression and incident vertebral fracture.
Introduction
The Lifting Intervention For Training Muscle and Osteoporosis Rehabilitation for Men (LIFTMOR-M) trial examined efficacy and safety of an eight-month, supervised, high-intensity progressive resistance and impact training (HiRIT) program compared with machine-based isometric axial compression (IAC) training in middle-aged and older men with low areal bone mineral density (aBMD). The primary purpose of the current work was to explore change in thoracic kyphosis and incident fracture from vertebral morphology following eight-months of HiRIT or IAC training. The secondary purpose was to explore change in clinical kyphosis measures for HiRIT, IAC and a non-randomized, matched control group.
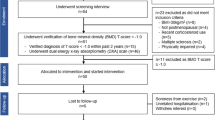
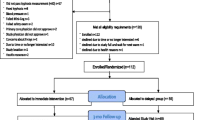
Methods
Men (≥ 45 yrs), with low aBMD, were recruited and randomized to HiRIT or IAC, or designated control. Clinical measures of thoracic kyphosis with inclinometry were determined. Cobb angle of kyphosis and vertebral fracture assessment using the Genant semi-quantitative method were determined from lateral thoracolumbar DXA (Medix DR, Medilink, France). Per-protocol (n = 40) and intention-to-treat (n = 93) analyses were conducted.
Results
Forty participants (HiRIT n = 20, IAC n = 20; 66.1 ± 7.8 yrs.; lumbar spine T-score − 0.1 ± 0.8; femoral neck T-score − 1.5 ± 0.5) underwent clinical kyphosis measures and thoracolumbar DXA at baseline and follow-up. No between-group differences were detected in kyphosis change, however, within-group improvements in neutral (HiRIT − 2.3 ± 0.8°; IAC − 2.5 ± 0.8°) and ‘standing tall’ (HiRIT − 2.4 ± 0.8°; IAC − 2.0 ± 0.8°) postures were observed (p < 0.05). HiRIT improved Cobb angle (− 3.5 ± 1.5°, p = 0.027) from baseline. Over the 8 months, no incident vertebral fractures nor progression of prevalent vertebral fractures occurred for HiRIT participants. Five incident fractures of thoracic vertebrae occurred for IAC and one wedge fracture progressed. Ninety-three participants underwent clinical kyphosis measures at both time-points (HiRIT n = 34, IAC n = 33, control n = 26). HiRIT exhibited a reduction in ‘standing tall’ kyphosis compared to control (− 2.3 ± 0.6° versus 1.4 ± 0.7°, p < 0.05), but no other between-group differences were detected.
Conclusions
Although there was no difference in change between intervention groups, thoracic kyphosis appeared to improve in both HiRIT and IAC with exercise exposure. HiRIT improved 'standing tall' posture in comparison to usual activities. HiRIT was not associated with vertebral fracture progression or incident vertebral fracture, but for some IAC participants there was evidence of progression of vertebral fracture severity and incident vertebral fractures, in our small sample. Larger trials are required to confirm the observations of the current work, which was exploratory in nature.


Similar content being viewed by others
References
Bouillon R, Burckhardt P, Christiansen C, Fleisch HA, Fujita T, Gennari C, Marin TJ, Mazzuoli G, Melton LJ, Ringe JD (1991) Consensus development conference: prophylaxis and treatment of osteoporosis. Am J Med 90:107–110
Cummings SR, Melton LJ III (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359(9319):1761–1767. https://doi.org/10.1016/S0140-6736(02)08657-9
Johnell O, Kanis JA, Oden A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jonsson B (2004) Mortality after osteoporotic fractures. Osteoporos Int 15(1):38–42. https://doi.org/10.1007/s00198-003-1490-4
Wasnich RD (1996) Vertebral fracture epidemiology. Bone 18(3):179S–183S. https://doi.org/10.1016/8756-3282(95)00499-8
Cooper C, Atkinson EJ, O'Fallon WM, Melton LJ III (1992) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res 7(2):221–227
Horii C, Asai Y, Iidaka T, Muraki S, Oka H, Tsutsui S, Hashizume H, Yamada H, Yoshida M, Kawaguchi H, Nakamura K, Akune T, Tanaka S, Yoshimura N (2019) Differences in prevalence and associated factors between mild and severe vertebral fractures in Japanese men and women: the third survey of the ROAD study. J Bone Miner Res 37(5):844–853. https://doi.org/10.1007/s00774-018-0981-5
Jackson SA, Tenenhouse S, Robertson L (2000) Vertebral fracture definition from population-based data: preliminary results from the Canadian Multicenter Osteoporosis Study (CaMos). Osteoporos Int 11(8):680–687. https://doi.org/10.1007/s001980070066
O'Neill TW, Felsenberg D, Varlow J, Cooper C, Kanis JA, Silman AJ, Group aTEVOS (1996) The prevalence of vertebral defomity in European men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res 11 (7): https://doi.org/10.1002/jbmr.5650110719
Magnus KK, Kherad M, Hasserius R, Nilsson J, Redlund-Johnell I, Ohlsson C, Lorentzon M, Mellstrom D, Rosengren BE (2016) Characteristics of prevalent vertebral fractures predict new fractures in elderly men. J Bone Joint Surg Am 98(5):379–385. https://doi.org/10.2106/JBJS.15.00328
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353(9156):878–882. https://doi.org/10.1016/S0140-6736(98)09075-8
Scane AC, Sutcliffe AM, Francis RM (1994) The sequelae of vertebral cruch fractures in men. Osteoporos Int 4(2):89–92. https://doi.org/10.1007/BF01623230
Kado DM, Huang M, Karlamangla AS, Cawthon P, Katzman WB, Hillier TA, Ensrud K, Cummings SR (2012) Factors associated with kyphosis progression in older women: 15 years’ experience in the study of osteoporotic fractures. J Bone Miner Res 28(1):179–187. https://doi.org/10.1002/jbmr.1728
Giangregorio LM, Papaioannou A, MacIntyre NJ, Ashe MC, Heinonen A, Shipp K, Wark JD, McGill S, Keller H, Jain R, Laprade J, Cheung AM (2014) Too fit to fracture: exercise recommendations for individuals with osteoporosis or osteoporotic vertebral fracture. Osteoporos Int 25(3):821–835. https://doi.org/10.1007/s00198-013-2523-2
Beck BR, Daly RM, Singh MA, Taaffe DR (2017) Exercise and Sports Science Australia (ESSA) position statement on exercise prescription for the prevention and management of osteoporosis. J Sci Med Sport 20(5):438–445. https://doi.org/10.1016/j.jsams.2016.10.001
Kukuljan S, Nowson CA, Bass SL, Sanders K, Nicholson GC, Seibel MJ, Salmon J, Daly RM (2009) Effects of a multi-component exercise program and calcium-vitamin-D3-fortified milk on bone mineral density in older men: a randomised controlled trial. Osteoporos Int 20(7):1241–1251. https://doi.org/10.1007/s00198-008-0776-y
Kukuljan S, Nowson CA, Sanders KM, Nicholson GC, Seibel MJ, Salmon J, Daly RM (2011) Independent and combined effects of calcium-vitamin D3 and exercise on bone structure and strength in older men: an 18-month factorial design randomized controlled trial. J Clin Endocrinol Metab 96(4):955–963. https://doi.org/10.1210/jc.2010-2284
Gianoudis J, Bailey CA, Ebeling PR, Nowson CA, Sanders KM, Hill K, Daly RM (2014) Effects of a targeted multimodal exercise program incorporating high-speed power training on falls and fracture risk factors in older adults: a community-based randomized controlled trial. J Bone Miner Res 29(1):182–191. https://doi.org/10.1002/jbmr.2014
Daly RM, Gianoudis J, Kersh ME, Bailey CA, Ebeling PR, Krug R, Nowson CA, Hill K, Sanders KM (2019) Effects of a 12-month supervised, community-based multimodal exercise program followed by a 6-month reseach-to-practice transition on bone mineral density, trabecular microarchitecture, and physical function in older adults: a randomized controlled trial. J Bone Miner Res 35 (3): 419-429. https://doi.org/10.1002/jbmr.3865
Watson SL, Weeks BK, Weis LJ, Harding AT, Horan SA, Beck BR (2019) High-intensity exercise did not cause vertebral fractures and improves thoracic kyphosis in postmenopausal women with low to very low bone mass: the LIFTMOR trial. Osteoporos Int 30(5):957–964. https://doi.org/10.1007/s00198-018-04829-z
Harding AT, Weeks BK, Lambert C, Watson SL, Weis LJ, Beck BR (2020) A comparison of bone-targeted exercise strategies to reduce fracture risk in middle-aged and older men with osteopenia and osteoporosis: LIFTMOR-M semi-randomized controlled trial. J Bone Miner Res. https://doi.org/10.1002/jbmr.4008
Harding AT, Weeks BK, Lambert C, Watson SL, Weis LJ, Beck BR (2020) Effects of supervised high-intensity resistance and impact training or machine-based isometric training on regional bone geometry and strength in middle-aged and older men with low bone mass: the LIFTMOR-M semi-randomised controlled trial. Bone 136:115362. https://doi.org/10.1016/j.bone.2020.115362
Harding AT, Weeks BK, Watson SL, Beck BR (2017) The LIFTMOR-M (Lifting Intervention For Training Muscle and Osteoporosis Rehabilitation for Men) trial: protocol for a semirandomised controlled trial of supervised targeted exercise to reduce risk of osteoporotic fracture in older men with low bone mass. BMJ Open 7(6):e014951. https://doi.org/10.1136/bmjopen-2016-014951
Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP (2011) 'American College of Sports Medicine' position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc 43(7):1334–1359. https://doi.org/10.1249/MSS.0b013e318213fefb
Weeks BK, Beck BR (2008) The BPAQ: a bone-specific physical activity assessment instrument. Osteoporos Int 19(11):1567–1577. https://doi.org/10.1007/s00198-008-0606-2
Beck BR, Weeks BK, Norling TL (2011) A novel Australian calcium-specific diet questionnaire: validity and reliability. Osteoporos Int 22:S626–S627
MacIntyre NJ, Lorbergs AL, Adachi JD (2014) Inclinometer-based measures of standing posture in older adults with low bone mass are reliable and associated with self-reported, but not performance-based, physical function. Osteoporos Int 25(2):721–728. https://doi.org/10.1007/s00198-013-2484-5
Katzman WB, Vittinghoff E, Lin F, Schafer A, Long RK, Wong S, Gladin A, Fan B, Allaire B, Kado DM, Lane NE (2017) Targeted spine strengthening exercise and posture training program to reduce hyperkyphosis in older adults: results from the study of Hyperkyphosis, exercise, and function (SHEAF) randomized controlled trial. Osteoporos Int 28(10):2831–2841. https://doi.org/10.1007/s00198-017-4109-x
Kado DM, Prenovost K, Crandall C (2007) Narrative review: hyperkyphosis in older persons. Ann Intern Med 147(5):330–338. https://doi.org/10.7326/0003-4819-147-5-200709040-00008
Kado DM, Christianson L, Palermo L, Smith-Bindman R, Cummings SR, Greendale GA (2006) Comparing a supine radiologic versus standing clinical measurement of kyphosis in older women: the Fracture Intervention Trial. Spine 31(4):463–467. https://doi.org/10.1097/01.brs.0000200131.01313.a9
Briggs AM, Wrigley TV, Tully EA, Adams PE, Greig AM, Bennell KL (2007) Radiographic measures of thoracic kyphosis in osteoporosis: Cobb and vertebral centroid angles. Skelet Radiol 36(8):761–767. https://doi.org/10.1007/s00256-007-0284-8
Schousboe JT, Shepherd JA, Bilezikian JP, Baim S (2013) Executive summary of the 2013 International Society for Clinical Densitometry Position Development Conference on Bone Densitometry. J Clin Densitom 16(4):455–466. https://doi.org/10.1016/j.jocd.2013.08.004
Genant HK, Chun YW, Van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8(9):1137–1148. https://doi.org/10.1002/jbmr.5650080915
Bansal S, Katzman WB, Giangregorio LM (2014) Exercise for improving age-related hyperkyphotic posture: a systematic review. Arch Phys Med Rehabil 95(1):129–140. https://doi.org/10.1016/j.apmr.2013.06.022
Katzman WB, Parimi N, Gladin A, Poltavskiy EA, Schafer AL, Long RK, Fan B, Wong SS, Lane NE (2017) Sex differences in response to targeted kyphosis specific exercise and posture training in community-dwelling older adults: a randomized controlled trial. BMC Musculoskelet Disord 18(1):509. https://doi.org/10.1186/s12891-017-1862-0
Katzman WB, Miller-Martinez D, Marshall LM, Lane NE, Kado DM (2014) Kyphosis and paraspinal muscle composition in older men: a cross-sectional study for the osteoporotic fractures in men (MrOS) research group. BMC Musculoskelet Disord 15(1):19. https://doi.org/10.1186/1471-2474-15-19
Kado DM, Miller-Martinez D, Lui LY, Cawthon P, Katzman WB, Hillier TA, Fink HA, Ensrud KE (2014) Hyperkyphosis, kyphosis progression, and risk of non-spine fractures in older community dwelling women: the Study of Osteoporotic Fractures (SOF). J Bone Miner Res 29(10):2210–2216. https://doi.org/10.1002/jbmr.2251
Mika A, Unnithan VB, Mika P (2005) Differences in thoracic kyphosis and in back muscle strength in women with bone loss due to osteoporosis. Spine 30(2):241–246. https://doi.org/10.1097/01.brs.0000150521.10071.df
Katzman WB, Parimi N, Mansoori Z, Nardo L, Kado DM, Cawthon PM, Marshall LM, Schousboe JT, Lane NE, Osteoporotic Fractures in Men Study Research G, the Study of Osteoporotic F (2016) Cross-sectional and longitudinal associations of diffuse idiopathic skeletal hyperostosis (DISH) and thoracic kyphosis in older men and women. Arthritis Care Res 69(8):1245–1252. https://doi.org/10.1002/acr.23115
Katzman WB, Harrison SL, Fink HA, Marshall LM, Orwoll E, Barrett-Connor E, Cawthon PM, Kado DM, Osteoporotic Fractures in Men (MrOS) Study Research Group (2015) Physical function in older men with hyperkyphosis. J Gerontol A Biol Sci Med Sci 70(5):635–640. https://doi.org/10.1093/gerona/glu213
Kado DM, Huang MH, Barrett-Connor E, Greendale GA (2005) Hyperkyphotic posture and poor physical functional ability in older community-dwelling men and women: the Rancho Bernardo study. J Gerontol A Biol Sci Med Sci 60(5):633–637. https://doi.org/10.1093/gerona/60.5.633
Webber C, Papaioannou A, Winegard K, Adachi JD, Parkinson W, Ferko N, Cook RJ, McCartney N (2003) A 6-mo home-based exercise program may slow vertebral height loss. J Clin Densitom 6(4):391–400. https://doi.org/10.1385/JCD:6:4:391
Giangregorio LM, Gibbs JC, Templeton JA, Adachi JD, Ashe MC, Bleakney RR, Cheung AM, Hill KD, Kendler DL, Khan AA, Kim S, McArthur C, Mittmann N, Papaioannou A, Prasad S, Scherer SC, Thabane L, Wark JD (2018) Build better bones with exercise (B3E pilot trial): results of a feasibility study of a multicenter randomized controlled trial of 12 months of home exercise in older women with vertebral fracture. Osteoporos Int 29(11):2545–2556. https://doi.org/10.1007/s00198-018-4652-0
Briggs AM, Wrigley TV, Van Dieen JH, Phillips BE, Kai Lo S, Greig AM, Bennell KL (2006) The effect of osteoporotic vertebral fracture on predicted spinal loads in vivo. Eur Spine J 15(12):1785–1795. https://doi.org/10.1007/s00586-006-0158-0
Giangregorio LM, McGill S, Wark JD, Laprade J, Heinonen A, Ashe MC, MacIntyre NJ, Cheung AM, Shipp K, Keller H, Jain R, Papaioannou A (2015) Too fit to fracture: outcomes of a Delphi consensus process on physical activity and exercise recommendations for adults with osteoporosis with or without vertebral fractures. Osteoporos Int 26(3):891–910. https://doi.org/10.1007/s00198-014-2881-4
Gibbs JC, MacIntyre NJ, Ponzano M, Templeton JA, Thabane L, Papaioannou A, Giangregorio LM (2019) Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst Rev 7:CD008618. https://doi.org/10.1002/14651858.CD008618.pub3
Lewiecki EM, Laster AJ (2006) Clinical review: clinical applications of vertebral fracture assessment by dual-energy x-ray absorptiometry. J Clin Endocrinol Metab 91(11):4215–4222. https://doi.org/10.1210/jc.2006-1178
Ferrar L, Eastell R (1999) Identification of vertebral deformities in men: comparison of morphometric radiographic and morphometric x-ray absorptiometry. Osteoporos Int 10(2):167–174. https://doi.org/10.1007/s001980050212
Binkley N, Krueger D, Gangnon R, Genant HK, Drezner MK (2005) Lateral vertebral assessment: a valuable technique to detect clinically significant vertebral fractures. Osteoporos Int 16(12):1513–1518. https://doi.org/10.1007/s00198-005-1891-7
Domiciano DS, Figueiredo CP, Lopes JB, Kuroishi ME, Takayama L, Caparbo VF, Fuller P, Menezes PF, Scazufca M, Bonfa E, Pereira RM (2012) Vertebral fracture assessment by dual X-ray absorptiometry: a valid tool to detect vertebral fractures in community-dwelling older adults in a population-based survey. Arthritis Care Res (Hoboken) 65(5):809–815. https://doi.org/10.1002/acr.21905
Acknowledgements
The authors wish to thank the participants who took part in the study for their valuable contribution, Sports Medicine Australia for its support for exercise equipment, and Osteoporosis Australia for the bioDensity™ equipment grant.
Registration
Australian New Zealand Clinical Trials Registry (#12616000344493).
Protocol
Harding AT, Weeks BK, Watson SL, Beck BR. The LIFTMOR–M (Lifting Intervention For Training Muscle and Osteoporosis Rehabilitation for Men) trial: Protocol for a semi-randomized controlled trial of supervised targeted exercise to reduce risk of osteoporotic fracture in older men with low bone mass. BMJ Open (Rehabilitation Medicine), 2017, 7 (e014951).
Funding
Performance Health Systems (Northbrook, IL, USA) supplied and installed the bioDensity™ isometric exercise machine through an equipment grant brokered by Osteoporosis Australia. The authors wish to acknowledge the support of the 2016 Sports Medicine Australian Research Foundation Grant for the purchase of HiRIT training equipment, and the Australian Government Research Training Program Scholarship support of Amy T Harding and Conor Lambert. The above funding sources had no role in the study design, analysis or interpretation of data, or in writing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Belinda R. Beck is a Director of The Bone Clinic, Brisbane, QLD, Australia. Amy T. Harding, Conor Lambert, Steven L. Watson and Benjamin K. Weeks declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Harding, A.T., Weeks, B.K., Lambert, C. et al. Exploring thoracic kyphosis and incident fracture from vertebral morphology with high-intensity exercise in middle-aged and older men with osteopenia and osteoporosis: a secondary analysis of the LIFTMOR-M trial. Osteoporos Int 32, 451–465 (2021). https://doi.org/10.1007/s00198-020-05583-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05583-x