Abstract
Summary
Change in total hip bone mineral density (BMD) provides a robust indication of anti-fracture effect during treatment monitoring in routine clinical practice, whereas spine BMD change is not independently associated with fracture risk.
Purpose
The role of monitoring bone mineral density (BMD) as an indicator of an anti-fracture effect is controversial. Discordance between the spine and hip BMD is common and creates uncertainty in clinical practice.
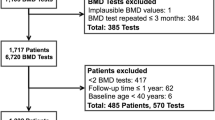
Methods
Using a population-based BMD Registry for the Province of Manitoba, Canada, we compared change in the spine and hip BMD as an indicator of treatment-related fracture risk reduction. The study cohort included 6093 women age > 40 years initiating osteoporosis treatment with two consecutive dual-energy X-ray absorptiometry (DXA) scans (mean interval 4.7 years). We computed change in the spine, total hip, and femur neck BMD between the first and second DXA scans as categorical (categorized as stable, detectable decrease, or detectable increase) and continuous measures. We modeled time to first incident fracture, ascertained from health services data, using Cox regression adjusted for baseline fracture probability.
Results
During a mean follow-up of 12.1 years, 995 women developed incident major osteoporotic fractures (MOF) including 246 with hip fractures and 301 with clinical vertebral fractures. Women with a detectable decrease in total hip BMD compared with stable BMD experienced an increase in MOF (adjusted hazard ratio [aHR] 1.46, 95% confidence interval [CI] 1.25–1.70) while those with a detectable increase in total hip BMD experienced a decrease in MOF (aHR 0.71, 95% CI 0.61–0.83), and these results were not attenuated when adjusted for change in spine BMD. Similar results were seen for hip and clinical vertebral fracture outcomes, when BMD change was assessed as a continuous measure, and when femur neck BMD monitoring was used instead of total hip BMD monitoring.
Conclusions
Treatment-related increases in total hip BMD are associated with lower MOF, hip, and clinical vertebral fracture risk compared with stable BMD, while BMD decreases are associated with higher fracture risk. In contrast, spine BMD change is not independently associated with fracture risk.

Similar content being viewed by others
References
Compston JE, McClung MR, Leslie WD (2019) Osteoporosis. Lancet 393(10169):364–376
Cummings SR, Bates D, Black DM (2002) Clinical use of bone densitometry: scientific review. JAMA. 288(15):1889–1897
Force USPST (2011) Screening for osteoporosis: U.S. preventive services task force recommendation statement. Ann Intern Med 154(5):356–364
Compston J, Cooper A, Cooper C, Gittoes N, Gregson C, Harvey N et al (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12(1):43
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R, National Osteoporosis Foundation (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381
Kanis JA, Harvey NC, Cooper C, Johansson H, Oden A, McCloskey EV et al (2016) A systematic review of intervention thresholds based on FRAX: a report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos 11(1):25
MacLean C, Newberry S, Maglione M, McMahon M, Ranganath V, Suttorp M, Mojica W, Timmer M, Alexander A, McNamara M, Desai SB, Zhou A, Chen S, Carter J, Tringale C, Valentine D, Johnsen B, Grossman J (2008) Systematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Ann Intern Med 148(3):197–213
Murad MH, Drake MT, Mullan RJ, Mauck KF, Stuart LM, Lane MA, Abu Elnour NO, Erwin PJ, Hazem A, Puhan MA, Li T, Montori VM (2012) Clinical review. Comparative effectiveness of drug treatments to prevent fragility fractures: a systematic review and network meta-analysis. J Clin Endocrinol Metab 97(6):1871–1880
Saito T, Sterbenz JM, Malay S, Zhong L, MacEachern MP, Chung KC (2017) Effectiveness of anti-osteoporotic drugs to prevent secondary fragility fractures: systematic review and meta-analysis. Osteoporos Int 28(12):3289–3300
Papaioannou A, Morin S, Cheung AM, Atkinson S, Brown JP, Feldman S, Hanley DA, Hodsman A, Jamal SA, Kaiser SM, Kvern B, Siminoski K, Leslie WD, for the Scientific Advisory Council of Osteoporosis Canada (2010) 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ. 182(17):1864–1873
Compston J (2009) Monitoring osteoporosis treatment. Best Pract Res Clin Rheumatol 23(6):781–788
Bruyere O, Reginster JY (2014) Monitoring of osteoporosis therapy. Best Pract Res Clin Endocrinol Metab 28(6):835–841
Bell KJ, Hayen A, Macaskill P, Irwig L, Craig JC, Ensrud K et al (2009) Value of routine monitoring of bone mineral density after starting bisphosphonate treatment: secondary analysis of trial data. BMJ. 338:b2266
Hochberg MC, Greenspan S, Wasnich RD, Miller P, Thompson DE, Ross PD (2002) Changes in bone density and turnover explain the reductions in incidence of nonvertebral fractures that occur during treatment with antiresorptive agents. J Clin Endocrinol Metab 87(4):1586–1592
Wasnich RD, Miller PD (2000) Antifracture efficacy of antiresorptive agents are related to changes in bone density. J Clin Endocrinol Metab 85(1):231–236
Bouxsein ML, Eastell R, Lui LY, Wu LA, de Papp AE, Grauer A, Marin F, Cauley JA, Bauer DC, Black DM, for the FNIH Bone Quality Project (2019) Change in bone density and reduction in fracture risk: a meta-regression of published trials. J Bone Miner Res. https://doi.org/10.1002/jbmr.3641
Leslie WD, Majumdar SR, Morin SN, Lix LM (2016) Change in bone mineral density is an indicator of treatment-related antifracture effect in routine clinical practice: a registry-based cohort study. Ann Intern Med 165(7):465–472
Shepherd JA, Lu Y, Wilson K, Fuerst T, Genant H, Hangartner TN, Wilson C, Hans D, Leib ES (2006) Cross-calibration and minimum precision standards for dual-energy X-ray absorptiometry: the 2005 ISCD Official Positions. J Clin Densitom 9(1):31–36
Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA (2011) Spine-hip discordance and fracture risk assessment: a physician-friendly FRAX enhancement. Osteoporos Int 22(3):839–847
Johansson H, Kanis JA, Oden A, Leslie WD, Fujiwara S, Gluer CC et al (2014) Impact of femoral neck and lumbar spine BMD discordances on FRAX probabilities in women: a meta-analysis of international cohorts. Calcif Tissue Int 95(5):428–435
Abrahamsen B, Stilgren LS, Hermann AP, Tofteng CL, Barenholdt O, Vestergaard P et al (2001) Discordance between changes in bone mineral density measured at different skeletal sites in perimenopausal women--implications for assessment of bone loss and response to therapy: the Danish osteoporosis prevention study. J Bone Miner Res 16(7):1212–1219
Kozyrskyj AL, Mustard CA (1998) Validation of an electronic, population-based prescription database. Ann Pharmacother 32(11):1152–1157
Leslie WD, Metge C (2003) Establishing a regional bone density program: lessons from the Manitoba experience. J Clin Densitom 6(3):275–282
Leslie WD, Caetano PA, Macwilliam LR, Finlayson GS (2005) Construction and validation of a population-based bone densitometry database. J Clin Densitom 8(1):25–30
Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston Jr CC, Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8(5):468–489
Gluer CC, Blake G, Lu Y, Blunt BA, Jergas M, Genant HK (1995) Accurate assessment of precision errors: how to measure the reproducibility of bone densitometry techniques. Osteoporos Int 5(4):262–270
Gluer CC (1999) Monitoring skeletal changes by radiological techniques. J Bone Miner Res 14(11):1952–1962
Leslie WD (2008) Factors affecting short-term bone density precision assessment and the effect on patient monitoring. J Bone Miner Res 23(2):199–204
Kanis JA, Oden A, Johansson H, Borgstrom F, Strom O, McCloskey E (2009) FRAX and its applications to clinical practice. Bone. 44(5):734–743
Leslie WD, Lix LM, Langsetmo L, Berger C, Goltzman D, Hanley DA, Adachi JD, Johansson H, Oden A, McCloskey E, Kanis JA (2011) Construction of a FRAX(R) model for the assessment of fracture probability in Canada and implications for treatment. Osteoporos Int 22(3):817–827
Bisson EJ, Finlayson ML, Ekuma O, Marrie RA, Leslie WD (2019) Accuracy of FRAX(R) in people with multiple sclerosis. J Bone Miner Res. https://doi.org/10.1002/jbmr.3682
Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA et al (2010) Independent clinical validation of a Canadian FRAX tool: fracture prediction and model calibration. J Bone Miner Res 25(11):2350–2358
Fraser LA, Langsetmo L, Berger C, Ioannidis G, Goltzman D, Adachi JD et al (2011) Fracture prediction and calibration of a Canadian FRAX(R) tool: a population-based report from CaMos. Osteoporos Int 22(3):829–837
Lix LM, Azimaee M, Osman BA, Caetano P, Morin S, Metge C, Goltzman D, Kreiger N, Prior J, Leslie WD (2012) Osteoporosis-related fracture case definitions for population-based administrative data. BMC Public Health 12:301
Epp R, Alhrbi M, Ward L, Leslie WD (2018) Radiological validation of fracture definitions from administrative data. J Bone Miner Res 33(Supp 1):S275
Tsang JF, Leslie WD (2007) Exclusion of focal vertebral artifacts from spine bone densitometry and fracture prediction: a comparison of expert physicians, three computer algorithms, and the minimum vertebra. J Bone Miner Res 22(6):789–798
Jones G, Nguyen T, Sambrook PN, Kelly PJ, Eisman JA (1995) A longitudinal study of the effect of spinal degenerative disease on bone density in the elderly. J Rheumatol 22(5):932–936
Gourlay ML, Fine JP, Preisser JS, May RC, Li C, Lui LY, Ransohoff DF, Cauley JA, Ensrud KE (2012) Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med 366(3):225–233
Acknowledgments
The authors acknowledge the Manitoba Centre for Health Policy (MCHP) for use of data contained in the Population Health Research Data Repository (HIPC Project Number 2016/2017-29). The results and conclusions are those of the authors, and no official endorsement by the MCHP, Manitoba Health, or other data providers is intended or should be inferred. This article has been reviewed and approved by the members of the Manitoba Bone Density Program Committee.
Grant support
Dr. Lix is supported by a Tier 1 Canada Research Chair.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Health Research Ethics Board for the University of Manitoba.
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOC 209 kb)
Rights and permissions
About this article
Cite this article
Leslie, W.D., Martineau, P., Bryanton, M. et al. Which is the preferred site for bone mineral density monitoring as an indicator of treatment-related anti-fracture effect in routine clinical practice? A registry-based cohort study. Osteoporos Int 30, 1445–1453 (2019). https://doi.org/10.1007/s00198-019-04975-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-04975-y