Abstract
Summary
Whether in-hospital management of patients with newly identified vertebral fractures leads to a higher rate of osteoporosis medication than delayed outpatient management remains unknown. Our study showed that early osteoporosis therapy initiation in a fracture liaison service during hospital stay was a more efficacious strategy for secondary fracture prevention.
Introduction
Fracture liaison services are standard care for secondary fracture prevention. A higher rate of osteoporosis treatment initiation may be considered when introduced in the hospital rather than an outpatient recommendation to a primary care physician (PCP). Whether this applies to patients with newly detected vertebral fractures in a general internal medicine ward remains unknown. We prospectively investigated whether in-hospital management of newly identified vertebral fractures led to a higher rate of osteoporosis medication initiation and persistence at 3 and 6 months than delayed outpatient management by a PCP.
Methods
We conducted a prospective study including hospitalized patients > 60 years systematically searched for asymptomatic vertebral fractures on lateral chest and/or abdominal radiographs. Patients were included either in phase 1 (outpatient care recommendations on osteoporosis management to a PCP) or in phase 2 (inpatient care management initiated during hospitalization). The percentage of patients under osteoporosis treatment was evaluated by telephone interview at 3 and 6 months.
Results
Outpatients’ (84 with fracture/407 assessed (21%); 75.7 ± 7.7 years) and inpatients’ (100/524 (19%); 77.8 ± 9.4 years) characteristics were similar. Osteoporosis medication was more often prescribed in inpatients at 3 (67% vs. 19%, respectively; p < 0.001) and 6 months (69 vs. 27%, respectively; p < 0.001). The percentage under treatment was also higher in inpatients than in outpatients at 3 (52 vs. 19%, p < 0.001) and 6 months (54 vs. 22%, p < 0.001). Length of stay and destination post-discharge were not different between groups.
Conclusions
Early patient management after a newly detected vertebral fracture during hospitalization was a more efficacious strategy of secondary fracture prevention than delayed outpatient management following discharge.


Similar content being viewed by others
References
Ballane G, Cauley JA, Luckey MM, El-Hajj Fuleihan G (2017) Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int 28:1531–1542
Fink HA, Milavetz DL, Palermo L, Nevitt MC, Cauley JA, Genant HK, Black DM, Ensrud KE, Fracture Intervention Trial Research G (2005) What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J Bone Miner Res 20:1216–1222
Casez P, Uebelhart B, Gaspoz JM, Ferrari S, Louis-Simonet M, Rizzoli R (2006) Targeted education improves the very low recognition of vertebral fractures and osteoporosis management by general internists. Osteoporos Int 17:965–970
Ensrud KE, Blackwell TL, Fink HA, Zhang J, Cauley JA, Cawthon PM, Black DM, Bauer DC, Curtis JR, Orwoll ES, Barrett-Connor E, Kado DM, Marshall LM, Shikany JM, Schousboe JT, for the Osteoporotic Fractures in Men (MrOS) Research Group (2016) What proportion of incident radiographic vertebral fractures in older men is clinically diagnosed and vice versa: a prospective study. J Bone Miner Res 31:1500–1503
Johansson L, Sundh D, Nilsson M, Mellstrom D, Lorentzon M (2018) Vertebral fractures and their association with health-related quality of life, back pain and physical function in older women. Osteoporos Int 29:89–99
Pizzato S, Trevisan C, Lucato P, Girotti G, Mazzochin M, Zanforlini BM, Bano G, Piovesan F, Bertocco A, Zoccarato F, Dianin M, Manzato E, Sergi G (2018) Identification of asymptomatic frailty vertebral fractures in post-menopausal women. Bone 113:89–94
Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB, Licata A, Benhamou L, Geusens P, Flowers K, Stracke H, Seeman E (2001) Risk of new vertebral fracture in the year following a fracture. Jama 285:320–323
Kanis JA, Johnell O, De Laet C et al (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375–382
Johansson H, Siggeirsdottir K, Harvey NC, Oden A, Gudnason V, McCloskey E, Sigurdsson G, Kanis JA (2017) Imminent risk of fracture after fracture. Osteoporos Int 28:775–780
Frederiksen A, Abrahamsen B, Johansen PB, Sorensen HA (2018) Danish, national cross-sectional observational study on the prevalence of prior major osteoporotic fractures in adults presenting with hip fracture-limitations and scope for fracture liaison services in prevention of hip fracture. Osteoporos Int 29:109–114
Rizzoli R (2011) Bisphosphonates for post-menopausal osteoporosis: are they all the same? QJM 104:281–300
Lyles KW, Colon-Emeric CS, Magaziner JS et al (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 357:1799–1809
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C, FREEDOM Trial (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361:756–765
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, Wang O, Mellström D, Oefjord ES, Marcinowska-Suchowierska E, Salmi J, Mulder H, Halse J, Sawicki AZ, Mitlak BH (2001) Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344:1434–1441
Khosla S, Shane E (2016) A crisis in the treatment of osteoporosis. J Bone Miner Res 31:1485–1487
Yusuf AA, Matlon TJ, Grauer A, Barron R, Chandler D, Peng Y (2016) Utilization of osteoporosis medication after a fragility fracture among elderly Medicare beneficiaries. Arch Osteoporos 11:31
Chevalley T, Hoffmeyer P, Bonjour JP, Rizzoli R (2002) An osteoporosis clinical pathway for the medical management of patients with low-trauma fracture. Osteoporos Int 13:450–455
Akesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, Kyer C, Cooper C, Group IOFFW (2013) Capture the Fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24:2135–2152
Javaid MK, Kyer C, Mitchell PJ et al (2015) Effective secondary fracture prevention: implementation of a global benchmarking of clinical quality using the IOF Capture the Fracture(R) Best Practice Framework tool. Osteoporos Int 26:2573–2578
Wu CH, Tu ST, Chang YF, Chan DC, Chien JT, Lin CH, Singh S, Dasari M, Chen JF, Tsai KS (2018) Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: a systematic literature review and meta-analysis. Bone 111:92–100
Wu CH, Kao IJ, Hung WC, Lin SC, Liu HC, Hsieh MH, Bagga S, Achra M, Cheng TT, Yang RS (2018) Economic impact and cost-effectiveness of fracture liaison services: a systematic review of the literature. Osteoporos Int 29:1227–1242
Ganda K, Puech M, Chen JS, Speerin R, Bleasel J, Center JR, Eisman JA, March L, Seibel MJ (2013) Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int 24:393–406
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Szulc P, Munoz F, Marchand F, Delmas PD (2001) Semiquantitative evaluation of prevalent vertebral deformities in men and their relationship with osteoporosis: the MINOS study. Osteoporos Int 12:302–310
Genant HK, Jergas M, Palermo L, Nevitt M, Valentin RS, Black D, Cummings SR (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis The Study of Osteoporotic Fractures Research Group. J Bone Miner Res 11:984–996
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY, Scientific Advisory Board of the European Society for C, Economic Aspects of O, Osteoarthritis, the Committee of Scientific Advisors of the International Osteoporosis F (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24:23–57
Cawthon PM, Haslam J, Fullman R, Peters KW, Black D, Ensrud KE, Cummings SR, Orwoll ES, Barrett-Connor E, Marshall L, Steiger P, Schousboe JT, Osteoporotic Fractures in Men (MrOS) Research Group (2014) Methods and reliability of radiographic vertebral fracture detection in older men: the osteoporotic fractures in men study. Bone 67:152–155
Jager PL, Jonkman S, Koolhaas W, Stiekema A, Wolffenbuttel BH, Slart RH (2011) Combined vertebral fracture assessment and bone mineral density measurement: a new standard in the diagnosis of osteoporosis in academic populations. Osteoporos Int 22:1059–1068
Majumdar SR, McAlister FA, Johnson JA et al (2012) Interventions to increase osteoporosis treatment in patients with ‘incidentally’ detected vertebral fractures. Am J Med 125:929–936
Majumdar SR, Lier DA, McAlister FA, Rowe BH, Siminoski K, Hanley DA, Russell AS, Johnson JA (2013) Cost-effectiveness of osteoporosis interventions for ‘incidental’ vertebral fractures. Am J Med 126(169):e169–e117
Majumdar SR, Beaupre LA, Harley CH, Hanley DA, Lier DA, Juby AG, Maksymowych WP, Cinats JG, Bell NR, Morrish DW (2007) Use of a case manager to improve osteoporosis treatment after hip fracture: results of a randomized controlled trial. Arch Intern Med 167:2110–2115
Kuiper BW, Graybill S, Tate JM, Kaufman N, Bersabe D (2018) After the fall: improving osteoporosis treatment following hip fracture. Osteoporos Int 29:1295–1301
Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW (2007) Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. Jama 297:831–841
Horwitz LI, Moriarty JP, Chen C, Fogerty RL, Brewster UC, Kanade S, Ziaeian B, Jenq GY, Krumholz HM (2013) Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med 173:1715–1722
Albrecht JS, Gruber-Baldini AL, Hirshon JM, Brown CH, Goldberg R, Rosenberg JH, Comer AC, Furuno JP (2014) Hospital discharge instructions: comprehension and compliance among older adults. J Gen Intern Med 29:1491–1498
Archbold RA, Laji K, Suliman A, Ranjadayalan K, Hemingway H, Timmis AD (1998) Evaluation of a computer-generated discharge summary for patients with acute coronary syndromes. Br J Gen Pract 48:1163–1164
Kattel S, Manning DM, Erwin PJ, Wood H, Kashiwagi DT, Murad MH (2016) Information transfer at hospital discharge: a systematic review. J Patient Saf. https://doi.org/10.1097/PTS.0000000000000248
Boudreau DM, Yu O, Balasubramanian A, Wirtz H, Grauer A, Crittenden DB, Scholes D (2017) A survey of women’s awareness of and reasons for lack of postfracture osteoporotic care. J Am Geriatr Soc 65:1829–1835
Merle B, Chapurlat R, Vignot E, Thomas T, Haesebaert J, Schott AM (2017) Post-fracture care: do we need to educate patients rather than doctors? The PREVOST randomized controlled trial. Osteoporos Int 28:1549–1558
Kastner M, Perrier L, Munce SEP, Adhihetty CC, Lau A, Hamid J, Treister V, Chan J, Lai Y, Straus SE (2018) Complex interventions can increase osteoporosis investigations and treatment: a systematic review and meta-analysis. Osteoporos Int 29:5–17
Mendis AS, Ganda K, Seibel MJ (2017) Barriers to secondary fracture prevention in primary care. Osteoporos Int 28:2913–2919
Acknowledgments
We thank the team of the Division of General Internal Medicine for the blood tests performed for the serum calcium-phosphate biochemistry, the team of the Division of Nuclear Medicine for DXA measurements, Michelle Le Braz and François Herrmann, MD, MPH, for help in statistical analysis.
Funding sources
This work was funded in part by an unrestricted grant from the Edmond J. Safra Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical approval
The study was conducted in accordance with the ethical standards of the institutional research committee and the 1964 Helsinki Declaration and its later amendments.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Table 1
(DOC 44 kb)
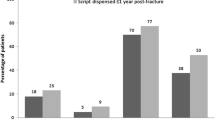
Supplementary Figure 1
Distribution (%) of vertebral fractures in outpatient care (white columns) and inpatient care (gray columns). (PNG 237 kb)
Rights and permissions
About this article
Cite this article
Spechbach, H., Fabreguet, I., Saule, E. et al. Higher rates of osteoporosis treatment initiation and persistence in patients with newly diagnosed vertebral fracture when introduced in inpatients than later in outpatients. Osteoporos Int 30, 1353–1362 (2019). https://doi.org/10.1007/s00198-019-04900-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-04900-3