Abstract
Summary
The extent of Canadian provincial variation in hip fracture surgical timing is unclear. Provinces performed a similar proportion of surgeries within three inpatient days after adjustment. Time to surgery varied by timing of admission across provinces. This may reflect different approaches to providing access to hip fracture surgery.
Introduction
The aim of this study was to compare whether time to surgery after hip fracture varies across Canadian provinces for surgically fit patients and their subgroups defined by timing of admission.
Methods
We retrieved hospitalization records for 140,235 patients 65 years and older, treated surgically for hip fracture between 2004 and 2012 in Canada (excluding Quebec). We studied the proportion of surgeries on admission day and within 3 inpatient days, and times required for 33%, 66%, and 90% of surgeries across provinces and by subgroups defined by timing of admission. Differences were adjusted for patient, injury, and care characteristics.
Results
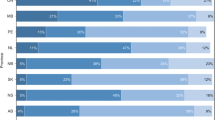
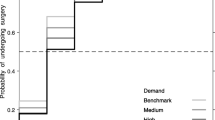
Overall, provinces performed similar proportions of surgeries within the recommended three inpatient days, with all provinces requiring one additional day to perform the recommended 90% of surgeries. Prince Edward Island performed 7.0% more surgeries on admission day than Ontario irrespective of timing of admission (difference = 7.0; 95% CI 4.0, 9.9). The proportion of surgeries on admission day was 6.3% lower in Manitoba (difference = − 6.3; 95% CI − 12.1, − 0.6), and 7.7% lower in Saskatchewan (difference = − 7.7; 95% CI − 12.7, − 2.8) compared to Ontario. These differences persisted for late weekday and weekend admissions. The time required for 33%, 66%, and 90% of surgeries ranged from 1 to 2, 2–3, and 3–4 days, respectively, across provinces by timing of admission.
Conclusions
Provinces performed similarly with respect to recommended time for hip fracture surgery. The proportion of surgeries on admission day, and time required to complete 33% and 66% of surgeries, varied across provinces and by timing of admission. This may reflect different provincial approaches to providing access to hip fracture surgery.


Similar content being viewed by others
References
Leslie WD, O'Donnell S, Jean S, Lagace C, Walsh P, Bancej C, Morin S, Hanley DA, Papaioannou A (2009) Trends in hip fracture rates in Canada. JAMA 302(8):883–889. https://doi.org/10.1001/jama.2009.1231
Sobolev B, Guy P, Sheehan KJ et al (2016) Hospital mortality after hip fracture surgery in relation to length of stay by care delivery factors. Medicine 96(16):e6683
Moja L, Piatti A, Pecoraro V, Ricci C, Virgili G, Salanti G, Germagnoli L, Liberati A, Banfi G (2012) Timing matters in hip fracture surgery: patients operated within 48 hours have better outcomes. A meta-analysis and meta-regression of over 190,000 patients. PLoS One 7(10):e46175. https://doi.org/10.1371/journal.pone.0046175
Beloosesky Y, Grinblat J, Pirotsky A, Weiss A, Hendel D (2004) Different C-reactive protein kinetics in post-operative hip-fractured geriatric patients with and without complications. Gerontology 50(4):216–222. https://doi.org/10.1159/000078350
Beloosesky Y, Hendel D, Weiss A, Hershkovitz A, Grinblat J, Pirotsky A, Barak V (2007) Cytokines and C-reactive protein production in hip-fracture-operated elderly patients. J Gerontol A Biol Sci Med Sci 62(4):420–426. https://doi.org/10.1093/gerona/62.4.420
Canadian Institute for Health Information (2007) Health indicators. https://secure.cihi.ca/free_products/hi07_health_indicators_2007_e.pdf. Accessed 18 Aug 2017
Canadian Institute for Health Information (2006) Final report of the federal advisor on wait times. https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/health-care-system/final-report-federal-advisor-wait-times.html. Accessed 18 Aug 2017
Government of Canada (1984). Canada health act. http://laws-lois.justice.gc.ca/eng/acts/C-6/page-2html#h-3. Accessed 22 Aug 2017
Allin S (2008) Does equity in healthcare use vary across Canadian provinces? Healthc Policy 3(4):83–99
Siciliani L, Borowitz M, Moran V (2013) Waiting time policies in the health sector: what works? OECD Publishing, Paris
Canadian Institute for Health Information (2017) Wait times for priority procedures in Canada. https://www.cihi.ca/sites/default/files/document/wait-times-report-2017_en.pdf. Accessed 18 Aug 2017
Ahmed I, Khan MA, Nayak V, Mohsen A (2014) An evidence-based warfarin management protocol reduces surgical delay in hip fracture patients. J Orthop Traumatol 15(1):21–27. https://doi.org/10.1007/s10195-013-0274-7
Siegmeth AW, Gurusamy K, Parker MJ (2005) Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br 87(8):1123–1126. https://doi.org/10.1302/0301-620X.87B8.16357
Orosz GM, Magaziner J, Hannan EL, Morrison RS, Koval K, Gilbert M, McLaughlin M, Halm EA, Wang JJ, Litke A, Silberzweig SB, Siu AL (2004) Association of timing of surgery for hip fracture and patient outcomes. JAMA 291(14):1738–1743. https://doi.org/10.1001/jama.291.14.1738
Orosz GM, Hannan EL, Magaziner J, Koval K, Gilbert M, Aufses A, Straus E, Vespe E, Siu AL (2002) Hip fracture in the older patient: reasons for delay in hospitalization and timing of surgical repair. J Am Geriatr Soc 50(8):1336–1340. https://doi.org/10.1046/j.1532-5415.2002.50353.x
Ricci WM, Brandt A, McAndrew C, Gardner MJ (2015) Factors affecting delay to surgery and length of stay for patients with hip fracture. J Orthop Trauma 29(3):e109–e114. https://doi.org/10.1097/BOT.0000000000000221
Charalambous CP, Yarwood S, Paschalides C, Siddique I, Hirst P, Paul A (2003) Factors delaying surgical treatment of hip fractures in elderly patients. Ann R Coll Surg Engl 85(2):117–119. https://doi.org/10.1308/003588403321219911
Fantini MP, Fabbri G, Laus M, Carretta E, Mimmi S, Franchino G, Favero L, Rucci P (2011) Determinants of surgical delay for hip fracture. Surgeon 9(3):130–134. https://doi.org/10.1016/j.surge.2010.11.031
Ryan DJ, Yoshihara H, Yoneoka D, Egol KA, Zuckerman JD (2015) Delay in hip fracture surgery: an analysis of patient-specific and hospital-specific risk factors. J Orthop Trauma 29(8):343–348. https://doi.org/10.1097/BOT.0000000000000313
Ventura C, Trombetti S, Pioli G, Belotti LM, De PR (2014) Impact of multidisciplinary hip fracture program on timing of surgery in elderly patients. Osteoporos Int 25(11):2591–2597. https://doi.org/10.1007/s00198-014-2803-5
Zeltzer J, Mitchell RJ, Toson B, Harris IA, Close J (2014) Determinants of time to surgery for patients with hip fracture. ANZ J Surg 84(9):633–638. https://doi.org/10.1111/ans.12671
Nijland LMG, Karres J, Simons AE, Ultee JM, Kerkhoffs G, Vrouenraets BC (2017) The weekend effect for hip fracture surgery. Injury 48(7):1536–1541. https://doi.org/10.1016/j.injury.2017.05.017
Sayers A, Whitehouse MR, Berstock JR, Harding KA, Kelly MB, Chesser TJ (2017) The association between the day of the week of milestones in the care pathway of patients with hip fracture and 30-day mortality: findings from a prospective national registry—the National Hip Fracture Database of England and Wales. BMC Med 15(1):62. https://doi.org/10.1186/s12916-017-0825-5
Sheehan KJ, Sobolev B, Guy P, Bohm E, Hellsten E, Sutherland JM, Kuramoto L, Jaglal S (2015) Constructing an episode of care from acute hospitalization records for studying effects of timing of hip fracture surgery. J Orthop Res 34(2):197–204. https://doi.org/10.1002/jor.22997
Sobolev B, Guy P, Sheehan KJ et al (2016) Time trends in hospital stay after hip fracture in Canada, 2004-2012: database study. Arch Osteoporos 11(1):13. https://doi.org/10.1007/s11657-016-0264-5
Centre NCG (2011) “6. Timing of surgery.” The management of hip fracture in adults. Royal College of Physicians (UK), London
Sheehan KJ, Sobolev B, Guy P, Tang M, Kuramoto L, Belmont P, Blair JA, Sirett S, Morin SN, Griesdale D, Jaglal S, Bohm E, Sutherland JM, Beaupre L, Canadian Collaborative Study on Hip Fractures (2017) Feasibility of using administrative data for identifying medical reasons to delay hip fracture surgery. BMJ Open 7(4):e015368. https://doi.org/10.1136/bmjopen-2016-015368
Vidan MT, Sanchez E, Gracia Y, Maranon E, Vaquero J, Serra JA (2011) Causes and effects of surgical delay in patients with hip fracture: a cohort study. Ann Intern Med 155(4):226–233. https://doi.org/10.7326/0003-4819-155-4-201108160-00006
Canadian Institute for Health Information (2005) Technical note for analyses of hip fracture admissions. https://secure.cihi.ca/free_products/WaitTimesReport_tech_Hip_e.pdf. Accessed 18 Aug 2017
Hosmer DW Jr, Lemeshow S (1989) Applied logistic regression. John Wiley & Sons, New York
StataCorp (2013) Stata treatment-effects reference manual: potential outcomes/counterfactual outcomes release 13. http://www.stata.com/manuals13/te.pdf. Accessed 21 Aug 2017
StataCorp (2015) Stata 14 base reference manual. Stata Press, College Station
Mood AF, Graybill FA, Boes DC (1963) Introduction to the theory of statistics. McGraw-Hill, New York
Machado JAF, Silva JMCS (2005) Quantiles for counts. J Am Stat Assoc 100(472):1226–1237. https://doi.org/10.1198/016214505000000330
Winkelmann R (2006) Reforming health care: evidence from quantile regressions for counts. J Health Econ 25(1):131–145. https://doi.org/10.1016/j.jhealeco.2005.03.005
Wu H, Gao L, XZhang Z, ASCE M (2014) Analysis of crash data using quantile regression for counts. Jounral of Transport Engineering 140(4):04013025–04013021. https://doi.org/10.1061/(ASCE)TE.1943-5436.0000650
Health Quality Ontario & Ministry of Health and Long-Term Care (2013) Quality-based procedures: clinical handbook for hip fracture. Toronto, http://www.health.gov.on.ca/en/pro/programs/ecfa/docs/qbp_hipfracture.pdf. Accessed on 21 Aug 2017
Sheehan KJ, Villa Y, Sobolev B, Guy P (2017) Patient and system factors of timing of hip fracture surgery: a scoping review. BMJ Open 7(8):e016939. https://doi.org/10.1136/bmjopen-2017-016939
StataCorp (2015) Statistical software: release 14. StataCorp LP, College Station
Canadian Institute for Health Information (2014) Benchmarks for treatment and wait time in Canada: hip fracture repair. https://secure.cihi.ca/free_products/2014_WaitTimesAiB_EN.pdf. Accessed 21 Aug 2017
Moran CG, Wenn RT, Sikand M, Taylor AM (2005) Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am 87(3):483–489. https://doi.org/10.2106/00004623-200503000-00001
Kristensen PK, Thillemann TM, Johnsen SP (2014) Is bigger always better? A nationwide study of hip fracture unit volume, 30-day mortality, quality of in-hospital care, and length of hospital stay. Med Care 52(12):1023–1029. https://doi.org/10.1097/MLR.0000000000000234
Canadian Institute for Health Information (2012) Health Indicators 2012. https://secure.cihi.ca/free_products/health_indicators_2012_en.pdf. Accessed 21 Aug 2017
Canadian Medical Association (2015) Number of physicians by Province/Territory and specialty, Canada. Canadian Medical Association Masterfile https://www.cma.ca/Assets/assets-library/document/en/advocacy/01-physicians-by-Specialty-Province-2015-e.pdf. Accessed 21 Aug 2017
Desai SJ, Patel J, Abdo H, Lawendy AR, Sanders D (2014) A comparison of surgical delays in directly admitted versus transferred patients with hip fractures: opportunities for improvement? Can J Surg 57(1):40–43. https://doi.org/10.1503/cjs.002613
Jean S, O'Donnell S, Lagace C et al (2013) Trends in hip fracture rates in Canada: an age-period-cohort analysis. J Bone Miner Res 28(6):1283–1289. https://doi.org/10.1002/jbmr.1863
Acknowledgements
We gratefully acknowledge the guidance from the CIHI experts in understanding the discharge abstracts.
The following are members of the Canadian Collaborative Study on Hip Fractures: Lauren Beaupre, Eric Bohm, Michael Dunbar, Donald Griesdale, Pierre Guy, Edward Harvey, Erik Hellsten, Susan Jaglal, Hans Kreder, Lisa Kuramoto, Adrian Levy, Suzanne N. Morin, Katie J. Sheehan, Boris Sobolev, Jason M. Sutherland, and James Waddell.
Funding
This research was funded by the Canadian Institutes of Health Research. This funder had no role in the design of this study, execution, analyses, data interpretation, or decision to submit results for publication.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
The University of British Columbia’s Behavioural Research Ethics Board approved this study (H11-02611).
Conflicts of interest
The following competing interests are declared: (1) PG has received grants from the Canadian Institutes of Health Research related to this work. PG also receives funding from the Natural Sciences and Engineering Research Council of Canada, and the Canadian Foundation for Innovation and the British Columbia Specialists Services Committee for work around hip fracture care not related to this manuscript. He has also received fees from the BC Specialist Services Committee (for a provincial quality improvement project on redesign of hip fracture care) and from Stryker Orthopedics (as a product development consultant). He is a board member and shareholder in Traumis Surgical Systems Inc. and a board member for the Canadian Orthopedic Foundation. He also serves on the speakers’ bureaus of AO Trauma North America and Stryker Canada. (2) SNM reports research grants from Amgen Canada and from Merck. (3) JDK is a research assistant, and AC is a postdoctoral fellow whose salary is paid by Canadian Institutes of Health Research funding related to this work. (4) BS, LK, KS, CF, EB, LB, JMS, MD, DG, and EH declare they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Sheehan, K.J., Filliter, C., Sobolev, B. et al. Time to surgery after hip fracture across Canada by timing of admission. Osteoporos Int 29, 653–663 (2018). https://doi.org/10.1007/s00198-017-4333-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4333-4