Abstract
Summary
This study revealed the risk of major osteoporotic fracture in patients with sarcoidosis exposed to glucocorticoids. Current use of glucocorticoids was associated with a risk of fracture, with no difference between patients with and without sarcoidosis. Sarcoidosis per se was not associated with an increased fracture risk.
Introduction
Sarcoidosis is a multi-organ, chronic inflammatory, granulomatous disorder that most frequently affects the lungs, lymph nodes, skin, eyes, and liver, but may occur in any organ, including the bones. While oral glucocorticoids (GCs) are commonly used as initial treatment, little is known about the risk of major osteoporotic fractures in patients with sarcoidosis exposed to GCs.
Methods
A case-control study was conducted using the Danish National Hospital Discharge Registry (NHDR) between January 1995 and December 2011. Conditional logistics regression models were used to derive adjusted odds ratios (OR) of major osteoporotic fractures in subjects with and without sarcoidosis stratified by average daily and cumulative dose exposures.
Results
A total of 376,858 subjects with a major osteoporotic fracture and the same number of subjects without this event were identified (mean age 64.2 ± 19.5 years, 69% female). In patients with sarcoidosis (n = 124), current use of GC was associated with an increased risk of major osteoporotic fracture (adjusted (adj.) OR 1.74; 95% CI 1.17–2.58), which dropped to baseline levels after discontinuation. In subjects without sarcoidosis, this risk was comparable (adj. OR 1.36; 95% CI 1.32–1.40). In sarcoidosis patients, cumulative dose 1.0–4.9 g and >10 g prednisolone equivalents were associated with increased risk of major osteoporotic fracture (adj. OR 2.75; 95% CI 1.06–7.14 and 2.22; 95% CI 1.17–4.22, respectively), whereas a cumulative dose of <1.0 g and 5.0–9.9 g was not associated with major osteoporotic fracture risk.
Conclusion
Both in subjects with and without sarcoidosis, current expose to GC is associated with increased risk of major osteoporotic fractures, with no between-group difference. Sarcoidosis per se was not associated with increased fracture risk. Having sarcoidosis per se, i.e., if not treated with GC, is not a risk factor for fracture, and such patients may only need risk assessment when they commence GC therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sarcoidosis is a multisystem, chronic inflammatory, granulomatous disease of unknown etiology that primarily affects the lungs, lymph nodes, skin, eyes, and liver. However, almost all organs of the body may be involved, including the musculoskeletal system [1]. The annual incidence of the disease ranges from 5 to 40 cases per 100,000 individuals worldwide. High-dose systemic glucocorticoids (GCs) have been the cornerstone of initial treatment. Although their exact mechanism of action in the treatment of sarcoidosis remains unknown, they are considered to suppress the granulomatous inflammatory process [2]. Typical regimens range from 20 to 40 mg oral prednisolone equivalents per day for 4 to 6 weeks, and may then be tapered off, depending on the severity of the underlying disease [1, 2]. Treatment with GCs has been associated with a decrease in BMD and an increased fracture risk, particularly fractures of the hip and vertebrae [3]. The onset of GC-induced fracture risk occurs rapidly, increases with higher average daily doses, and drops quickly to baseline after discontinuation [4, 5].
In addition, a limited number of studies have assessed fracture risk in patients with sarcoidosis. A cross-sectional study in 124 patients with sarcoidosis exposed to GCs reported a prevalence of 20% of vertebral deformities; a separate study showed 32% vertebral deformities over a period of 4 years later, although no reduced BMD was observed [6, 7]. Another cross-sectional study with 142 patients showed similar results; vertebral fractures occurred in 24% of patients whereas a normal mean BMD was found [7]. These data suggest an increased risk of vertebral fractures in patients with sarcoidosis, which is not reflected by changes in BMD [6,7,8]. A large observational cohort study using data from the UK Clinical Practice Research Datalink showed a doubled risk of osteoporotic fracture (spine, hip, forearm, or humerus fracture) in sarcoidosis patients who had received >10 mg prednisone per day [9]. Whether or not sarcoidosis per se is a risk factor for fractures is currently unknown. Also, the potential relation with the type of osteoporotic fracture is unclear.
The objectives of the current study were to study the risk of major osteoporotic fractures in patients with and without sarcoidosis and investigate the relation with average and cumulative GC exposure and the type of major osteoporotic fractures in both these groups.
Methods
Source population
A population-based case-control study was conducted using electronic medical records from the Danish National Database. In Denmark, separate registers of computerized medical records on all contacts to hospitals and on the use of drugs can be linked for the entire population (approximately 5.5 million inhabitants) [10]. Information on hospital admissions is kept in the National Hospital Discharge Register. The register was founded in 1977 and covers all inpatients contacts from 1977 to 1994 and from 1995 onwards as well as all outpatient visits to hospitals, outpatient clinics, and emergency rooms. Upon discharge, the physician codes the reason for the contact according to the International Classification of Diseases (ICD) system. The register has nationwide coverage of public hospitals with an almost 100% completeness of recordings and a high precision of diagnoses [10, 11], particularly for fracture diagnoses [12].
The Danish Medicines Agency keeps a nationwide prescription database, the Register of Medicinal Product Statistics, with key information on prescriptions for refundable drugs. The prescription database includes information on the patient’s civil registry number, the type and amount of drug prescribed according to the Anatomical Therapeutical Chemical (ATC) classification system [13], and the date when the prescription was filled. The database started on January 1, 1994 and has been updated hereafter. All registers can be linked through the use of the civil registry number that is assigned to all Danish citizens [14].
Study population/outcome
Cases were all subjects aged 18 years and older, who had sustained a major osteoporotic fracture between 1 January 1995 and 31 December 2011. A major osteoporotic fracture was defined as a fracture of the hip (ICD10 code S72.0–S72.2), radius/ulna (S52), vertebrae (S12, S22.0–S22.1, S32.0–S32.2, S32.7, S32.8, T08), or humerus (S42.2–S42.4) according to the World Health Organization’s (WHO) definition [15]. To each case, a control subject who did not sustain a major osteoporotic fracture was randomly matched by gender and year of birth using the incidence-density sampling technique [16]. The date of the first major osteoporotic fracture defined the index date. Controls received the same index date as their matched cases. This database has been reported to have a quality recording of patient’s diagnosis [11] and has been used in studies on patients with sarcoidosis [17,18,19].
Exposure
Sarcoidosis before the index date was determined based on ICD-10 code (D86). In addition, we evaluated GC use before the index date for all patients. Based on the time since the most recent GC prescription prior to the index date, patients were classified as current (>0–3 months), recent (4–6 months), past (7–12 months), or distant past (>1 year) users.
For each current GC user, the cumulative and average daily GC exposures were estimated. The cumulative dose was calculated by adding up all previous GC prescriptions using the World Health Organization’s defined daily dosages (DDDs) [5]. The average daily dose was calculated by dividing the cumulative GC exposure by the treatment time (i.e., the time between the first GC prescription and the index date). GC exposure was expressed as oral prednisolone equivalents using average daily and cumulative dose. Cumulative dose was classified as <1.0, 1.0–4.9, 5.0–9.9, or ≥10 g [5].
We considered the following potential confounders before the index date: a history of chronic obstructive pulmonary disease (COPD), a previous fracture, rheumatoid arthritis, inflammatory bowel disease (IBD), or secondary osteoporosis (type 1 diabetes, hyperthyroidism, hypogonadism, or renal failure). Other potential confounders included a prescription in the 6 months before the index date of the following drugs: bisphosphonates, vitamin D, calcium, raloxifene, strontium, denosumab, calcitonin, parathyroid hormone, hormone replacement therapy, inhaled corticosteroids, inhaled bronchodilators, antipsychotics, antidepressants, hypnotics/anxiolytics, anticonvulsants, and anti-Parkinson drugs.
Statistical analysis
Conditional logistic regression was used to estimate odds ratios (ORs) for fracture risk (SAS 9.3). Final regression models were determined by stepwise backward elimination using a significance level of 0.05. Analysis was stratified by current, recent, past, and distant GC use in patients with sarcoidosis and without sarcoidosis. We also stratified individuals according to their cumulative and average daily dose of systemic GC exposure. Additionally, we analyzed the risk of hip, radius/ulna, and clinically symptomatic vertebral fractures among current GC users. All results were presented as ORs with corresponding 95% confidence intervals (CIs).
Results
A total of 376,858 subjects, with a major osteoporotic fracture and the same number of subjects without such fracture, were included. Table 1 shows the baseline characteristics. The mean age of our population was 64.2 ± 19.5 years, and 69% were female. About 5% of the cases (n = 19,476) and 4% of the controls (n = 13,734) had used GCs in the 6 months before the index date. There was a previous history of fracture in 26.3% of the cases and 8.3% of the controls. A higher proportion of cases had used anticonvulsants, hypnotics, anxiolytics, and antidepressants in the 6 months prior to index date. There were 493 (0.1%) patients with sarcoidosis among the cases and 402 (0.1%) among the controls with adjusted (adj.) OR of 1.14 and 95% CI of 0.99–1.31.
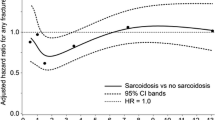
Table 2 shows GC use and the risk of a major osteoporotic fracture among patients with sarcoidosis and without sarcoidosis stratified by GC use. Among subjects with a major osteoporotic fracture, 263 patients had a diagnosis of sarcoidosis and GC use compared with 182 in controls. In patients with sarcoidosis, current use of GC was associated with an increased risk of major osteoporotic fracture (adj. OR 1.74; 95% CI 1.17–2.58) compared to never GC using subjects without sarcoidosis. No association was seen with recent use of GC in patients with sarcoidosis (adj. OR 1.47; 95% CI 0.72–3.01). Similarly, distant and past GC use was not associated with an increased risk.
In subjects without sarcoidosis, current use of GCs was associated with an increased risk of major osteoporotic fracture compared to never GC using subjects with sarcoidosis (adj. OR 1.36; 95% CI 1.32–1.40). The risk of major osteoporotic fracture in patients with recent exposure to GCs without sarcoidosis was marginally increased (adj. OR 1.11; 95% CI 1.06–1.16). However, past and distant GC use was not associated with major osteoporotic fracture risk. There was no difference in risk of major osteoporotic fracture with current GC use between subjects with and without sarcoidosis (p value Wald test = 0.23).
Current GC use was associated with increased risk of hip fracture in both sarcoidosis subjects (adj. OR 3.80; 95% CI 1.23–11.50) and patients without sarcoidosis (adj. OR 1.55; 95% CI 1.47–1.64). Similarly, the risk of clinically symptomatic vertebral fracture was increased with current GC use in patients with sarcoidosis (adj. OR 6.05; 95% CI 1.59–23.00) and without sarcoidosis (adj. OR 2.35; 95% CI 2.14–2.59). The risk of radius/ulna fractures was not associated with current GC use in patients with sarcoidosis (adj. OR 1.09; 95% CI 0.64–1.87) while the risk was slightly elevated among subjects without sarcoidosis (adj. OR 1.08; 95% CI 1.03–1.13; Table 3).
Table 4 shows GC exposure and risk of major osteoporotic fracture stratified by average daily dose and cumulative daily dose in sarcoidosis and non-sarcoidosis. Current GC use was further stratified by average daily dose. Average daily dose <7.5 and ≥15 mg prednisolone equivalents was not associated with a risk of major osteoporotic fracture in sarcoidosis patients (adj. OR <7.5 mg 1.37; 95% CI 0.79–2.40; adj. OR ≥15 mg 1.22; 95% CI 0.54–2.74). Average daily dose 7.5–14.9 mg prednisolone equivalent was associated with an increased risk of major osteoporotic fracture (adj. OR 3.62; 95% CI 1.59–8.26) compared to never GC use in patients with sarcoidosis.
Current GC use was also stratified by cumulative dose among sarcoidosis patients. A cumulative dose 1.0–4.9 and >10 g prednisolone equivalent was associated with an increased risk of major osteoporotic fracture (adj. OR 2.75; 95% CI 1.06–7.14 and 2.22; 95% CI 1.17–4.22, respectively), whereas a cumulative dose of <1.0 and 5.0–9.9 g was not associated with major osteoporotic fracture risk as compared to never GC use (adj. OR 1.34; 95% CI 0.33–5.39 and 1.03; 95% CI 0.51–2.08, respectively).
In subjects without sarcoidosis, a dose-response relationship was observed between average daily dose and major osteoporotic fracture risk. The highest risk was seen among patients without sarcoidosis who received ≥15 mg prednisolone equivalents (adjusted OR 1.79; 95% CI 1.66–1.92). The risk of major osteoporotic fractures increased with increase in cumulative GC dose. However, this trend was lost at a cumulative dose ≥10 g prednisolone equivalent (adjusted OR 1.43; 95% CI 1.35–1.51).
Discussion
We found that currently using GC patients with sarcoidosis have a 1.7-fold increased risk of major osteoporotic fracture compared to never GC users without sarcoidosis. This risk was mainly related to hip and clinically symptomatic vertebral fractures and was comparable to that in subjects without sarcoidosis. Also, sarcoidosis per se was not associated with increased risk of major osteoporotic fractures. Among subjects with and without sarcoidosis, the risk of osteoporotic fractures quickly disappeared after cessation of GC use. In contrast to subjects without sarcoidosis, there was no dose-related increase in the risk of major osteoporotic fractures with increasing daily and cumulative dose among sarcoidosis patients.
The findings from our study are consistent with a population-based cohort study in patients with sarcoidosis using data from the Clinical Practice Research Datalink (CPRD), which found an increased risk of any fracture (adjusted OR 1.50; 95% CI 1.20–1.89) among sarcoidosis patients with exposure to systemic GCs compared to non-users of GCs with sarcoidosis [9]. In that study, exposure was defined as systemic GCs use in the previous 6 months, which compares to current and recent GC exposure together in our study. Similarly, we found an increased risk of major osteoporotic fracture among non-sarcoidosis patients with current GC use compare to never GC use. Furthermore, we tested the risk of major osteoporotic fractures in current GC users with and without sarcoidosis. We found no difference in the two groups, which suggest that the disease itself may not increase the risk of major osteoporotic fracture. Various studies, evaluating fracture risk with GC use but with no particular focus on patients with sarcoidosis, have reported an increased risk of fracture with current GC use [5, 20, 21].
Some studies in other groups have reported a dose-dependent increase in the risk of fractures, with varying explanations for the perceived increased risk observed [22, 23]. However, Bours et al. [9] also found that fracture risk did not increase significantly with increased daily or cumulative dose in patients with sarcoidosis. This was in line with our observation among patients with sarcoidosis. Nevertheless, in patients without sarcoidosis, a dose-related increased risk of major osteoporotic fracture with increase in cumulative and average daily dose of GCs was observed. It is important to note that the dose-response relationship disappeared at a cumulative dose ≥10 g, which might indicate a dose threshold. In a case-control study conducted in Denmark, increase in cumulative dose of corticosteroids was associated with increased risk of hip fractures [24]. Another study, which evaluated fracture risks with use of GCs, concluded that current exposure to daily dose ≥15 mg and cumulative exposure ≤1 g resulted in a small increased risk of osteoporotic fracture [9]. Also, the risk increased with increasing cumulative exposure [9]. The lack of a dose-related increased risk of major osteoporotic fracture in sarcoidosis patients enrolled in our study was likely due to the small number of patients in each dose category. However, it is also possible that other factors, including disease activity, dietary intake, or decreased physical activity, contribute to increased fracture risk in GC using sarcoidosis patients. This warrants further study.
Although the exact mechanism of major osteoporotic fracture in patients with sarcoidosis exposed to GCs remains unknown, it might be due to a complex interplay of factors. Researchers have always linked this to low BMD in patients. Various studies showed normal BMD in patients with sarcoidosis [7, 8, 25, 26] even in those undergoing GC therapy [8] although a study carried out among postmenopausal women showed a decrease in BMD [27]. The actual reason for this is unknown but it is hypothesized that in patients with sarcoidosis, mechanisms exist which compensate for the effect of inflammatory cytokines on osteoclastogenesis and bone resorption [9, 28]. Low dietary calcium is correlated with low BMD and increase fracture risk [7]. There is an increased risk of sarcopenia in patients with increased risk of bone loss [29]. Higher levels of 25(OH)D and 1.25(OH)D are associated with the increased risk of fracture and bone resorption in sarcoidosis [22]. Likewise, other factors such as CRP and calcium levels could potentially affect the risk of fractures in patients with sarcoidosis [9, 22, 23, 30, 31].
The main strength of our study was the large sample size among case and control populations. This was possible because our study was conducted using the Danish National database with approximately 5 million anonymised patient records from across Denmark [10]. We were also able to adjust for a wide range of covariates. Our limitations included the lack of information on smoking, alcohol use, inflammatory markers, muscle mass or strength, and BMD as such we could not adjust for these potential confounders in our analysis. There is also a potential of missed diagnosis of sarcoidosis due to the different clinical presentation of the disease. We could not independently confirm the predictive values of cases diagnosed with a fracture by a general practitioner. However, a high positive predictive value (93%) of diagnosis of fractures has been reported in the Danish database [24], thereby limiting the possibility of misclassification of cases and controls in our study. As with most observational studies, we could not rule out the possibility of misclassification of exposure to GCs. Information on potential treatment received prior to entry into the Danish National database was also not available. There is a chance that vertebral fractures may have been underrepresented in the study population; however, we expect that this will affect both sarcoidosis and non-sarcoidosis patients (non-differential misclassification).
In conclusion, we found that current GC use was associated with an increased risk of major osteoporotic fracture compared to never GC use in subjects with and without sarcoidosis. There was no dose-related increase in risk of a major osteoporotic fracture with increasing daily and cumulative dose among sarcoidosis patients as was seen in patients without sarcoidosis. The risk of major osteoporotic fractures was comparable in current GC users with and without sarcoidosis, which suggests that the disease itself may not increase the risk of major osteoporotic fractures and that is mainly related to GC use. Patients currently exposed to GC are particularly vulnerable to increased fracture risk as such clinicians should consider regular fracture risk assessment to detect changes in bone integrity and may contemplate the initiation of osteoporosis treatment when necessary in patients with sarcoidosis. Having sarcoidosis per se, i.e., if not treated with GC, is not a risk factor for fracture, and such patients may only need risk assessment when they commence GC therapy.
References
Valeyre D, Prasse A, Nunes H et al (2014) Sarcoidosis. Lancet 383:1155–1167. doi:10.1016/S0140-6736(13)60680-7
Baughman RP, Costabel U, du Bois RM (2016) Treatment of sarcoidosis. Clin Chest Med 29:533–548. doi:10.1016/j.ccm.2008.03.012
Majumdar SR, Morin SN, Lix LM, Leslie WD (2013) Influence of recency and duration of glucocorticoid use on bone mineral density and risk of fractures: population-based cohort study. Osteoporos Int 24:2493–2498. doi:10.1007/s00198-013-2352-3
Van Staa TP, Leufkens HG, Abenhaim L et al (2000) Use of oral corticosteroids and risk of fractures. J Bone Min Res 15:993–1000. doi:10.1359/jbmr.2000.15.6.993
De Vries F, Bracke M, Leufkens HGM et al (2007) Fracture risk with intermittent high-dose oral glucocorticoid therapy. Arthritis Rheum 56:208–214. doi:10.1002/art.22294
Heijckmann AC, Drent M, Dumitrescu B et al (2008) Progressive vertebral deformities despite unchanged bone mineral density in patients with sarcoidosis: a 4-year follow-up study. Osteoporos Int 19:839–847. doi:10.1007/s00198-007-0513-y
Saidenberg-Kermanac’h N, Semerano L, Nunes H et al (2014) Bone fragility in sarcoidosis and relationships with calcium metabolism disorders: a cross sectional study on 142 patients. Arthritis Res Ther 16:R78. doi:10.1186/ar4519
Heijckmann AC, Huijberts MSP, De Vries J et al (2007) Bone turnover and hip bone mineral density in patients with sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis 24:51–58
Bours S, de Vries F, van den Bergh JPW et al (2016) Risk of vertebral and non-vertebral fractures in patients with sarcoidosis: a population-based cohort. Osteoporos Int 27:1603–1610. doi:10.1007/s00198-015-3426-1
Andersen TF, Madsen M, Jørgensen J et al (1999) The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull 46:263–268. doi:10.1177/1759720X13491025
Mosbech J, Jorgensen J, Madsen M et al (1995) The national patient registry. Evaluation of data quality. Ugeskr Laeger 157:3741–3745
Vestergaard P, Mosekilde L (2002) Fracture risk in patients with celiac disease, Crohn’s disease, and ulcerative colitis: a nationwide follow-up study of 16,416 patients in Denmark. Am J Epidemiol 156:1–10. doi:10.1093/aje/kwf007
Nielsen GL, Sørensen HT, Zhou W et al (1997) The Pharmacoepidemiologic Prescription Database of North Jutland—a valid tool in pharmacoepidemiological research. Int J Risk Saf Med 10:203–205. doi:10.3233/JRS-1997-10309
Vestergaard P, Prieto-Alhambra D, Javaid MK, Cooper C (2013) Fractures in users of antidepressants and anxiolytics and sedatives: effects of age and dose. Osteoporos Int 24:671–680. doi:10.1007/s00198-012-2043-5
Johnell O, Kanis J (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16:S3–S7. doi:10.1007/s00198-004-1702-6
Wacholder S, McLaughlin JK, Silverman DT, Mandel JS (1992) Selection of controls in case-control studies. I. Principles. Am J Epidemiol 135:1019–1028. doi:10.1002/bdra.20388
Sverrild A, Backer V, Kyvik KO et al (2008) Heredity in sarcoidosis: a registry-based twin study. Thorax 63:894 LP–894896
Byg KE, Milman N, Hansen S (2003) Sarcoidosis in Denmark 1980–1994. A registry-based incidence study comprising 5536 patients. Sarcoidosis Vasc Diffus lung Dis 20:46–52
Khalid U, Gislason GH, Hansen PR (2014) Sarcoidosis in patients with psoriasis: a population-based cohort study. PLoS One 9:e109632
Van Staa TP, Abenhaim L, Cooper C et al (2000) The use of a large pharmacoepidemiological database to study exposure to oral corticosteroids and risk of fractures: validation of study population and results. Pharmacoepidemiol Drug Saf 9:359–366. doi:10.1002/1099-1557(200009/10)9:5<359::AID-PDS507>3.0.CO;2-E
van Staa TP, Leufkens HG, Abenhaim L et al (2000) Oral corticosteroids and fracture risk: relationship to daily and cumulative doses. Rheumatology 39:1383–1389. doi:10.1093/rheumatology/39.12.1383
Nakamura K, Saito T, Kobayashi R et al (2011) C-reactive protein predicts incident fracture in community-dwelling elderly Japanese women: the Muramatsu study. Osteoporos Int 22:2145–2150. doi:10.1007/s00198-010-1425-9
Schett G, Kiechl S, Weger S et al (2006) High-sensitivity C-reactive protein and risk of nontraumatic fractures in the Bruneck study. Arch Intern Med 166:2495–2501. doi:10.1001/archinte.166.22.2495
Vestergaard P, Olsen ML, Johnsen SP et al (2003) Corticosteroid use and risk of hip fracture: a population-based case-control study in Denmark. J Intern Med 254:486–493
Tervonen S, Karjalainen P, Valta R (1974) Bone mineral in sarcoidosis. Acta Med Scand 196:497–503
Montemurro L, Fraioli P, Rizzato G (1991) Bone loss in untreated longstanding sarcoidosis. Sarcoidosis 8:29–34
Sipahi S, Tuzun S, Ozaras R et al (2004) Bone mineral density in women with sarcoidosis. J Bone Miner Metab 22:48–52. doi:10.1007/s00774-003-0448-0
van Tuyl LHD, Boers M, Lems WF et al (2010) Survival, comorbidities and joint damage 11 years after the COBRA combination therapy trial in early rheumatoid arthritis. Ann Rheum Dis 69:807–812. doi:10.1136/ard.2009.108027
Cremers JP, Drent M, Elfferich MD et al (2013) Body composition profiling in a Dutch sarcoidosis population. Sarcoidosis Vasc Diffuse Lung Dis 30:289–299
Oei L, Campos-Obando N, Dehghan A et al (2014) Dissecting the relationship between high-sensitivity serum C-reactive protein and increased fracture risk: the Rotterdam study. Osteoporos Int 25:1247–1254. doi:10.1007/s00198-013-2578-0
Ahmadi-Abhari S, Luben RN, Wareham NJ, Khaw K-T (2013) C-reactive protein and fracture risk: European prospective investigation into Cancer Norfolk Study. Bone 56:67–72. doi:10.1016/j.bone.2013.05.009
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Oshagbemi, O.A., Driessen, J.H.M., Pieffers, A. et al. Use of systemic glucocorticoids and the risk of major osteoporotic fractures in patients with sarcoidosis. Osteoporos Int 28, 2859–2866 (2017). https://doi.org/10.1007/s00198-017-4115-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4115-z