Abstract
Summary
Patients with spinal cord deficits following new unstable osteoporotic compression fracture and surgical contraindications were considered to receive conservative treatment. Teriparatide was better than alendronate at improving bone mineral density and bone turnover parameters, as well as preventing aggravation of spinal cord compromise.
Introduction
This study compared the preventive effects of teriparatide and alendronate on aggravation of spinal cord compromise following new unstable osteoporotic vertebral compression fracture (OVCF) in patients with surgical contraindications.
Methods
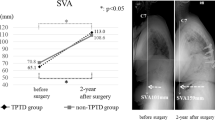
This was a 12-month, randomized, open-label study of teriparatide versus alendronate in 49 patients with new unstable OVCF and surgical contraindications. Neurological function was evaluated using modified Japanese Orthopedic Association (mJOA) score (11-point scale, the maximum score of 11 implies normalcy). Visual analog scale (VAS) scores, kyphotic angles, anterior-border heights and diameters of the spinal canal of the fractured vertebrae, any incident of new OVCFs (onset of OVCF during follow-up), spine bone mineral density (BMD), and serum markers of bone resorption and bone formation were also examined at baseline and 1, 3, 6, and 12 months after initiation of the medication regimen.
Results
At 12 months, mean mJOA score had improved in the teriparatide group and decreased in the alendronate group. Mean concentrations of bone formation and bone resorption biomarkers, mean spine BMD, and mean anterior-border height and spinal canal diameter of the fractured vertebrae were significantly greater in the teriparatide group than in the alendronate group. Mean VAS score, mean kyphotic angle of the fractured vertebrae, and incidence of new OVCFs were significantly smaller in the teriparatide group than in the alendronate group.
Conclusions
In patients with neurological deficits following new unstable OVCF and with surgical contraindications, teriparatide was better than alendronate at improving the BMD and the bone turnover parameters, as well as preventing aggravation of spinal cord compromise.

Similar content being viewed by others
References
Johnell O, Kanis J (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16(Suppl 2):S3–7
Lee HM, Park SY, Lee SH, Suh SW, Hong JY (2012) Comparative analysis of clinical outcomes in patients with osteoporotic vertebral compression fractures (OVCFs): conservative treatment versus balloon kyphoplasty. Spine J 12:998–1005
Kim DH, Vaccaro AR (2006) Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J 6:479–487
Patil S, Rawall S, Singh D, Mohan K, Nagad P, Shial B, Pawar U, Nene A (2013) Surgical patterns in osteoporotic vertebral compression fractures. Eur Spine J 22:883–891
Gao C, Wei D, Yang H, Chen T, Yang L (2015) Nanotechnology for treating osteoporotic vertebral fractures. Int J Nanomedicine 10:5139–5157
Kim HJ, Yi JM, Cho HG, Chang BS, Lee CK, Kim JH, Yeom JS (2014) Comparative study of the treatment outcomes of osteoporotic compression fractures without neurologic injury using a rigid brace, a soft brace, and no brace: a prospective randomized controlled non-inferiority trial. J Bone & Joint Surg 96:1959–1966
Farahmand P, Marin F, Hawkins F et al (2013) Early changes in biochemical markers of bone formation during teriparatide therapy correlate with improvements in vertebral strength in men with glucocorticoid-induced osteoporosis. Osteoporos Int 24:2971–2981
Keaveny TM, Donley DW, Hoffmann PF, Mitlak BH, Glass EV, San Martin JA (2007) Effects of teriparatide and alendronate on vertebral strength as assessed by finite element modeling of QCT scans in women with osteoporosis. J Bone and Min Res 22:149–157
Park JH, Kang KC, Shin DE, Koh YG, Son JS, Kim BH (2014) Preventive effects of conservative treatment with short-term teriparatide on the progression of vertebral body collapse after osteoporotic vertebral compression fracture. Osteoporos Int 25:613–618
Sudo H, Ito M, Kaneda K, Abumi K, Kotani Y, Nagahama K, Minami A, Iwasaki N (2013) Anterior decompression and strut graft versus posterior decompression and pedicle screw fixation with vertebroplasty for osteoporotic thoracolumbar vertebral collapse with neurologic deficits. Spine J 13:1726–1732
Guglielmi G, Andreula C, Muto M, Gilula LA (2005) Percutaneous vertebroplasty: indications, contraindications, technique, and complications. Acta Radiol 46:256–268
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Desai SK, Vadivelu S, Patel AJ, Brayton A, Jea A (2013) Isolated cervical spinal canal stenosis at C-1 in the pediatric population and in Williams syndrome. J Neurosurg Spine 18:558–563
Fujiwara A, Kobayashi N, Saiki K, Kitagawa T, Tamai K, Saotome K (2003) Association of the Japanese orthopaedic association score with the oswestry disability index, roland-morris disability questionnaire, and short-form 36. Spine 28:1601–1607
Sudo H, Ito M, Abumi K, Kotani Y, Takahata M, Hojo Y, Minami A (2010) One-stage posterior instrumentation surgery for the treatment of osteoporotic vertebral collapse with neurological deficits. Eur Spine J 19:907–915
Aizawa T, Sato T, Sasaki H, Kusakabe T, Morozumi N, Kokubun S (2006) Thoracic myelopathy caused by ossification of the ligamentum flavum: clinical features and surgical results in the Japanese population. J Neurosurg Spine 5:514–519
Yonenobu K, Ebara S, Fujiwara K, Yamashita K, Ono K, Yamamoto T, Harada N, Ogino H, Ojima S (1987) Thoracic myelopathy secondary to ossification of the spinal ligament. J Neurosurg 66:511–518
SCOTT PJ, Huskisson E (1977) Measurement of functional capacity with visual analogue scales. Rheumatology 16:257–259
Ammann P, Rizzoli R (2003) Bone strength and its determinants. Osteoporos Int 14(Suppl 3):S13–18
Roberto Izzoa GG, Giuseppe Guglielmib, Mario Mutoa (2013) Biomechanics of the spine. Part I: Spinal stability. Eur J Radiol 82
Roberto Izzoa GG, Giuseppe Guglielmib, Mario Mutoa (2013) Biomechanics of the spine. Part II: Spinal instability. Eur J Radiol 82:12
Tu PH, Liu ZH, Lee ST, Chen JF (2012) Treatment of repeated and multiple new-onset osteoporotic vertebral compression fractures with teriparatide. J Clin Neurosci 19:532–535
Ataka H, Tanno T, Yamazaki M (2009) Posterior instrumented fusion without neural decompression for incomplete neurological deficits following vertebral collapse in the osteoporotic thoracolumbar spine. Eur Spine J 18:69–76
Kashii M, Yamazaki R, Yamashita T et al (2013) Surgical treatment for osteoporotic vertebral collapse with neurological deficits: retrospective comparative study of three procedures--anterior surgery versus posterior spinal shorting osteotomy versus posterior spinal fusion using vertebroplasty. Eur Spine J 22:1633–1642
Nevitt MC, Chen P, Dore RK, Reginster J-Y, Kiel DP, Zanchetta JR, Glass EV, Krege JH (2006) Reduced risk of back pain following teriparatide treatment: a meta-analysis. Osteoporos Int 17:273–280
Nakamura T, Sugimoto T, Nakano T, Kishimoto H, Ito M, Fukunaga M, Hagino H, Sone T, Yoshikawa H, Nishizawa Y (2012) Randomized Teriparatide [human parathyroid hormone (PTH) 1–34] Once-Weekly Efficacy Research (TOWER) trial for examining the reduction in new vertebral fractures in subjects with primary osteoporosis and high fracture risk. J Clin Endocrinol & Metab 97:3097–3106
Acknowledgments
This work has been supported by the National Science Foundation of China 81471403 and 30973024. Ruoyan Xue contributed equally with the first author Ying Zhao in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Zhao, Y., Xue, R., Shi, N. et al. Aggravation of spinal cord compromise following new osteoporotic vertebral compression fracture prevented by teriparatide in patients with surgical contraindications. Osteoporos Int 27, 3309–3317 (2016). https://doi.org/10.1007/s00198-016-3651-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3651-2