Abstract
Summary
We studied the ranking of osteoporosis (OP) medication attributes in a convenience sample of four different racial/ethnic groups in the United States. Our study showed that postmenopausal women differ in the ranking of OP medication attributes based on age, educational level, income, and prior fracture history.
Introduction
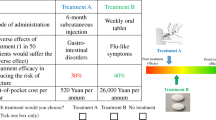
Decision making about OP medication-related behavior relies heavily on patient preferences about specific medication attributes. Patients may decide to initiate, change, or stop therapies based on ranking of perceived attributes of the therapy and their personal attitudes toward those attributes. We used MaxDiff, a form of conjoint analysis (Ryan and Farrar 2000), to explore patient weighting of attributes across four racial/ethnic groups at two sites in the United States and defined four critical attributes that influence such decisions (safety, efficacy, cost, and convenience) from qualitative interviews.
Methods
We recruited a sample of 367 Postmenopausal (PM) women at risk of OP fractures from four racial/ethnic groups: Caucasian (n = 100), African American (n = 100), Asian American (n = 82), and Hispanic American (n = 85). Respondents completed a laptop-based questionnaire that included demographic items, several short scales on medical care preference and OP patient perceptions, and a MaxDiff procedure that determines comparative ranking of attributes either as least important or most important to their decisions.
Results
MaxDiff analyses were done to evaluate the relative weight of specific statements for each participant and to determine whether racial/ethnic groups differed across dimensions. Overall, participants in all four groups rated efficacy > safety > cost > convenience.
Conclusions
Although there were no significant differences among the racial/ethnic groups on overall ranking of attributes, subgroup analyses revealed significant impact of age, education, income, and prior fracture on these decisions. The findings from this study suggest that postmenopausal women differ in their ranking of OP medication attributes, and healthcare providers must account for personal preferences in their communication about and selection of OP medications.
Similar content being viewed by others
References
Fraenkel L, Gulanski B, Wittink D (2006) Patient treatment preferences for osteoporosis. Arthritis Rheum 55(5):729–735
Fraenkel L, Gulanski B, Wittink D (2007) Patient willingness to take teriparatide. Patient Educ Couns 65(2):237–244
Barry MJ (2011) Helping patients make better personal decisions: the promise of patient centered health outcomes research. JAMA 306:1258–1259
O’Connor AM, Bennett CL, Stacey D, et al. (2009) Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews 3:CD 001431
de Bekker-Grob E, Essink-Bot M, Meerding W, Koes B, Steyerberg E (2009) Preferences of GPs and patients for preventive osteoporosis drug treatment: a discrete-choice experiment. PharmacoEconomics 27(3):211–219
Lee S, Glendenning P, Inderjeeth C (2011) Efficacy, side effects and route of administration are more important than frequency of dosing of anti-osteoporosis treatments in determining patient adherence: a critical review of published articles from 1970 to 2009. Osteoporos Int 22(3):741–753
Constantinescu F, Goucher S, Weinstein A, Fraenkel L (2009) Racial disparities in treatment preferences for rheumatoid arthritis. Med Care 47(3):350–355
Constantinescu F, Goucher S, Weinstein A, Smith W, Fraenkel L (2009) Understanding why rheumatoid arthritis patient treatment preferences differ by race. Arthritis Rheum 61(4):413–418
Piette J, Heisler M, Harand A, Juip M (2010) Beliefs about prescription medications among patients with diabetes: variation across racial groups and influences on cost-related medication underuse. J Health Care Poor Underserved 21(1):349–361
Qato D, Lindau S, Conti R, Schumm L, Alexander G (2010) Racial and ethnic disparities in cardiovascular medication use among older adults in the United States. Pharmacoepidemiol Drug Saf 19(8):834–842
Fraenkel L, Constantinescu F, Oberto-Medina M, Wittink DR (2005) Women’s preferences for prevention of bone loss. J Rheumatol 32(6):1086–1092
Darbà J, Restovic G, Kaskens L, Balbona MA, Carbonell A, Cavero P, Jordana M, Prieto C, Molina A, Padró I (2011) Patient preferences for osteoporosis in Spain: a discrete choice experiment. Osteoporos Int 22(6):1947–1954
Marshall D, Bridges J, Johnson F et al (2010) Conjoint analysis applications in health—how are studies being designed and reported?: an update on current practice in the published literature between 2005 and 2008. Patient 3(4):249–256
Ryan M, McIntosh E, Shackley P (1998) Using conjoint analysis to assess consumer preferences in primary care: an application to the patient health card. Heal Expect 1:11729
Orme B (2009) Getting started with conjoint analysis: strategies for product design and pricing research. Second edition. Research Pub Lic, Madison
Ryan M, Farrar S (2000) Using conjoint analysis to elicit preferences for health care. Br Med J 320(1):1530–1533
Cadarette SM, Gignac MAM, Jaglal SB et al (2009) Measuring patient perceptions about osteoporosis pharmacotherapy. BMC Res Notes 2:133
Ganther JM, Wiederholt JB, Kreling DH (2001) Measuring patients’ medical care preferences: care seeking versus self-treating. Med Dec Making 21(2):133–140
Gelman A, Carlin JB, Stern HS, Rubin DB (2003) Hierarchical models. In: Part II: fundamentals for Bayesian data analysis: Bayesian data analysis. Chapman and Hall/CRC, Boca Raton
Acknowledgments
These data were presented at the 2011 Annual Scientific Meeting of the American Society for Bone and Mineral Research (abstract submitted: 4/11/2011; abstract accepted: 6/10/2011; presented on 9/17/2011). Support for this study was provided by Novartis Pharmaceuticals, Hanover, NJ, USA. We acknowledge the following individuals for their valuable roles in the conduct of this study: Joe Curry and Tai Nguyen for their formulation of the MaxDiff and its statistical analyses (Sawtooth, Inc.), Jim Mirocha for statistical analysis, and Amy Mofield (Duke) and Michael Silver (OMC) who participated in data collection.
Conflicts of interest
Stuart L. Silverman is a member of the advisory board of Lilly, Amgen and a consultant of Pfizer, Lilly, Amgen, and Roche. Silverman has also received research grants from Lilly, Amgen, Medtronics, Novartis, Pfizer, and Alliance for Better Bone Health. Deborah T. Gold is a member of the advisory board and a consultant of Lilly, Amgen. Gold has also received research grants from Novartis. Andrew Calderon, Kristina Kaw, Trenita Childers, Bethany Stafford, Wendy Brynildsen, Augusto Focil, and Michael Koenig have no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Silverman, S., Calderon, A., Kaw, K. et al. Patient weighting of osteoporosis medication attributes across racial and ethnic groups: a study of osteoporosis medication preferences using conjoint analysis. Osteoporos Int 24, 2067–2077 (2013). https://doi.org/10.1007/s00198-012-2241-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-012-2241-1