Abstract
Summary
This study investigated the effects of a single administration of teriparatide on bone turnover markers in postmenopausal women. Teriparatide caused a transient increase in bone resorption and inhibition of bone formation followed by a subsequent increase in bone formation and a decrease in resorption that lasted at least 1 week.
Introduction
This study aims to investigate the effects of a single subcutaneous administration of teriparatide on bone turnover markers to elucidate why once weekly intermittent administration of teriparatide is effective on osteoporosis.
Methods
Pharmacokinetics and calcium metabolism and bone turnover parameters were measured in 30 postmenopausal women after two doses of teriparatide (28.2 or 56.5 μg injection) or placebo in a randomized, double-blind, placebo-controlled study.
Results
Teriparatide plasma concentration increased in a dose-dependent manner, and the maximum concentration was achieved 1 h after injection. Serum levels of calcium and phosphorus were transiently increased and decreased after teriparatide injection, respectively. Calcium metabolism returned to baseline levels 24 h later. Two days after injection, the serum level of 1,25-dihydroxy vitamin D was increased by ~80 % from baseline for both doses of teriparatide. Serum levels of osteocalcin and procollagen type I N-terminal propeptide decreased during the first 24 h followed by a ~10 % increase for 14 days. The serum level of cross-linked N-telopeptide (NTX) of type I collagen increased during the first 24 h followed by a 10 to 12 % dose-dependent suppression from baseline for 14 days. Urinary cross-linked C-telopeptide of type I collagen changes occurred in the same direction as serum NTX, but not dose dependently.
Conclusion
A single administration of teriparatide caused an immediate, transient increase in bone resorption and inhibited bone formation followed by an increase in bone formation and decrease in resorption for ≥1 week. These findings may provide proof for the effect of a once-weekly regimen of teriparatide on bone turnover.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Teriparatide is the synthetic form of human parathyroid hormone (PTH) 1-34 and has been widely used for the treatment of osteoporosis with high risk of fracture as daily [1–3] and weekly subcutaneous injections [4]. It has been shown that continuous and intermittent administrations of teriparatide have different metabolic effects on bone. Continuous administration of PTH or teriparatide induced an increase in bone resorption and a decrease in bone strength, which resembles the pathophysiology of primary hyperparathyroidism [5, 6]. Intermittent administration of teriparatide induced large increases in bone formation followed by increased bone resorption. The early increase in bone formation markers [procollagen type I N-terminal propeptide (P1NP) or proco1lagen type I C-terminal propeptide (P1CP)] after daily PTH or teriparatide injection has been reported to associate with increases in spine or hip bone mineral density (BMD) after treatment for 1 or 1.5 years [7, 8]. Therefore, early increases in bone formation markers seem to be important for increased BMD after PTH or teriparatide treatments. Although the differences in the changes between bone resorption and formation continued at least for 1 year, measurements in subsequent years showed that these two metabolic processes were equally stimulated [9]. Femoral neck BMD was increased by 3 to 4 % during a median of 19-month treatment with daily teriparatide [2]. The increase was sustained in subjects receiving bisphosphonate after cessation of teriparatide and rapidly decreased in subjects who received no subsequent treatment for osteoporosis [10]. It is possible that the rapid decrease in BMD once drug treatment was stopped may be due to a predisposed increase in bone resorption. Over a decade ago, Fujita et al. [11] reported that weekly administration of teriparatide for 48 weeks increased lumbar BMD by 0.6, 3.6, and 8.1 % with injection doses of 14.1, 28.2, and 56.5 μg, respectively. The maximum teriparatide dose (56.5 μg injection) in a weekly injection was approximately three times that of a daily administration of teriparatide (20 μg injection). However, the total amount per week of teriparatide in the daily injection schedule was ~2.5 times higher than the weekly injection. Therefore, neither the dose of each injection nor the total amount of dose received in the weekly regimen is likely to explain the effects on BMD and anti-fracture efficacy. In this context, we have attempted to investigate the effects of a single injection of teriparatide on bone turnover markers, calcium metabolism, pharmacokinetics (PK), and safety in postmenopausal women.
Methods
Study subjects
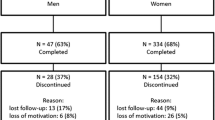
This was a single-center, randomized, double-blind, placebo-controlled study. Postmenopausal Japanese women between the ages of 60 and 79 years were eligible. The inclusion criteria included postmenopausal women without concomitant allergic diathesis, secondary osteoporosis, past histories of extensive abdominal surgery, calcium abnormalities, drug use which may affect bone metabolism, or bone fractures within 12 weeks prior to the study.
Study drug
Teriparatide and the placebo, both of which were identical in appearance, were supplied by Asahi Kasei Pharma Corporation.
Study design
Eligible women were randomized before receiving a single subcutaneous injection of placebo or teriparatide (28.2 or 56.5 μg). On the first day of administration (day 1), baseline (0 h) examinations were performed at 0800 h. Teriparatide or placebo was administered immediately after collection of baseline blood and urine samples. Blood samples were collected at 15, 30, 45, 60, 90, 120, 180, 240, 360, and 720 min after the injection. Urine samples were collected 120, 240, 360, and 720 min after the injection on day 1. Subsequent blood and urine samples were collected at 0800 h on day 2 and in the morning on days 4, 6, 8, 11, 13, and 15.
Outcomes measures
PK, safety, and changes in calcium metabolism and bone turnover markers were measured. Teriparatide acetate plasma concentrations were measured at Daiichi Pure Chemicals Co., Ltd. (Tokyo, Japan) using a rat PTH immunoradiometric assay (IRMA) kit (Immutopics, Inc., San Clemente, CA, USA) with a range of 10 to 1,000 pg/mL. Measurement of the markers of calcium metabolism [serum calcium (Ca), inorganic phosphorus (P), and urinary excretion of Ca and P] was performed at Mitsubishi Chemical Medience Co. (Tokyo, Japan). Serum-corrected Ca was calculated by the value of serum albumin [12]. Serum levels of intact PTH were measured by an electrochemiluminescence immunoassay (Roche Diagnostics K.K., Tokyo, Japan). 1,25-Dihydroxy vitamin D (1,25(OH)2D) was measured by a radio receptor assay (TFB Inc., Tokyo, Japan), and 25-hydroxy vitamin D (25(OH)D) was measured by a competitive protein-binding assay (Mitsubishi Chemical Medience); the inter-assay coefficient of variation (CV) was 11.3–13.2 and 3.7–9.9 %, respectively. Serum levels of the bone turnover markers osteocalcin and P1NP (both bone formation markers) were measured by BGP-IRMA (Mitsubishi Chemical Medience, Tokyo, Japan) and bone radioimmunoassay (Orion Diagnostic, Espoo, Finland), respectively (inter-assay CV, 4.7–7.6 and 2.7–5.0 %, respectively). Serum cross-linked N-telopeptide of type I collagen (NTX, Osteomark, Inverness Medical Innovations Inc, Waltham, MA, USA) was measured by ELISA, and urinary cross-linked C-telopeptide of type I collagen (CTX, Fujirebio Inc., Tokyo, Japan) was measured by ELISA; both are bone resorption markers (inter-assay CV, 6.9–11.1 and 2.4–9.0 %, respectively). All samples from each participant were measured in a single batch. Adverse events (AEs) occurring after teriparatide injection were collected.
Data and statistical analysis
Teriparatide plasma concentration was expressed as mean ± SD. PK analyses were performed on women who received active drug treatment by calculating the time course of plasma drug concentration and several PK parameters (Cmax, AUClast, AUCinf, Tmax, and T1/2). The calcium metabolic markers and bone turnover markers were expressed as the mean absolute values or mean percent changes from baseline. The corresponding mean placebo values were subtracted from the percent changes in order to eliminate the diurnal and daily variations of the markers. AEs (e.g., symptoms and abnormal changes in laboratory values) were summarized after coding and classified according to system organ class and preferred term using MedDRA/J (version 9.0). Statistical analysis using Dunnett’s test was performed to examine the differences between the placebo and the two teriparatide groups.
Ethical considerations
The protocol of the present study was approved by the Ethical Committee of the Medical Corporation Shinanokai Shinanozaka Clinic. Written informed consent was obtained from all participants prior to their participation in the study.
Results
Subjects
Thirty subjects (ten per group) were randomized into the three treatment groups (placebo, 28.2 μg or 56.5 μg teriparatide). There were no dropouts during the study period. The subject characteristics of the three groups were well balanced at baseline, and there were no significant differences between the groups (Table 1). The serum level of 25(OH)D in the 28.2 μg dose group seemed to be lower than that in the other groups. However, none of the groups had a level less than 10 ng/mL, suggesting that vitamin D deficiency at baseline was not included.
Pharmacokinetics
The time course and the change in plasma teriparatide acetate concentrations are shown in Fig. 1. The plasma concentration of teriparatide increased in a dose-dependent manner, and Cmax was achieved 1 h after the injection (193.12 ± 35.30 and 338.14 ± 134.18 pg/mL and 28.2 and 56.5 μg groups, respectively). The remaining PK parameter data were AUClast 25.84 ± 3.18 and 49.91 ± 11.33 ng/min/mL, AUCinf 28.07 ± 2.47 and 52.73 ± 10.03 ng/min/mL, Tmax 54.0 ± 10.5 and 52.5 ± 10.6 min, and T1/2 69.57 ± 13.04 and 77.69 ± 35.22 min, in the 28.2 and 56.5 μg groups, respectively.
Changes in calcium metabolism
Serum-corrected Ca increased rapidly and reached its peak value 4 to 6 h after the injection, returning to baseline after 24 h (Fig. 2a). The maximum mean corrected serum Ca level was 9.58 mg/dL in the 56.5 μg group, and the changes were within the normal serum Ca range. None of the samples obtained after injection were outside the normal range of serum Ca, and the changes were not dose-dependent. Urinary Ca excretion was transiently decreased 4 h after teriparatide administration and returned to the baseline level within 24 h (Fig. 2b). Serum P decreased rapidly and reached its lowest value 2 to 6 h after injection, and urinary excretion of P increased rapidly after injection (Fig. 2c, d). The serum levels of intact PTH were decreased during the first 24 h after administration and returned to baseline at day 6 (Fig. 3a, b). Serum levels of 1,25(OH)2D after teriparatide injection were increased for 2 days before returning to baseline (Fig. 3c, d). There was no obvious dose-dependent difference in Ca regulation changes after the teriparatide injection. The median values at baseline and the distribution at follow-up are indicated in Table 2.
Mean change of (a) serum corrected calcium (in milligrams per deciliter), (b) urinary calcium (in milligrams per gram Cr), (c) serum phosphate (in milligrams per deciliter), and (d) urinary phosphate (in milligrams per gram Cr) through 72 h after a single subcutaneous injection of teriparatide (filled circle 56.5 μg, filled triangle 28.2 μg) or placebo (empty square). Significant differences between the teriparatide (number sign 56.5 μg, asterisk 28.2 μg) and placebo groups (p < 0.05)
Mean percent change of serum intact PTH (a, b) and 1,25(OH)2D (c, d) through 15 days after a single subcutaneous injection of teriparatide (filled circle 56.5 μg, filled triangle 28.2 μg) or placebo (empty square). Delta intact PTH (b) and Δ 1,25(OH)2D (d) were adjusted by the corresponding placebo value (formulation, each measurement − mean placebo value). Significant differences between the teriparatide (number sign 56.5 μg, asterisk 28.2 μg) and placebo groups (p < 0.05)
Changes in bone formation markers
Percent change from baseline and percent changes subtracted by the corresponding placebo values were calculated for serum P1NP and osteocalcin. In the placebo group, serum levels of P1NP and osteocalcin were increased after injection followed by a gradual decrease to ~15 % below baseline (Fig. 4a–d). These changes in bone formation markers were considered to be due to circadian variations. After adjustment for circadian variations, serum levels of P1NP in the teriparatide-treated groups were decreased shortly after the injection (−15 %) followed by a continuous increase to ~15 % (Fig. 4d). The increase in P1NP was maintained for 14 days after the injection. There were no remarkable dose-related differences in P1NP changes. Serum osteocalcin levels followed a similar trend including a dose-dependent response. However, the late-phase increase was not as obvious (+10 %).
Mean percent change of serum P1NP (a, b) and osteocalcin (c, d) through 15 days after a single subcutaneous injection of teriparatide (filled circle 56.5 μg, filled triangle 28.2 μg) or placebo (empty square). Delta serum P1NP (b) and Δ serum osteocalcin (d) were adjusted by the corresponding placebo value (formulation, each measurement − mean placebo value). Significant differences between the teriparatide (number sign 56.5 μg, asterisk 28.2 μg) and placebo groups (p < 0.05). P1NP procollagen type I N-terminal propeptide
Changes in bone resorption markers
The same technique to nullify the effects of circadian rhythm was used to analyze serum NTX and urinary CTX levels. Both serum NTX and urinary CTX levels were increased transiently on day 1 followed by a 10 % decline from baseline (Fig. 5a–d). This decline persisted during the 14 days of observation, and the urinary NTX levels decreased in a dose-dependent manner.
Mean percent change of serum NTX (a) and urinary CTX (b) through 15 days after a single injection of teriparatide (filled circle 56.5 μg, filled triangle 28.2 μg) and placebo (empty square). Delta serum NTX (b) and Δ urinary CTX (d) were adjusted by the corresponding placebo value (formulation, each measurement − placebo value). Significant differences between the teriparatide (number sign 56.5 μg, asterisk 28.2 μg) and placebo groups (p < 0.05). NTX cross-linked N-telopeptide of type I collagen, CTX cross-linked C-telopeptide of type I collagen
Safety outcomes
AEs occurred in 5 out of 10 subjects in the placebo group and in all 10 subjects in each of the 28.2 and 56.5 μg teriparatide groups (Table 3). AEs in two of the placebo subjects and in all of the teriparatide subjects were classified as adverse drug reactions (ADRs). ADRs observed in two or more subjects treated with teriparatide were erythema at injection site, somnolence, headache, and hot flashes. More women in the 28.2 and 56.5 μg groups experienced ADRs than their placebo-group counterparts, but most of these ADRs were mild and resolved without intervention. Moreover, there were no significant differences between the 28.2 and 56.5 μg groups in the incidence or extent of ADRs. There were also no significant changes in laboratory values before or after administration throughout the study duration.
Conclusions
The present study aimed to investigate the effects of a single administration of teriparatide on calcium metabolism and bone turnover markers for 2 weeks following administration. Long-term changes in bone turnover markers with daily teriparatide administration have been well documented. Daily administration yields initial increases in bone formation markers followed by increased bone resorption markers [9]. This time difference in the responses of bone turnover markers in daily teriparatide injection has been referred to as an “anabolic window” [9]. The anabolic window was presented as the reason that daily teriparatide injection increased BMD. However, the late-phase increase in bone resorption markers may rapidly decrease BMD after teriparatide injections are stopped [13]. Although the daily administration of teriparatide showed clinical benefits including fracture prevention [2] and improvement of patients’ quality of life [14], the daily self-administered regimen is bothersome, especially for elderly patients. Fujita et al. reported that once-weekly administration of teriparatide effectively increased BMD in postmenopausal osteoporosis patients [11], and Nakamura et al. reported a significant risk reduction for fracture [4]. However, there had been no available data to demonstrate why once-weekly administration of teriparatide effectively increases BMD.
PK analysis in the present study revealed that the teriparatide concentration peaked after 1 h and disappeared 6 h after a single injection. To respond to the rapid rise in teriparatide, serum calcium and urinary phosphate excretion transiently increased. Increases in the serum level of 1,25(OH)2D in response to teriparatide injection were observed. These changes in calcium metabolism were within our expectation, and the findings indicated that a single injection of teriparatide is biologically active in terms of calcium metabolism. Cosman et al. reported that daily 20 μg teriparatide injections increased 1,25(OH)2D levels with a peak effect occurring at 1 month and a persistent increase over 1 year [15]; a similar result was seen with weekly 56.5 μg teriparatide therapy [11].
The response of bone turnover markers to a single administration of teriparatide had not previously been investigated. The present study indicated that a single administration of teriparatide caused biphasic changes in bone formation and resorption markers, namely, a rapid increase in resorption markers and decrease in formation markers for 1 or 2 days, followed by a sustained suppression of resorption markers and stimulation of formation markers for the subsequent 2 to 14 days. These bone marker changes did not show dose dependency except for serum NTX, and the magnitude of change in bone markers was smaller than the changes seen with daily administration of teriparatide [16]. The sustained late-phase response of bone turnover markers in the present study may be one possible explanation for the BMD increase seen with weekly administration of teriparatide.
The present study includes several limitations. First, most of the changes in calcium metabolic and bone turnover markers after a single administration of teriparatide did not show dose-related differences. However, the previous study indicated that once-weekly administration of teriparatide increased BMD in a dose-dependent manner [11]. Therefore, the changes in calcium metabolic and bone turnover markers may explain limited parts of the effect of teriparatide on bone. Furthermore, the magnitude of the changes in the bone turnover markers was not enough to assess quantitatively; we were only able to assess them qualitatively.
Although the present study included the limitations mentioned above, the results indicate that a single administration of teriparatide may have a sustained effect (14 days) in terms of the changes in bone turnover markers. However, it is still not clear as to whether or not repeated weekly administration of teriparatide induces a more powerful reduction of bone resorption and stimulation of bone formation. Therefore, further research will be required.
We concluded that a single administration of teriparatide caused an immediate, transient increase in bone resorption and inhibition of bone formation followed by a subsequent increase in bone formation and decrease in resorption for at least 1 week. These findings may provide substantial proof for the effect of a once-weekly regimen of teriparatide on bone turnover.
References
Reeve J, Meunier PJ, Parsons JA, Bernat M, Bijvoet OL, Courpron P, Edouard C, Klenerman L, Neer RM, Renier JC, Slovik D, Vismans FJ, Potts JT Jr (1980) Anabolic effect of human parathyroid hormone fragment on trabecular bone in involutional osteoporosis: a multicentre trial. Br Med J 7(280):1340–1344
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, Wang O, Mitlak BH (2001) Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 10(344):1434–1441
Hodsman AB, Bauer DC, Dempster DW, Dian L, Hanley DA, Harris ST, Kendler DL, McClung MR, Miller PD, Olszynski WP, Orwoll E, Yuen CK (2005) Parathyroid hormone and teriparatide for the treatment of osteoporosis: a review of the evidence and suggested guidelines for its use. Endocr Rev 26:688–703
Nakamura T, Sugimoto T, Nakano T, Kishimoto H, Ito M, Fukunaga M, Hagino H, Sone T, Yoshikawa H, Nishizawa Y, Fujita T, Shiraki M (2012) Randomized Teriparatide [Human Parathyroid Hormone (PTH) 1-34] Once-Weekly Efficacy Research (TOWER) trial for examining the reduction in new vertebral fractures in subjects with primary osteoporosis and high fracture risk. J Clin Endocrinol Metab 97:3097–3106
Tam CS, Heersche JN, Murray TM, Parsons JA (1982) Parathyroid hormone stimulates the bone apposition rate independently of its resorptive action: differential effects of intermittent and continuous administration. Endocrinology 110:506–512
Uzawa T, Hori M, Ejiri S, Ozawa H (1995) Comparison of the effects of intermittent and continuous administration of human parathyroid hormone (1-34) on rat bone. Bone 16:477–484
Bauer DC, Garnero P, Bilezikian JP, Greenspan SL, Ensrud KE, Rosen CJ, Palermo L, Black DM (2006) Short-term changes in bone turnover markers and bone mineral density response to parathyroid hormone in postmenopausal women with osteoporosis. J Clin Endocrinol Metab 91:1370–1375
Chen P, Satterwhite JH, Licata AA, Lewiecki EM, Sipos AA, Misurski DM, Wagman RB (2005) Early changes in biochemical markers of bone formation predict BMD response to teriparatide in postmenopausal women with osteoporosis. J Bone Miner Res 20:962–970
Girotra M, Rubin MR, Bilezikian JP (2006) The use of parathyroid hormone in the treatment of osteoporosis. Rev Endocr Metab Disord 7:113–121
Prince R, Sipos A, Hossain A, Syversen U, Ish-Shalom S, Marcinowska E, Halse J, Lindsay R, Dalsky GP, Mitlak BH (2005) Sustained nonvertebral fragility fracture risk reduction after discontinuation of teriparatide treatment. J Bone Miner Res 20:1507–1513
Fujita T, Inoue T, Morii H, Morita R, Norimatsu H, Orimo H, Takahashi HE, Yamamoto K, Fukunaga M (1999) Effect of an intermittent weekly dose of human parathyroid hormone (1-34) on osteoporosis: a randomized double-masked prospective study using three dose levels. Osteoporosis Int 9:296–306
Payne RB, Little AJ, Williams RB, Milner JR (1973) Interpretation of serum calcium in patients with abnormal serum proteins. Br Med J 4:643–646
Leder BZ, Neer RM, Wyland JJ, Lee HW, Burnett-Bowie SM, Finkelstein JS (2009) Effects of teriparatide treatment and discontinuation in postmenopausal women and eugonadal men with osteoporosis. J Clin Endocrinol Metab 94:2915–2921
Crans GG, Silverman SL, Genant HK, Glass EV, Krege JH (2004) Association of severe vertebral fractures with reduced quality of life: reduction in the incidence of severe vertebral fractures by teriparatide. Arthritis Rheumatism 50:4028–4034
Cosman F, Dawson-Hughes B, Wan X, Krege JH (2012) Changes in vitamin D metabolites during teriparatide treatment. Bone 50:1368–1371
Glover SJ, Eastell R, McCloskey EV, Rogers A, Garnero P, Lowery J, Belleli R, Wright TM, John MR (2009) Rapid and robust response of biochemical markers of bone formation to teriparatide therapy. Bone 45:1053–1058
Acknowledgments
This study was performed with funding support from Asahi Kasei Pharma Corporation; the test drugs were also supplied by this company.
Conflicts of interest
MS has received consulting fees from the pharmaceutical companies, Asahi Kasei Pharma, Dai-ichi Sankyo, Chugai, and Teijin Pharma. TS has received research grants and consulting fees from the pharmaceutical companies, Asahi Kasei and Dai-ichi Sankyo. TN has received research grants and/or consulting fees from the pharmaceutical companies, Chugai, Teijin, Asahi Kasei, and Dai-ichi Sankyo. TN is a councilor for hospital administration and social medical insurance with the Japan Ministry of Health, Welfare, and Labour.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Shiraki, M., Sugimoto, T. & Nakamura, T. Effects of a single injection of teriparatide on bone turnover markers in postmenopausal women. Osteoporos Int 24, 219–226 (2013). https://doi.org/10.1007/s00198-012-2159-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-012-2159-7