Abstract
Summary
The extent to which fracture protection and safety varies with increasing time on teriparatide [rhPTH(1-34)] therapy is a clinically relevant unanswered question. In postmenopausal women with osteoporosis, increased duration of teriparatide versus placebo treatment was associated with a progressive decrease in the rates of nonvertebral fragility fractures and back pain.
Introduction
The impact of duration of teriparatide [rhPTH(1-34)] therapy on patient outcomes is a relevant unanswered question.
Methods
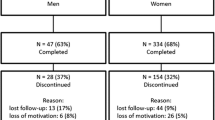
Postmenopausal women with osteoporosis were randomized to once-daily subcutaneous injection with placebo (N = 544), teriparatide 20 µg (TPTD20; N = 541), or teriparatide 40 µg (TPTD40; N = 552) plus calcium and vitamin D supplementation. The time to first nonvertebral fragility fracture and new or worsening back pain following treatment initiation was analyzed using Cox partial likelihood regression treating time on therapy as a linear, time-dependent covariate.
Results
Compared with placebo, the relative hazard for nonvertebral fragility fractures decreased by 7.3% for each additional month of TPTD20 [hazard ratio = 0.927, 95% CI (0.876 to 0.982), p = 0.009] and by 7.6% for each additional month of TPTD40 [hazard ratio = 0.924, 95% CI (0.871 to 0.981), p = 0.009]. Clinical vertebral fractures appeared to increase over time in the placebo group and occurred primarily in the first time interval in the teriparatide treatment groups. Compared with placebo, the relative hazard of back pain was decreased by 8.3% for each additional month of TPTD20 [hazard ratio = 0.920, 95% CI (0.902 to 0.939), p < 0.001] and 8.7% for each additional month of TPTD40 [hazard ratio = 0.917, 95% CI (0.898 to 0.935), p < 0.001].
Conclusions
These findings suggest increased nonvertebral fracture protection, reduced back pain, and reduced occurrence of side effects with longer duration of teriparatide therapy.


Similar content being viewed by others
References
Lindsay R, Nieves J, Formica C et al (1997) Randomised controlled study of effect of parathyroid hormone on vertebral-bone mass and fracture incidence among postmenopausal women on oestrogen with osteoporosis. Lancet 350:550–555
Finkelstein JS, Hayes A, Hunzelman JL et al (2003) The effects of parathyroid hormone, alendronate, or both in men with osteoporosis. N Engl J Med 249:1216–1226
Neer RM, Arnaud CD, Zanchetta JR et al (2001) Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344:1434–1441
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Cox DR, Oakes D (2001) Analysis of survival data. Chapman and Hall, London, England
Caro JJ, Ishak KJ, Huybrechts KF et al (2004) The impact of compliance with osteoporosis therapy on fracture rates in actual practice. Osteoporos Int 15(12):1003–1008
Ma YL, Zeng Q, Donley DW et al (2006) Teriparatide increases bone formation in modeling and remodeling osteons and enhances IGF-II immunoreactivity in postmenopausal women with osteoporosis. J Bone Miner Res 21(6):855–864
Jiang Y, Zhao JJ, Mitlak BH et al (2003) Teriparatide [recombinant human parathyroid hormone (1–34)] improves both cortical and cancellous bone structure. J Bone Miner Res 18:1932–1941
Dempster DW, Cosman F, Kurland ES et al (2001) Effects of daily treatment with parathyroid hormone on bone microarchitecture and turnover in patients with osteoporosis: a paired biopsy study. J Bone Miner Res 16:1846–1853
Reeve J, Meunier PJ, Parsons JA et al (1980) Anabolic effect of human parathyroid hormone fragment on trabecular bone in involutional osteoporosis: a multicentre trial. BMJ 280:1340–1344
Bradbeer JN, Arlot ME, Meunier PJ et al (1992) Treatment of osteoporosis with parathyroid peptide (hPTH 1–34) and oestrogen: increase in volumetric density of iliac cancellous bone may depend on reduced trabecular spacing as well as increased thickness of packets of newly formed bone. Clin Endocrinol 37:282–289
Hodsman AB, Steer BM (1993) Early histomorphometric changes in response to parathyroid hormone therapy in osteoporosis: evidence for de novo bone formation on quiescent cancellous surfaces. Bone 14:523–527
Dempster DW, Zhou H, Cosman F et al (2001) PTH treatment directly stimulates bone formation in cancellous and cortical bone in humans. J Bone Miner Res 16(Suppl 1):S179
Genant HK, Halse J, Briney WG et al (2005) The effects of teriparatide on the incidence of back pain in postmenopausal women with osteoporosis. Curr Med Res Opin 21(7):1027–1034
Nevitt MC, Chen P, Dore RK et al (2006) Reduced risk of back pain following teriparatide treatment: a meta-analysis. Osteoporos Int 17(2):273–280
Nevitt MC, Chen P, Kiel DP et al (2006) Reduction in the risk of developing back pain persists at least 30 months after discontinuation of teriparatide treatment: a meta-analysis. Osteoporos Int 17(11):1630–1637
Lindsay R, Scheele WH, Neer RM et al (2004) Sustained vertebral fracture risk reduction after withdrawal of teriparatide in postmenopausal women with osteoporosis. Arch Intern Med 164(18):2024–2030
Acknowledgements
The authors are grateful for the assistance of Melinda Rance, BS, in the preparation of the figures, and Jahangir Alam, MS, and Kathryn Engstrom, BS, for assistance with programming the statistical analyses. We thank Jingyuan Wang, PhD, and Erik F. Eriksen, DMSc, MD, for contributions to the design of the study and critical review of earlier drafts of the manuscript. This work was sponsored by Lilly Research laboratories, Eli Lilly and Company, Indianapolis, Indiana, USA.
Conflicts of interest
Funding was provided by Eli Lilly and Company. Drs. Pohl, Glass, Chen and Krege are employees of Eli Lilly and Company.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lindsay, R., Miller, P., Pohl, G. et al. Relationship between duration of teriparatide therapy and clinical outcomes in postmenopausal women with osteoporosis. Osteoporos Int 20, 943–948 (2009). https://doi.org/10.1007/s00198-008-0766-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0766-0