Abstract.
Skeletal assessment by morphometry at peripheral sites (e.g. metacarpal index), although simple to perform and widely available, was limited by poor precision and technical aspects of radiogrammetry. Digital X-ray radiogrammetry (DXR) uses the principles of this long-established method but applies more sophisticated methodology to overcome these problems. The aims of this study were to (a) investigate the effects of radiographic technique on bone mineral density (BMD) measurement by DXR, (b) compare DXR to dual-energy X-ray absorptiometry (DXA) and single-energy X-ray absorptiometry (SXA) and (c) determine the applicability of DXR in identifying individuals who most appropriately might be referred for axial DXA. Different radiographers performing the radiograph do not adversely affect precision. Precision, unstandardised (CV%) and standardised (sCV%), is good with both double (DF)- and single (SF)-sided emulsion radiographic film, but better with SF (CV% 0.92 vs 1.12 DF; SCV% 1.76 vs 2.93 DF). Repeat analysis precision was determined on SF (CV% 0.24, sCV% 0.55). A significant (p<0.001), systematic difference was found between BMD measured from DF and SF (mean difference 0.017 g/cm2). The overall percentage difference between the methods was 2.98% (range 0.18–5.78%). Correlations between DXR BMD and DXA were moderately good (r=0.56–0.77, p<0.001); with SXA of the forearm they were excellent (r=0.91, p<0.001). The sensitivity and specificity of DXR for detecting women with osteopaenia or osteoporosis (DXA T-score less than −1; World Health Organisation) was determined at the spine [area under curve (AUC)=0.82, standard error (SE)=0.04], femoral neck (AUC=0.84, SE=0.04) and total hip (AUC=0.84, SE=0.04). Based on femoral neck BMD for detection of osteopaenia, a DXR T-score threshold of −1.05 would be appropriate for detection of patients who might benefit most from axial DXA measurements. The DXR is quick and simple to use, having potential for application in a variety of settings as analysis can be performed in a central unit, with radiographs taken in sites over a wide geographical area. Retrospective analysis may also be performed, e.g. on radiographs taken to monitor rheumatoid arthritis. The technique may also provide a simple, widely available and relatively inexpensive method to assess patients at risk of osteopaenia or osteoporosis, and who most appropriately could be referred for axial DXA. This may be particularly relevant in those who suffer low-trauma fractures and attend accident and emergency or fracture clinics, where investigation for osteoporosis is often overlooked.


Similar content being viewed by others
References
Barnett E, Nordin B (1960) The radiological diagnosis of osteoporosis. Clin Radiol 11:166–174
Meema H (1962) The occurrence of cortical bone atrophy in old age and osteoporosis. J Can Assoc Radiol 13:27–32
Meema H, Meema S (1963) Measurable roentgenologic changes in some peripheral bones in senile osteoporosis. J Am Geriatr Soc 11:1170–1182
Garn S, Poznanski A, Nagy J (1971) Bone measurement in the differential diagnosis of osteopenia and osteoporosis. Radiology 100:509–518
Exton-Smith A, Millard P, Payne P, Wheeler E (1969) Method of measuring quantity of bone. Lancet 2:1153–1157
Ashby R, Ward K, Mughal M, Adams J (2002) Age related changes in metacarpal morphometry and areal bone mineral density in children assessed by digital X-ray radiogrammetry (DXR). J Bone Miner Res 17:S297
Adams P, Davies G,Sweetnam P (1969) Observer error and measurements of the metacarpal. Br J Radiol 42:192–197
Tovey F Radiographic morphometry and photodensitometry. In: Metabolic bone disease
Dequeker J (1976) Quantitative radiology: radiogrammetry of cortical bone. Br J Radiol 49:912–920
Saville PD, Heaney RP, Recker RR (1976) Radiogrammetry at four bone sites in normal middle-aged women: their relation to each other, to calcium metabolism and to other biological variables. Clin Orthop Relat Res 307–315
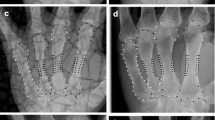
Cootes T, Hill A, Taylor C, Haslam J (1994) The use of active shape models for locating structures in medical images. Image Vision Comput 6:276–285
Cootes T, Taylor C, Cooper D, Graham J (1995) Active shape models: their training and application. Comput Vision Image Understanding 1:38–59
Derisquebourg T, Dubois P, Devogelaer J et al. (1994) Automated computerized radiogrammetry of the second metacarpal and its correlation with absorptiometry of the forearm and spine. Calcif Tiss Int 54:461–465
Kalla A, Meyers O, Parkyn N, Kotze T (1989) Osteoporosis screening-radiogrammetry revisited. Br J Rheumatol 28:511–517
Jorgensen J, Andersen P, Rosholm A, Bjarnason N (2000) Digital X-ray radiogrammetry: a new appendicular bone densitometric method with high precision. Clin Physiol 20:330–335
Hyldstrup L, Jorgensen J, Sorenson T, Baeksgaard L (2001) Response of cortical bone to antiresorptive treatment. Calcif Tiss Int 68:135–139
European Communities/ European Foundation for Osteoporosis (1998) Building strong bones and preventing fractures. Summary report on osteoporosis in the European Community-Action for Prevention, Germany, pp 3–12
National Osteoporosis Society (2001) Position statement on the use of peripheral X-ray absorptiometry in the management of osteoporosis, pp 1–15
Miller PD, Njeh CF, Jankowski LG, Lenchik L (2002) What are the standards by which bone mass measurement at peripheral skeletal sites should be used in the diagnosis of osteoporosis? J Clin Densitom 5 (Suppl): S39–S45
World Health Organization (1994) Assessment of fracture risk and its implication to screening for postmenopausal osteoporosis, WHO, Geneva
Okkalides D, Fotakis M (1994) Patient effective dose resulting from radiographic examinations. Br J Radiol 67:564–672
Black D, Palermo L, Sorenson J et al. (2001) A normative reference database study for Pronosco X-posure System. J Clin Densitom 4:5–12
Pacheco E, Harrison E, Ward K, Lunt M, Adams J (2002) Detection of osteoporosis by dual energy X-ray absorptiometry (DXA) of the calcaneus: Is the WHO criterion applicable? Calcif Tiss Int 70:475–482
Gluer C, Blake G, Lu Y et al. (1995) Accurate assessment of precision errors: how to measure the reproducibility of bone densitometry techniques. Osteoporos Int 5:262–270
Miller C, Herd R, Ramalingam T, Fogelman I, Blake G (1993) Ultrasonic velocity measurements through the calcaneus: Which velocity should be measured? Osteoporos Int 3:31–35
Bland J, Altman D (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 307–310
Altman D (1999) Practical statistics for medical research. Chapman and Hall/CRC, London
Rosholm A (2002) X-posure system. Manchester
Faulkner R, Stetten E von, Miller P (1999) Discordance in patient classification using T-scores. J Clin Densitom 2:343–350
Kanis JA, Gluer C (2000) An update in the diagnosis and assessment of osteoporosis with densitometry. Osteoporos Int 11:192–202
Miller P (2000) Controversies in bone mineral density diagnostic classification. Calcif Tiss Int 66:317–319
Bouxsein M, Palermo L, Yeung C, Black D (2002) Digital X-ray radiogrammetry predicts hip, wrist and vertebral fracture risk in elderly women: a prospective analysis from the study of osteoporotic fractures. Osteoporos Int 13:358–365
Vasireddy S, Haigh C, Reaney L et al. (2002) Digital X-ray radiogrammetry indices, particularly MCI, can predict vertebral fracture risk in osteoporotic women. J Bone Miner Res 17:S186
Haigh C, Reaney L, Adams J et al. (2002) Digital X-ray radiogrammetry indices are sensitive to clodronate treatment in women with osteoporosis. J Bone Miner Res 17:S231
Acknowledgements. The authors thank M. Hodgkinson, D. Legerton, B. Booth and E. Bate for performing the radiographs.We also thank Lanmark, Buckinghamshire and Sectra Pronosco A/S, Denmark, for the loan of the Pronosco X-Posure Version 1 system and for advice and technical support throughout the study. We thank M. Lunt for assistance with standardisation between the two DXA machines.
Author information
Authors and Affiliations
Corresponding author
Appendix: Standardisation of BMD
Appendix: Standardisation of BMD
The BMD measurements were measured on both the Hologic QDR 4500 (n=154) and the Lunar DPX-L (n=50). In order to combine the BMD measurements and T-scores from these machines, standardisation was necessary. The European Spine Phantom [1] is scanned daily in our department. Twenty measurements were taken over the time period of this study and used to produce standardisation equations for conversion of lumbar spine (L2–L4) and femoral neck BMD:
where y is the measured density, x is the standardised density, and α and β are parameters unique to each machine [2]. Solving the equation for x enables measured values to be converted to standardised values. For our scanners, the standardisation equations are:
and
where y h and y l are the densities measured on the Hologic and Lunar machines, respectively.
Recalculation of T-scores
To combine T-scores from both machines, the standardised BMD is converted back into one of the manufacturer's units using the inverse of the above equations. In this study the standardised Lunar data was recalculated into Hologic data using the following equation:
The BMD was then converted to T-scores (NHANES III) using an equation provided by T. Kelly (Hologic Inc., Pers. commun.):
and
Appendix references
The following are references for the Appendix:
-
1.
Kalender W, Felsenberg D, Genant H et al. (1995) European Spine Phantom: a tool for standardization and quality control in spinal bone mineral measurements by DXA and QCT. Eur J Radiol 20:83–92
-
2.
Pearson J, Dequeker J, Henley M et al. (1995) European semi-anthropomorphic spine phantom for the calibration of bone densitometers: assessment of precision, stability and accuracy. Osteoporos Int 2:174–184
Rights and permissions
About this article
Cite this article
Ward, K.A., Cotton, J. & Adams, J.E. A technical and clinical evaluation of digital X-ray radiogrammetry. Osteoporos Int 14, 389–395 (2003). https://doi.org/10.1007/s00198-003-1386-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-003-1386-3