Abstract
Introduction and hypothesis
The objective was to examine the effect of the surgical removal of vaginally placed prolapse and incontinence mesh on sexual function. We hypothesize that patients with painful complications of mesh will experience improvement in dyspareunia and sexual function after mesh removal.
Methods
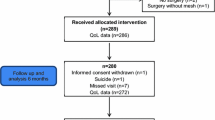
The eligible cohort consisted of 133 women who presented with a new onset of pain attributed to mesh-augmented incontinence or prolapse surgery and who elected to undergo mesh removal between 1 August 2012 and 1 July 2013. Sexual function symptoms were assessed before and after mesh removal surgery using the Pelvic Organ Prolapse and Urinary Incontinence Sexual Function Questionnaire short form (PISQ-12). Multivariate analysis was performed to identify predictors of improvement in dyspareunia.
Results
Ninety-four patients undergoing mesh removal completed a pre-operative questionnaire, 63 of whom also completed a post-operative questionnaire. After mesh removal, there was a nearly 50% reduction in the proportion of women reporting always experiencing post-operative pain with intercourse among those experiencing pre-operative pain. There was a statistically significant quantitative improvement in pain with intercourse after mesh removal based on mean change score of PISQ-12 question 5 “How often do you experience pain with intercourse?”. In multivariate analysis, only history of vaginal delivery was associated with symptom improvement.
Conclusion
Removal of transvaginal prolapse mesh is associated with improvement in self-reported dyspareunia based on a standardized question on a validated instrument in a small cohort of women. Although larger studies are needed to confirm the relationship between mesh-augmented surgeries and post-procedural dyspareunia, these data suggest that consideration of mesh removal is a reasonable step for patients with painful intercourse attributed to mesh-augmented prolapse and incontinence surgeries.

Similar content being viewed by others
Abbreviations
- FDA:
-
Federal Drug Administration
- LUTS:
-
Lower urinary tract symptoms
- PISQ-12:
-
Prolapse and Urinary Incontinence Sexual Function Questionnaire short form
- POP:
-
Pelvic organ prolapse
- TVM:
-
Transvaginal mesh
- UCLA:
-
University of California, Los Angeles
- UTIs:
-
Urinary tract infections
References
Wu JM, Vaughan CP, Goode PS, et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol. 2014;123:141–8. https://doi.org/10.1097/AOG.0000000000000057.
Handa VL, Garrett E, Hendrix S, Gold E, Robbins J. Progression and remission of pelvic organ prolapse: a longitudinal study of menopausal women. Am J Obstet Gynecol. 2004;190:27–32. https://doi.org/10.1016/j.ajog.2003.07.017.
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501–6. https://doi.org/10.1016/S0029-7844(97)00058-6.
Khan AA, Eilber KS, Clemens JQ, Wu N, Pashos CL, Ange JT. Trends in management of pelvic organ prolapse among female Medicare beneficiaries. Am J Obstet Gynecol. 2015;212(463):e461–8. https://doi.org/10.1016/j.ajog.2014.10.025.
Opinion no. 513: vaginal placement of synthetic mesh for pelvic organ prolapse. Obstet Gynecol. 2011;118:1459–64. https://doi.org/10.1097/AOG.0b013e31823ed1d9.
Skala CE, Renezeder K, Albrich S, et al. Mesh complications following prolapse surgery: management and outcome. Eur J Obstet Gynecol Reprod Biol. 2011;159:453–6. https://doi.org/10.1016/j.ejogrb.2011.07.024.
Baessler K, Hewson AD, Tunn R, Schuessler B, Maher CF. Severe mesh complications following intravaginal slingplasty. Obstet Gynecol. 2005;106:713–6. https://doi.org/10.1097/01.AOG.0000177970.52037.0a.
Falagas ME, Velakoulis S, Iavazzo C, Athanasiou S. Mesh-related infections after pelvic organ prolapse repair surgery. Eur J Obstet Gynecol Reprod Biol. 2007;134:147–56. https://doi.org/10.1016/j.ejogrb.2007.02.024.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2016;2:CD012079. https://doi.org/10.1002/14651858.CD012079.
US Food and Drug Administration, authors. Urogynecologic surgical mesh: update on the safety and effectiveness of transvaginal placement for pelvic organ prolapse. 2011. www.fda.gov/downloads/MedicalDevices/Safety/AlertsandNotices/UCM262760.pdf. Accessed 25 May 2014.
US Food and Drug Administration, authors. Urogynecologic surgical mesh: update on the safety and effectiveness of transvaginal placement for pelvic organ prolapse. 2019. www.fda.gov/downloads/MedicalDevices/Safety/AlertsandNotices/UCM262760.pdf. Accessed 3 Sept 2020.
Withagen MI, Vierhout ME, Hendriks JC, Kluivers KB, Milani AL. Risk factors for exposure, pain, and dyspareunia after tension-free vaginal mesh procedure. Obstet Gynecol. 2011;118:629–36. https://doi.org/10.1097/AOG.0b013e31822ada95.
De Tayrac R, Devoldere G, Renaudie J, et al. Prolapse repair by vaginal route using a new protected low-weight polypropylene mesh: 1-year functional and anatomical outcome in a prospective multicentre study. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:251–6. https://doi.org/10.1007/s00192-006-0135-5.
Milani R, Salvatore S, Soligo M, Pifarotti P, Meschia M, Cortese M. Functional and anatomical outcome of anterior and posterior vaginal prolapse repair with prolene mesh. BJOG. 2005;112:107–11. https://doi.org/10.1111/j.1471-0528.2004.00332.x.
Altman D, Falconer C. Perioperative morbidity using transvaginal mesh in pelvic organ prolapse repair. Obstet Gynecol. 2007;109:303–8. https://doi.org/10.1097/01.AOG.0000250970.23128.63.
Rogo-Gupta L, Grisales T, Huynh L, Rodriguez LV, Raz S. Symptom improvement after prolapse and incontinence graft removal in a case series of 306 patients. Female Pelvic Med Reconstr Surg. 2015;21:319–24. https://doi.org/10.1097/SPV.0000000000000191.
Kasyan G, Abramyan K, Popov AA, Gvozdev M, Pushkar D. Mesh-related and intraoperative complications of pelvic organ prolapse repair. Cent European J Urol. 2014;67:296–301. https://doi.org/10.5173/ceju.2014.03.art17.
Tijdink MM, Vierhout ME, Heesakkers JP, Withagen MI. Surgical management of mesh-related complications after prior pelvic floor reconstructive surgery with mesh. Int Urogynecol J. 2011;22:1395–404. https://doi.org/10.1007/s00192-011-1476-2.
Ridgeway B, Walters MD, Paraiso MFR, et al. Early experience with mesh excision for adverse outcomes after transvaginal mesh placement using prolapse kits. Am J Obstet Gynecol. 2008;199:703.e1–7. https://doi.org/10.1016/j.ajog.2008.07.055.
Warembourg S, Labaki M, de Tayrac R, Costa P, Fatton B. Reoperations for mesh-related complications after pelvic organ prolapse repair: 8-year experience at a tertiary referral center. Int Urogynecol J. 2017;28:1139–51. https://doi.org/10.1007/s00192-016-3256-5.
Crosby EC, Abernethy M, Berger MB, DeLancey JO, Fenner DE, Morgan DM. Symptom resolution after operative management of complications from transvaginal mesh. Obstet Gynecol. 2014;123: 134–9. https://doi.org/10.1097/AOG.0000000000000042.
Lee D, Dillon B, Lemack G, Gomelsky A, Zimmern P. Transvaginal mesh kits—how "serious" are the complications and are they reversible? Urology. 2013;81:43–8. https://doi.org/10.1016/j.urology.2012.07.098.
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:164–8; discussion 168. https://doi.org/10.1007/s00192-003-1063-2.
Fan Y, Huang Z, Yu D. Incontinence-specific quality of life measures used in trials of sling procedures for female stress urinary incontinence: a meta-analysis. Int Urol Nephrol. 2015;47:1277–95. https://doi.org/10.1007/s11255-015-1020-2.
Zyczynski HM, Rickey L, Dyer KY, et al. Sexual activity and function in women more than 2 years after midurethral sling placement. Am J Obstet Gynecol. 2012;207(5):421.e1–6. https://doi.org/10.1016/j.ajog.2012.06.053.
Mengerink BB, Van Leijsen SAL, Vierhout ME, et al. The impact of midurethral sling surgery on sexual activity and function in women with stress urinary incontinence. J Sex Med. 2016;13:1498–507. https://doi.org/10.1016/j.jsxm.2016.08.005.
Younger A, Rac G, Clemens JQ, et al. Pelvic organ prolapse surgery in academic female pelvic medicine and reconstructive surgery urology practice in the setting of the Food and Drug Administration public health notifications. Urology. 2016;91:46–51. https://doi.org/10.1016/j.urology.2015.12.057.
Welk B, Al-Hothi H, Winick-Ng J. Removal or revision of vaginal mesh used for the treatment of stress urinary incontinence. JAMA Surg. 2015;150:1167–75. https://doi.org/10.1001/jamasurg.2015.2590.
Margulies RU, Lewicky-Gaupp C, Fenner DE, McGuire EJ, Clemens JQ, Delancey JOL. Complications requiring reoperation following vaginal mesh kit procedures for prolapse. Am J Obstet Gynecol. 2008;199(6):678.e1–4. https://doi.org/10.1016/j.ajog.2008.07.049.
Rogowski A, Bienkowski P, Tosiak A, Jerzak M, Mierzejewski P, Baranowski W. Mesh retraction correlates with vaginal pain and overactive bladder symptoms after anterior vaginal mesh repair. Int Urogynecol J. 2013;24:2087–92. https://doi.org/10.1007/s00192-013-2131-x.
Mamik MM, Rogers RG, Qualls CR, Morrow JD. The minimum important difference for the Pelvic Organ Prolapse-Urinary Incontinence Sexual Function Questionnaire. Int Urogynecol J. 2014;25(10):1321–6. https://doi.org/10.1007/s00192-014-2342-9.
Author information
Authors and Affiliations
Contributions
T. Grisales: project development, manuscript writing and editing, data collection, data analysis, and final approval; A.L. Ackerman: manuscript editing, data analysis and visualization, and final approval of the manuscript; L.J. Rogo-Gupta: project development, manuscript editing and final approval of the manuscript; L. Herbert: data analysis and visualization; S. Raz: project development and final approval of the manuscript; L.V. Rodriguez: project development, manuscript editing, and final approval of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
A.L. Ackerman is consultant for Watershed Medical and Cynosure. The remaining authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
192_2021_4923_MOESM1_ESM.tif
Dyspareunia after mesh removal. a For all patients who underwent mesh removal, post-operative pain varied by the amount of pre-operative dyspareunia. Almost half of patients complaining usually or always of dyspareunia pre-operatively exhibited substantial improvement, with no subjects worsening after surgery. For patients with less frequent pre-operative dyspareunia, most were unchanged, with only one subject exhibiting worsening pain. b Among the 51 patients reporting always or usually experiencing dyspareunia pre-operatively, the relative improvement is indicated by the post-operative scores on Pelvic Organ Prolapse and Urinary Incontinence Sexual Function Questionnaire short form 12 question 5 (TIF 1.41 mb)
Rights and permissions
About this article
Cite this article
Grisales, T., Ackerman, A.L., Rogo-Gupta, L.J. et al. Improvement in dyspareunia after vaginal mesh removal measured by a validated questionnaire. Int Urogynecol J 32, 2937–2946 (2021). https://doi.org/10.1007/s00192-021-04923-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04923-7