Abstract
Introduction and hypothesis
Pelvic floor muscle training (PFMT) improves urinary incontinence and mild pelvic organ prolapse (POP). We aimed to investigate the effect of preoperative PFMT on urinary and colorectal-anal distress and related quality of life (QoL) in women with severe POP scheduled for surgery.
Methods
Randomized controlled trial of 159 women scheduled for POP surgery (intervention = 81, controls = 78). Intervention consisted of daily PFMT from inclusion to the day of surgery. Symptoms and QoL were assessed at inclusion, day of surgery and 6 months postoperatively using the Urinary Distress Inventory (UDI-6), Colorectal-Anal Distress Inventory (CRADI-8), Urinary Impact Questionnaire (UIQ) and Colorectal-Anal Impact Questionnaire (CRAIQ) (range 0–100). Mixed model statistical analyses were used.
Results
One hundred fifty-one (95%) women completed the study (intervention = 75, controls = 76). Mean waiting times until surgery and follow-up were 22 and 28 weeks. There was no difference in mean postoperative symptom and QoL scores (95% CI) between the intervention and control group: UDI-6 16 (12–21) vs. 17 (13–22), CRADI-8 15 (11–18) vs. 13 (10–16), UIQ 11 (7–15) vs. 10 (6–13) and CRAIQ 5 (2–7) vs. 6 (4–9), all p > 0.05. Overall mean scores were reduced from baseline to postoperative follow-up: UDI-6 37 (33–41) vs. 17 (14–20), CRADI-8 22 (19–25) vs. 14 (11–16); UIQ 28 (24–32) vs. 10 (7–13) and CRAIQ 16 (12–19) vs. 5 (3–7), all p < 0.01.
Conclusions
We found no added effect of preoperative PFMT on symptoms or QoL related to urinary and colorectal-anal distress in women scheduled for POP surgery. They achieved symptomatic improvement postoperatively regardless of PFMT.
Clinical trial registration
The study was registered in clinicaltrials.gov: NCT 03,064,750.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary and colorectal-anal distress has a negative impact on quality of life [1,2,3]. These symptoms are highly prevalent in women with pelvic organ prolapse (POP) because of shared risk factors such as age, parity and pelvic floor trauma occurring during delivery [1,2,3,4,5]. Injury to nerves, connective tissue and muscles contributes to the pathophysiology of pelvic floor disorders [1, 6]. Strengthening the pelvic floor muscles is therefore one option to treat pelvic floor disorders [7].
Intensive pelvic floor muscle training (PFMT) is effective in treating stress urinary incontinence and symptomatic mild POP, reducing bulge sensation and frequent urination [8, 9]. PFMT is also effective in treating anal incontinence symptoms and improve quality of life, but the effect on other urinary symptoms or colorectal-anal symptoms such as emptying difficulties is unclear [9,10,11,12,13]. Repeated contractions improve the strength and endurance of the pelvic floor muscles, providing better support to pelvic organs and improving urinary continence [9, 12]. However, most studies have either examined women in the immediate postpartum period or women with isolated stress urinary incontinence [10, 12]. Other studies of women undergoing POP surgery have mainly focused on the effect of peri- or postoperative PFMT on urinary and colorectal-anal symptoms, and one study found marginal effects of PFMT on quality of life [14,15,16,17]. Previous studies with < 100 participants have included women scheduled for surgery because of different conditions (POP, urinary incontinence and hysterectomy for other reasons), and it is unclear whether the positive effect of peri- and postoperative PFMT was found in women with POP [15, 16, 18]. Any additional effect of preoperative PFMT on urinary and colorectal-anal symptoms and quality of life in women with advanced POP has not been thoroughly investigated.
Our aim was therefore to examine the effect of preoperative PFMT on urinary and colorectal-anal symptoms in women scheduled for POP surgery. We also aimed to study any effect on quality of life related to these symptoms.
Materials and methods
This was a randomized controlled trial (RCT) of women scheduled for POP surgery at Trondheim University Hospital, Norway, from January 2017 through March 2019. Women were recruited from the outpatient urogynecological clinic from January 2017 through June 2018. All participants signed a written informed consent form at a preoperative consultation. Inclusion criteria were indication for POP surgery (bulge sensation and POP stage ≥ 2), age > 18 years and fluent in Norwegian or English. Women declining participation, needing immediate surgery or with cognitive impairments were excluded. The study was approved by the Regional Committee for Medical and Health Research Ethics (REK2015/1751/midt) and registered in clinicaltrials.gov with the identifier NCT 03,064,750.
Age, parity, delivery mode, height, weight, smoking habits, menopausal status, hormonal therapy, pessary use and any previous PFMT or POP surgery were registered at inclusion. Surgical procedure was determined according to the clinical practice considering age, prolapse grade, involved compartments and any previous POP surgery. Available procedures were: colporrhaphy (anterior and posterior), perineoplasty, enterocele correction, cervical amputation with shortening of the ligaments, vaginal hysterectomy, sacrospinous ligament fixation, laparoscopic robot-assisted sacrouteropexy or sacrocolpopexy. The procedures performed and any surgical complications were registered.
At inclusion, women were randomized to intervention or control with the allocation ratio of 1:1 and stratified using POP stage > or < 3 and age > or < 60 years using a web-based randomization tool (WebRAND). Participants were examined and patient-reported outcomes collected at inclusion, day of surgery (minimum 3 months later) and 6 months postoperatively by one of three authors (SM/MØN/IV). Data were registered in a web-based case report form (WebCRF) provided by the Unit of Applied Clinical Research, Norwegian University of Science and Technology. A gynecological examination was performed with the participant in the supine position with hips and knees semi-flexed and abducted. POP was assessed at maximum Valsalva according to the Pelvic Organ Prolapse Quantification (POP-Q) system [19]. Examiners were not blinded to background data or group allocation at examination. At each visit the women answered a validated Norwegian translation of the Pelvic Floor Distress Inventory (PFDI-20) and Pelvic Floor Impact Questionnaire (PFIQ-7) [20, 21]. For quantification of urinary and colorectal-anal distress and impact on quality of life, we used the PFDI-20 sub-scales: Urinary Distress Inventory (UDI-6) and Colorectal Anal Distress Inventory (CRADI-8) and PFIQ-7 subscales: Urinary Impact Questionnaire (UIQ) and Colorectal Anal Impact Questionnaire (CRAIQ), all with a range of 0–100 where 100 is the worst bother [20, 21]. The average waiting time to surgery at Trondheim University Hospital during the study period was 3 months. Waiting time was not influenced by group allocation.
Women allocated to intervention received written information regarding the correct pelvic floor exercise technique at inclusion. They were given written lifestyle advice regarding diet and proper emptying of the bladder and bowel as well as instructions on contraction of the pelvic floor muscles when sneezing, coughing or laughing [7, 9]. Vaginal examination was performed by one of the examiners (SM, MØN, IV) at inclusion and by a pelvic floor physiotherapist at visits 2 and 6 weeks after inclusion to ensure proper contraction for women in the intervention group. Women were instructed to perform intensive pelvic floor muscle exercise with 8–12 maximal contractions holding at least 6–8 s three times daily from time of inclusion until the day of surgery [22, 23]. They were informed about voluntary weekly group training sessions at the baseline examination and at the first consultation with the physiotherapist 2 weeks after inclusion. They were required to record daily exercises in a training diary, to be handed in at the day of surgery. Women who failed to deliver a training diary were interviewed by telephone regarding the number of days per week they had performed training and the number of repetitions each day. A ≥ 70% completion of daily exercise rate was defined as adherence to the protocol [24, 25]. Women in the control group received no intervention in the waiting time for surgery. All postmenopausal women, regardless of randomization, received local estrogen therapy unless contraindicated.
Primary outcome measures of the RCT were pelvic floor muscle strength assessed by palpation and ultrasound and symptoms of pelvic floor disorders as registered in clinicaltrials.gov (NCT 03,064,750). We have previously reported results regarding muscle contraction assessed by palpation, manometry and ultrasound as well as prolapse symptoms [25]. In the present article, we report on another of the primary outcomes: symptoms of urinary and colorectal-anal distress assessed by validated PFDI sub-scales: UDI-6 and CRADI-8. A secondary outcome was patient reported quality of life related to urinary and colorectal-anal symptoms using the PFIQ sub-scales: UIQ and CRAIQ.
Sample size calculation was based on differences in pelvic floor muscle contraction. A mean modified Oxford scale of 2.6 ± 1.3 was anticipated and a clinically relevant change in modified Oxford scale at 6-month follow-up of 3.2 ± 1.3. With power 80%, p = 0.05 and sampling ratio 1:1, a study sample of 74 women in each group was considered sufficient.
Statistical methods
Outcomes were analyzed following an intention-to-treat principle. We used IBM SPSS Statistics version 25 (SPSS Inc., Chicago, IL) and R version 3.6.3 (R Project for Statistical Computing) to perform statistical analyses. The level of statistical significance was set at 5%. Normality of the continuous variables (UDI-6, CRADI-8, UIQ and CRAIQ) was assessed using histograms and QQ plots. Independent sample t-test was used to examine any differences between women accepting and declining randomization. Symptoms and quality of life in the intervention group versus the control group at the day of surgery and postoperative control were evaluated with mixed models analysis with a five-level combined variable for time and group status as fixed effects (baseline for total study population, day of surgery for intervention group, day of surgery for control group, postoperative follow-up intervention group and postoperative follow-up control group). The model was fitted by restricted maximum likelihood estimation and unstructured covariance for the repeated measurements of each participant. The effect of the stratification variables (POP stage > or < 3 and age > or < 60) was tested, and no effect was found. The change in the total study population with time as fixed effect (baseline for total study population, postoperative follow-up for total population) was also tested using a mixed models analysis fitted by restricted maximum likelihood estimation and unstructured covariance for the repeated measurements.
Results
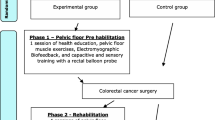
During the recruitment period from January 2017 through June 2018, 272 women were referred for POP surgery. One hundred thirteen women were excluded because they refused participation, did not fulfill the inclusion criteria or declined randomization; see the flow chart (Fig. 1). Of the 159 randomized women, 151 (95%) completed the study, 75 in the intervention group and 76 in the control group. Data collection ended in June 2019.
Flowchart of study population. ¶Declined participation (n = 36), missed for recruitment (n = 4), did not meet eligibility criteria (n = 32). *Three women postponed surgery (one because of other medical conditions and two because of symptomatic improvement). Three women declined further participation. §Two women postponed surgery because of improvement of symptoms
Background characteristics and outcome variables are outlined in Table 1. Overall, 92/151 (61%) had POP stage ≥ 3. The proportion of women undergoing an isolated anterior or posterior compartment repair was 28/151 (19%) and 27/151 (18%), respectively. Thirty-eight (25%) women had an isolated central compartment repair. A combination of procedures involving more than one compartment was performed in 58/151 (38%) women. Sixty (80%) women in the training group achieved an adherence level of ≥ 70% to the intervention. None of the participants met for the voluntary weekly group training sessions. Women declining randomization were similar to study participants in POP stage ≥ 3, body mass index and parity, but significantly older compared to the study participants (67 vs. 61 years, p = 0.002).
Mean (SD) and median (range) waiting time to surgery was 22 (10) and 21(7–84) weeks, and women were examined postoperatively after mean 28 (8) and median 26 (11–79) weeks. There was no statistically significant difference in UDI-6 or CRADI-8 scores or change in scores between intervention and control groups at day of surgery or postoperatively; see Table 2. Analysis of the quality of life related to urinary and colorectal-anal distress (UIQ and CRAIQ) revealed similar findings (Table 2). Figure 2 demonstrates the linear mixed model analysis of the change in scores for the intervention and control group at each examination. Overall, there was a statistically significant decrease in symptoms and improvement in quality of life from baseline to postoperative control in the total study population (Table 3).
Figure comparing symptoms and related quality of life in the intervention group (solid line) and the control group (dashed line) from baseline to the day of surgery and the postoperative follow-up, using linear mixed models analysis. Examination time (baseline, day of surgery and postoperative follow-up) on the x-axis and mean score with 95% confidence interval on the y-axis of the a urinary distress inventory (UDI-6), b colorectal-anal distress inventory (CRADI-8), c urinary impact questionnaire (UIQ) and d colorectal-anal impact questionnaire (CRAIQ)
Two major complications were registered: an intestinovaginal fistula after laparoscopic sacrocolpopexy and one postoperative hemorrhage, both requiring further surgery. Other complications were postoperative urinary tract infection requiring treatment in 3/151 (2%) and one woman (< 1%) with persisting residual urine after 6 months.
Discussion
In this randomized controlled trial of women scheduled for POP surgery, we found no effect of preoperative PFMT on urinary or colorectal-anal distress and related quality of life 6 months after surgery. Women achieved symptomatic improvement postoperatively regardless of PFMT.
PFMT is shown to reduce stress urinary incontinence, anal incontinence and symptoms of mild POP, but there is less evidence regarding the effect of a strong and well-functioning pelvic floor on other urinary symptoms and colorectal-anal distress [8, 9, 11, 12, 17]. A systematic review on fecal incontinence in adults reported conflicting results in different studies comparing PFMT to other conservative treatments such as dietary advice, medical management and PFMT with biofeedback [11]. This review included both genders and varying treatment durations from 1 to 12 months, thus making it difficult to generalize [11]. Our results are consistent with previous studies on women with severe POP where peri- and postoperative PFMT did not alter symptoms of urinary and colorectal-anal distress [14, 15]. A recent study by Duarte et al. included a preoperative intervention period of 2 weeks and reported an overall improvement in symptoms and quality of life (using PFDI-20, PFIQ-7 and subscales) for all women scheduled for POP surgery, without clear advantage from PFMT in the intervention group, which agrees with our findings [14]. The study excluded women with previous POP surgery and covered a shorter postoperative follow-up of 90 days [14]. In contrast, 10% of the women in the current study had prior POP surgery, and they were followed 6 months to observe any durable effects. Tools used for symptom assessment differ between studies, and the intervention in the current study was exclusively preoperative whereas the intervention in most prior studies was mainly postoperative PFMT [15, 16]. McClurg et al. demonstrated a postoperative reduction of prolapse symptoms in the intervention group, but no effect on incontinence symptoms, although the participants had milder prolapses and other adjuncts such as electrical stimulation and biofeedback were also applied in addition to PFMT [16]. Incontinence and POP symptoms did not improve after PFMT alone in a study by Frawley et al., although they reported less de novo stress incontinence after PFMT [15]. However, the intervention consisted of only one supervised preoperative PFMT session followed by seven sessions over 1 year, and women scheduled for hysterectomy for other indications than POP were included [15]. A study by Jarvis et al. included women scheduled for urinary incontinence or POP surgery with 12-week follow-up and found reduced stress urinary incontinence after PFMT, but it is unclear whether the positive effect of PFMT was found only in women with isolated incontinence or also in women with POP [18].
The main clinical implication of our findings is that women scheduled for POP surgery have no additional benefit of PFMT on urinary and colorectal-anal symptoms. Women with advanced POP and complex injuries to the pelvic floor may need more supervised and intensive exercise or additional treatments such as nerve stimulation to increase strength. In a previous publication from this RCT, we found no difference in muscle strength or POP symptoms between the intervention and control groups [25]. The failure to improve pelvic floor muscle strength is a possible explanation for the lack of effect also on urinary and colorectal-anal distress. They experienced improved pelvic floor muscle contraction after surgery, which may explain the results from the present study of reduced urinary and colorectal-anal distress and improved quality of life at the postoperative follow-up [25]. With 60% of women having POP stage ≥ 3, it seems likely that advanced POP poses limitations to correct muscle contraction for sufficient clinical and subjective improvement. In addition, the large reduction in symptoms and improvement of quality of life after surgery may obscure any additional minor effect of PFMT after surgery. Latent stress urinary incontinence can appear after anterior compartment correction and may also be a reason for failing to detect any effect of PFMT on urinary distress in this cohort [26]. The etiology of urinary and colorectal-anal distress is complex and not solely dependent on weak pelvic floor muscle function [1, 4, 5, 27]. This cohort consists of women with extensive pelvic floor injuries, such as levator muscle injury, sphincter injury and nerve damage, all possibly contributing to the development and persistence of urinary or colorectal-anal symptoms [1]. Other chronic diseases and lifestyle habits also contribute to symptoms [1, 2].
The main strength of the present study was the randomized controlled design and the large study size. The intervention consisted of daily PFMT and 80% of women in the intervention group maintained ≥ 70% adherence, indicating that the training program was acceptable for most women scheduled for POP surgery. We included women with advanced POP in any compartment and those with prior POP surgery, representing a heterogenous cohort commonly encountered in urogynecological practice and further increasing the clinical relevance of this study. The intervention lasted on average 22 weeks, which should be sufficient to achieve muscle hypertrophy [8, 22, 23]. No adjunctive treatments such as biofeedback or nerve stimulation were given in order to uncover the exclusive effects of PFMT. Validated questionnaires designed for evaluating distress and quality of life related to urinary and colorectal-anal symptoms were used [20, 21]. We used mixed models statistics for assessment of symptoms over time and between the groups, making it possible to use all data available also for women with missing data at the day of surgery or postoperative follow-up.
A limitation was that we did not register the number of women with previous incontinence surgery. However, the randomization ensured similar distribution to the intervention and control group for both previous surgery and other potential confounders. Another limitation was that we did not record whether women in the control group performed PFMT, and this might dilute any possible difference between the groups. Participants were not blinded to the intervention, and therefore women in the intervention group might have scored higher on quality of life because of an expectation of improvement. Examining gynecologists were not blinded to group allocation at the day of surgery or at the postoperative follow-up, but since this study only presents patient-reported outcomes, this would not be relevant to the outcome. Women declining randomization were significantly older; hence, the results may not apply to the older segment of POP patients. No power calculation was performed for these outcome measures, but the women had symptom scores between 20–40 out of 100. Hence, with 75 and 76 women in each group we would expect to find a clinical and statistically significant difference in symptom scores after intervention if there were any effect of PFMT.
Conclusion
In women with advanced POP scheduled for surgery, we found no added effect of preoperative PFMT on symptoms or quality of life related to urinary or colorectal-anal distress 6 months after surgery. Surgical prolapse correction decreased urinary and colorectal-anal symptoms and improved quality of life related to these symptoms. There is a need for long-term trials of intensive PFMT in women after corrective POP surgery in order to investigate the comprehensive effect on urinary and colorectal-anal distress and de novo incontinence.
References
Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, Markland AD. Prevalence and trends of symptomatic pelvic floor disorders in US women. Obstet Gynecol. 2014;123(1):141–8. https://doi.org/10.1097/AOG.
Boreham MK, Richter HE, Kenton KS, Nager CW, Gregory WT, Aronson MP, Vogt VY, McIntire DD, Schaffer JI. Anal incontinence in women presenting for gynecologic care: prevalence, risk factors, and impact upon quality of life. Am J Obstet Gynecol. 2005;192(5):1637–42.
Rømmen K, Schei B, Rydning A, Sultan AH, Mørkved S. Prevalence of anal incontinence among Norwegian women: a cross-sectional study. BMJ Open. 2012;2(4):e001257.
Guzmán Rojas RA, Kamisan Atan I, Shek KL, Dietz HP. Anal sphincter trauma and anal incontinence in urogynecological patients. Ultrasound Obstet Gynecol. 2015;46(3):363–6.
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6. https://doi.org/10.1097/aog.
Delancey JO, Kane Low L, Miller JM, Patel DA, Tumbarello JA. Graphic integration of causal factors of pelvic floor disorders: an integrated life span model. Am J Obstet Gynecol. 2008;199(6):610.e611-615. https://doi.org/10.1016/j.ajog.2008.04.001.
Bo K, Frawley HC, Haylen BT, Abramov Y, Almeida FG, Berghmans B, Bortolini M, Dumoulin C, Gomes M, McClurg D, Meijlink J, Shelly E, Trabuco E, Walker C, Wells A. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Int Urogynecol J. 2017;28(2):191–213. https://doi.org/10.1007/s00192-016-3123-4.
Braekken IH, Majida M, Engh ME, Bo K. Can pelvic floor muscle training reverse pelvic organ prolapse and reduce prolapse symptoms? An assessor-blinded, randomized, controlled trial. Am J Obstet Gynecol. 2010;203(2):170.e171-177. https://doi.org/10.1016/j.ajog.2010.02.037.
Dumoulin C, Cacciari LP, Hay‐Smith EJC (2018) Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev (10):CD005654. https://doi.org/10.1002/14651858.CD005654.pub4
Sigurdardottir T, Steingrimsdottir T, Geirsson RT, Halldorsson TI, Aspelund T, Bo K. Can postpartum pelvic floor muscle training reduce urinary and anal incontinence?: an assessor-blinded randomized controlled trial. Am J Obstet Gynecol. 2019. https://doi.org/10.1016/j.ajog.2019.09.011.
Simillis C, Lal N, Pellino G, Baird D, Nikolaou S, Kontovounisios C, Smith JJ, Tekkis PP. A systematic review and network meta-analysis comparing treatments for faecal incontinence. Int J Surg. 2019;66:37–47. https://doi.org/10.1016/j.ijsu.2019.04.007.
Woodley SJ, Lawrenson P, Boyle R, Cody JD, Mørkved S, Kernohan A, Hay-Smith EJC. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev. 2020;5(5):Cd007471. https://doi.org/10.1002/14651858.CD007471.pub4.
Mazur-Bialy AI, Kołomańska-Bogucka D, Opławski M, Tim S. Physiotherapy for prevention and treatment of fecal incontinence in women—systematic review of methods. J Clin Med. 2020;9(10):3255.
Duarte TB, Bo K, Brito LGO, Bueno SM, Barcelos TM, Bonacin MA, Ferreira CH. Perioperative pelvic floor muscle training did not improve outcomes in women undergoing pelvic organ prolapse surgery: a randomised trial. J Physiother. 2020;66(1):27–32. https://doi.org/10.1016/j.jphys.2019.11.013.
Frawley HC, Phillips BA, Bø K, Galea MP. Physiotherapy as an adjunct to prolapse surgery: an assessor-blinded randomized controlled trial. Neurourol Urodyn. 2010;29(5):719–25. https://doi.org/10.1002/nau.20828.
McClurg D, Hilton P, Dolan L, Monga A, Hagen S, Frawley H, Dickinson L. Pelvic floor muscle training as an adjunct to prolapse surgery: a randomised feasibility study. Int Urogynecol J. 2014;25(7):883–91. https://doi.org/10.1007/s00192-013-2301-x.
Haya N, Feiner B, Baessler K, Christmann-Schmid C, Maher C. Perioperative interventions in pelvic organ prolapse surgery. Cochrane Database Syst Rev. 2018;8(8):Cd013105. https://doi.org/10.1002/14651858.Cd013105.
Jarvis SK, Hallam TK, Lujic S, Abbott JA, Vancaillie TG. Peri-operative physiotherapy improves outcomes for women undergoing incontinence and or prolapse surgery: results of a randomised controlled trial. Aust N Z J Obstet Gynaecol. 2005;45(4):300–3. https://doi.org/10.1111/j.1479-828X.2005.00415.x.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193(1):103–13. https://doi.org/10.1016/j.ajog.2004.12.025.
Teig CJ, Grotle M, Bond MJ, Prinsen CAC, Engh MAE, Cvancarova MS, Kjollesdal M, Martini A. Norwegian translation, and validation, of the Pelvic Floor Distress Inventory (PFDI-20) and the Pelvic Floor Impact Questionnaire (PFIQ-7). Int Urogynecol J. 2017;28(7):1005–17. https://doi.org/10.1007/s00192-016-3209-z.
Garcia-Sanchez E, Avila-Gandia V, Lopez-Roman J, Martinez-Rodriguez A, Rubio-Arias JA (2019) What pelvic floor muscle training load is optimal in minimizing urine loss in women with stress urinary incontinence? A systematic review and meta-analysis. Int J Environ Res Public Health 16 (22). https://doi.org/10.3390/ijerph16224358
Bø K, Talseth T, Holme I. Single blind, randomised controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones, and no treatment in management of genuine stress incontinence in women. BMJ. 1999;318(7182):487–93. https://doi.org/10.1136/bmj.318.7182.487.
Dumoulin C, Hay-Smith J, Frawley H, McClurg D, Alewijnse D, Bo K, Burgio K, Chen S-Y, Chiarelli P, Dean S, Hagen S, Herbert J, Mahfooza A, Mair F, Stark D, Van Kampen M. 2014 consensus statement on improving pelvic floor muscle training adherence: international continence society 2011 state-of-the-science seminar. NeurourolUrodyn. 2015;34(7):600–5. https://doi.org/10.1002/nau.22796.
Nyhus M, Mathew S, Salvesen Ø, Salvesen K, Stafne S, Volløyhaug I. The effect of preoperative pelvic floor muscle training on pelvic floor contraction, symptomatic and anatomical pelvic organ prolapse after surgery: a randomized controlled trial. Ultrasound Obstet Gynecol. 2020. https://doi.org/10.1002/uog.22007.
Davenport MT, Sokol ER, Comiter CV, Elliott CS. Does the degree of cystocele predict de novo stress urinary incontinence after prolapse repair? Further analysis of the colpopexy and urinary reduction efforts trial. Female Pelvic Med Reconstr Surg. 2018;24(4):292–4. https://doi.org/10.1097/spv.
Mathew S, Guzmán Rojas RA, Salvesen KA, Volløyhaug I. Levator ani muscle injury and risk for urinary and fecal incontinence in parous women from a normal population, a cross-sectional study. Neurourol Urodyn. 2019;38(8):2296–302. https://doi.org/10.1002/nau.24138.
Acknowledgements
We thank Nina Askimdal for coordination of clinical examinations, Berit M. Bjelkåsen at the Unit of Applied Clinical Research for technical help with the web-based database and physiotherapist Clara Karoliussen for guiding patients in pelvic floor muscle exercise. We thank our colleagues at the Trondheim University Hospital and the Norwegian University of Science and Technology for assistance and infrastructure for this study.
Funding
Open access funding provided by NTNU Norwegian University of Science and Technology (incl St. Olavs Hospital - Trondheim University Hospital). This study was funded by The Liasion Committee for Education, Research and Innovation in Central Norway (Samarbeidsorganet Helse-Midt). The funding sources were not involved in any steps of study design, data collection, analysis or interpretation or article formation.
Author information
Authors and Affiliations
Contributions
S. Mathew: Protocol/project development, study design, data collection and management, data analysis, manuscript conception and writing/editing.
MØ Nyhus: Protocol/project development, study design, data collection and management, manuscript editing.
Ø Salvesen: Protocol development, data analysis, manuscript editing.
KÅ Salvesen: Protocol/project development, study design, manuscript editing.
SN Stafne: Protocol development, manuscript editing/revising.
I Volløyhaug: Protocol/project development, study design, data collection, manuscript conception and writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mathew, S., Nyhus, M.Ø., Salvesen, Ø. et al. The effect of preoperative pelvic floor muscle training on urinary and colorectal-anal distress in women undergoing pelvic organ prolapse surgery—a randomized controlled trial. Int Urogynecol J 32, 2787–2794 (2021). https://doi.org/10.1007/s00192-021-04684-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04684-3