Abstract
Introduction and hypothesis
This study aimed to compare the expression levels of extracellular matrix (ECM) and apoptosis proteins in the uterosacral ligament (USL) of patients with and without pelvic organ prolapse (POP).
Methods
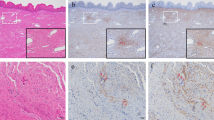
The USL were obtained from patients with POP-Q ≥ III (n = 35) and without POP (n = 20). Immunohistochemistry (IHC) staining and RT-qPCR were conducted to assess the protein and mRNA levels, respectively. The levels of type I collagen (COLI), type III collagen (COLIII), matrix metalloproteinase (MMP)1, MMP2, MMP9, tissue inhibitor of metalloproteinase (TIMP)1, TIMP2, estrogen receptor (ER)α, ERβ and apoptosis-related gene B cell lymphoma 2 (Bcl-2)-associated agonist of cell death (Bad) and Bcl-2-associated X (Bax) in the USL were analyzed.
Results
The protein expression and mRNA levels of MMP2 and MMP9, mRNA levels of BAD and BAX, and protein expression of active cleaved-Caspase3 were significantly higher in the POP group. There were no evident differences in COLIII, MMP1 or ERβ expression at either the mRNA or protein level or in TIMP1, TIMP2 or Caspase3 by IHC between the two groups. However, obvious decreases in COLI and ERα were evident at both the mRNA and protein levels in the POP group, and the mRNA levels of TIMP1 and TIMP2 were also decreased compared to those of the control group.
Conclusion
ECM in the USL tissues of POP patients is remodeled compared with non-POP patients and is characterized by decreased synthesis and increased degradation of collagen; moreover, the levels of the main proteins involved in apoptosis are increased in POP tissue.




Similar content being viewed by others
References
Alarab M, Kufaishi H, Lye S, Drutz H, Shynlova O. Expression of extracellular matrix-remodeling proteins is altered in vaginal tissue of premenopausal women with severe pelvic organ prolapse. Reprod Sci. 2014;21(6):704–15. https://doi.org/10.1177/1933719113512529.
Smith FJ, Holman CD, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096–100. https://doi.org/10.1097/AOG.0b013e3181f73729.
John OLD, Lisa KL, Janis MM, Divya AP, Julie AT. Graphic integration of causal factors of pelvic floor disorders: an integrated life span model. Am J Obstet Gynecol. 2008;199(6):610.e611–5. https://doi.org/10.1016/j.ajog.2008.04.001.
Maldonado PA, Wai CY. Pelvic organ prolapse: new concepts in pelvic floor anatomy. Obstet Gynecol Clin N Am. 2016;43(1):15–26. https://doi.org/10.1016/j.ogc.2015.10.001.
Kim T, Sridharan I, Ma Y, Zhu BF, Chi NW, Kobak W, et al. Identifying distinct nanoscopic features of native collagen fibrils towards early diagnosis of pelvic organ prolapse. Nanomed. 2016;12(3):667–75. https://doi.org/10.1016/j.nano.2015.11.006.
Kerkhof MH, Hendriks L, Brolmann HAM. Changes in connective tissue in patients with pelvic organ prolapse-a review of the current literature. Int Urogynecol J. 2009;20(4):461–74. https://doi.org/10.1007/s00192-008-0737-1.
Jackson S, James M, Abrams P. The effect of oestradiol on vaginal collagen metabolism in postmenopausal women with genuine stress incontinence. BJOG-Int J Obstet Gy. 2002;109(3):339–44. https://doi.org/10.1111/j.1471-0528.2002.01052.x.
Li HJ, Haque Z, Lu Q, Li L, Karas R, Mendelsohn M. Steroid receptor coactivator 3 is a coactivator for myocardin, the regulator of smooth muscle transcription and differentiation. Proc Natl Acad Sci U S A. 2007;104:4065–70. https://doi.org/10.1073/pnas.0611639104.
Han LY, Wang L, Wang Q, Li HL, Zang H. Association between pelvic organ prolapse and stress urinary incontinence with collagen. Exp Ther Med. 2014;7(5):1337–41. https://doi.org/10.3892/etm.2014.1563.
Zhou L, Lee JH, Wen Y, Constantinou C, Yoshinobu M, Omata S, et al. Biomechanical properties and associated collagen composition in vaginal tissue of women with pelvic organ prolapse. J Urology. 2012;188(3):875–80. https://doi.org/10.1016/j.juro.2012.05.017.
Michal D, Elad L, Jacob D, Moshe M, Ruthy SL. Increased matrix metalloproteinases-1,-9 in the uterosacral ligaments and vaginal tissue from women with pelvic organ prolapse. Eur J Obstet Gyn R B. 2011;156(1):113–7. https://doi.org/10.1016/j.ejogrb.2010.12.043.
Phillips CH, Anthony F, Benyon C, Monga AK. Collagen metabolism in the uterosacral ligaments and vaginal skin of women with uterine prolapse. BJOG-Int J Obstet Gy. 2006;113(1):39–46. https://doi.org/10.1111/j.1471-0528.2005.00773.x.
Lang JH, Zhu L, Sun ZJ, Chen J. Estrogen levels and estrogen receptors in patients with stress urinary incontinence and pelvic organ prolapse. Int J Gynaecol Obstet. 2003;80(1):35–9. https://doi.org/10.1016/s0020-7292(02)00232-1.
Ewies AA, Thompson J, Al-Azzawi F. Changes in gonadal steroid receptors in the cardinal ligaments of prolapsed uteri: immunohistomorphometric data. Hum Reprod. 2004;19(7):1622–8. https://doi.org/10.1093/humrep/deh282.
Kim EJ, Chung N, Park SH, Lee KH, Kim SW, Kim JY, et al. Involvement of oxidative stress and mitochondrial apoptosis in the pathogenesis of pelvic organ prolapse. J Urology. 2013;189(2):588–94. https://doi.org/10.1016/j.juro.2012.09.041.
Elmore S. Apoptosis: a review of programmed cell death. Toxicol Pathol. 2007;35(4):495–516. https://doi.org/10.1080/01926230701320337.
Jackson SR, Avery NC, Tatlton JF, Eckford SD, Abrams P, Bailey AJ. Changes in metabolism of collagen in genitourinary prolapse. Lancet. 1996;347(9016):1658–61. https://doi.org/10.1016/s0140-6736(96)91489-0.
Zeng CY, Liu J, Wang HL, Zhou Y, Wu JW, Yan GR. Correlation between autophagy and collagen deposition in patients with pelvic organ prolapse. Female Pelvic Med Re. 2018;24(3):213–21. https://doi.org/10.1097/Spv.0000000000000455.
Yucel N, Usta A, Guzin K, Kanter M, Bilgic E, Ozel NO, et al. Immunohistochemical analysis of connective tissue in patients with pelvic organ prolapse. J Mol Histol. 2013;44(1):97–102. https://doi.org/10.1007/s10735-012-9456-5.
Välimaa H, Savolainen S, Soukka T, Silvoniemi P, Mäkelä S, Kujari H, et al. Estrogen receptor-β is the predominant estrogen receptor subtype in human oral epithelium and salivary glands. J Endocrinol. 2004;180:55–62. https://doi.org/10.1677/joe.0.1800055.
McIntush EW, Smith MF. Matrix metalloproteinases and tissue inhibitors of metalloproteinases in ovarian function. Rev Reprod. 1998;3(1):23–30. https://doi.org/10.1530/ror.0.0030023.
Dietrich W, Elenskaia K, Obermayr E, Horvat R, Mayerhofer K, Umek W, et al. Relaxin and gonadal steroid receptors in uterosacral ligaments of women with and without pelvic organ prolapse. Int Urogynecol J. 2012;23:454–500. https://doi.org/10.1007/s00192-011-1615-9.
Ewies AA, Elshafie M, Li J, Stanley A, Thompson J, Styles J, et al. Changes in transcription profile and cytoskeleton morphology in pelvic ligament fibroblasts in response to stretch: the effects of estradiol and levormeloxifene. Mol Hum Reprod. 2008;14(2):127–35. https://doi.org/10.1093/molehr/gam090.
Borazjani A, Kow N, Harris S, Ridgeway B, Damaser MS. Transcriptional regulation of connective tissue metabolism genes in women with pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2017;23(1):44–52. https://doi.org/10.1097/SPV.0000000000000337.
Vetuschi A, Pompili S, Gallone A, D’Alfonso A, Carbone MG, Carta G, et al. Immunolocalization of advanced glycation end products, mitogen activated protein kinases, and transforming growth factor-beta/Smads in pelvic organ prolapse. J Histochem Cytochem. 2018;66(9):673–86. https://doi.org/10.1369/0022155418772798.
Li BS, Guo WJ, Hong L, Liu YD, Liu C, Hong SS, et al. Role of mechanical strain-activated PI3K/Akt signaling pathway in pelvic organ prolapse. Mol Med Rep. 2016;14(1):243–53. https://doi.org/10.3892/mmr.2016.5264.
Funding
The study was supported by The National Natural Science Foundation of China (81671442, 81971366), the Beijing Natural Science Foundation (Z190021) and the Chinese Academy of Medical Sciences (CAMS) Initiative for Innovative Medicine (CAMS-2017-I2M-1-002).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Fig. 1
RT-qPCR analysis of the relative ratio of COLI/COLIII in the USL tissues of patients in the POP group (n = 35) (gray bars) and control group (n = 20) (black bars). The results represent the mean and standard deviation. p < 0.05 indicates a significant difference, and the specific p value is indicated (TIF 126 kb)
Rights and permissions
About this article
Cite this article
Zhu, Yp., Xie, T., Guo, T. et al. Evaluation of extracellular matrix protein expression and apoptosis in the uterosacral ligaments of patients with or without pelvic organ prolapse. Int Urogynecol J 32, 2273–2281 (2021). https://doi.org/10.1007/s00192-020-04446-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04446-7