Abstract
Introduction and hypothesis
This study was aimed at comparing pelvic floor parameters between the standing and supine positions using upright computed tomography (CT) and evaluating the effects of sex and age in normal healthy volunteers.
Methods
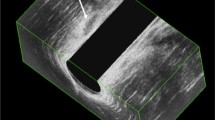
In total, 139 volunteers (70 men, mean 46.7 years; 69 women, mean 47.3 years) underwent both upright CT in the standing position and conventional CT in the supine position. The distances from the bladder neck to the pubococcygeal line (PCL) and anorectal junction (ARJ), defined as the posterior aspect of the puborectalis muscle, to PCL were measured. The length, width, and area of the levator hiatus (LH) were measured on oblique axial images.
Results
The bladder neck (men, 22.2 ± 4.9 mm vs 28.3 ± 5.3 mm; women, 9.0 ± 5.1 mm vs 19.0 ± 4.0 mm) and ARJ (men, −18.8 ± 5.5 mm vs −12.1 ± 5.1 mm; women, −20.0 ± 4.7 mm vs −11.2 ± 4.3 mm) were significantly lower in the standing position than in the supine position (all p < 0.0001). The LH area (men, 1,990 ± 380 mm2 vs 1,697 ± 329 mm2; women, 2,284 ± 344 mm2 vs 1,811 ± 261 mm2) was significantly larger in the standing position (both p < 0.0001). Differences in all parameters between the standing and supine positions were larger in women than in men. ARJ in women showed a significant tendency to descend with age only in the standing position (r = −0.29, p = 0.017).
Conclusions
The bladder neck and ARJ descend and the LH area enlarges in the standing position. Pelvic floor mobility is greater in women than in men. Descent of the ARJ in the standing position is associated with aging in women.



Similar content being viewed by others
References
Bitti GT, Argiolas GM, Ballicu N, Caddeo E, Cecconi M, Demurtas G, et al. Pelvic floor failure: MR imaging evaluation of anatomic and functional abnormalities. Radiographics. 2014;34:429–48. https://doi.org/10.1148/rg.342125050.
Garcia del Salto L, de Miguel CJ, Aguilera del Hoyo LF, Gutierrez Velasco L, Fraga Rivas P, Manzano Paradela M, et al. MR imaging-based assessment of the female pelvic floor. Radiographics. 2014;34:1417–39. https://doi.org/10.1148/rg.345140137.
Ribas Y, Hotouras A, Chan CL, Clave P. Imaging of pelvic floor disorders: are we underestimating gravity? Dis Colon Rectum. 2014;57:1242–4. https://doi.org/10.1097/DCR.0000000000000201.
Kelvin FM, Maglinte DD, Hale DS, Benson JT. Female pelvic organ prolapse: a comparison of triphasic dynamic MR imaging and triphasic fluoroscopic cystocolpoproctography. AJR Am J Roentgenol. 2000;174:81–8. https://doi.org/10.2214/ajr.174.1.1740081.
Jinzaki M, Yamada Y, Nagura T, Nakahara T, Yokoyama Y, Narita K, et al. Development of upright computed tomography with area detector for whole-body scans: phantom study, efficacy on workflow, effect of gravity on human body, and potential clinical impact. Investig Radiol. 2020;55:73–83. https://doi.org/10.1097/RLI.0000000000000603.
MacLennan AH, Taylor AW, Wilson DH, Wilson D. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000;107:1460–70.
Yamada Y, Yamada M, Yokoyama Y, Tanabe A, Matsuoka S, Niijima Y, et al. Differences in lung and lobe volumes between supine and standing positions scanned with conventional and newly developed 320-detector-row upright CT: intra-individual comparison. Respiration. 2020. https://doi.org/10.1159/000507265.
Yamada Y, Jinzaki M, Hosokawa T, Tanami Y, Sugiura H, Abe T, et al. Dose reduction in chest CT: comparison of the adaptive iterative dose reduction 3D, adaptive iterative dose reduction, and filtered back projection reconstruction techniques. Eur J Radiol. 2012;81:4185–95. https://doi.org/10.1016/j.ejrad.2012.07.013.
El Sayed RF, Alt CD, Maccioni F, Meissnitzer M, Masselli G, Manganaro L, et al. Magnetic resonance imaging of pelvic floor dysfunction—joint recommendations of the ESUR and ESGAR Pelvic Floor Working Group. Eur Radiol. 2017;27:2067–85. https://doi.org/10.1007/s00330-016-4471-7.
Goh V, Halligan S, Kaplan G, Healy JC, Bartram CI. Dynamic MR imaging of the pelvic floor in asymptomatic subjects. AJR Am J Roentgenol. 2000;174:661–6. https://doi.org/10.2214/ajr.174.3.1740661.
Barbaric ZL, Marumoto AK, Raz S. Magnetic resonance imaging of the perineum and pelvic floor. Top Magn Reson Imaging. 2001;12:83–92.
Nardos R, Thurmond A, Holland A, Gregory WT. Pelvic floor levator hiatus measurements: MRI versus ultrasound. Female Pelvic Med Reconstr Surg. 2014;20:216–21. https://doi.org/10.1097/SPV.0000000000000079.
Gregory WT, Nardos R, Worstell T, Thurmond A. Measuring the levator hiatus with axial MRI sequences: adjusting the angle of acquisition. Neurourol Urodyn. 2011;30:113–6. https://doi.org/10.1002/nau.20957.
Kepenekci I, Keskinkilic B, Akinsu F, Cakir P, Elhan AH, Erkek AB, et al. Prevalence of pelvic floor disorders in the female population and the impact of age, mode of delivery, and parity. Dis Colon Rectum. 2011;54:85–94. https://doi.org/10.1007/DCR.0b013e3181fd2356.
Barber MD, Lambers A, Visco AG, Bump RC. Effect of patient position on clinical evaluation of pelvic organ prolapse. Obstet Gynecol. 2000;96:18–22. https://doi.org/10.1016/s0029-7844(00)00859-0.
Swift SE, Herring M. Comparison of pelvic organ prolapse in the dorsal lithotomy compared with the standing position. Obstet Gynecol. 1998;91:961–4. https://doi.org/10.1016/s0029-7844(98)00111-2.
Braverman M, Kamisan Atan I, Turel F, Friedman T, Dietz HP. Does patient posture affect the ultrasound evaluation of pelvic organ prolapse? J Ultrasound Med. 2019;38:233–8. https://doi.org/10.1002/jum.14688.
Maglinte DD, Hale DS, Sandrasegaran K. Comparison between dynamic cystocolpoproctography and dynamic pelvic floor MRI: pros and cons: which is the "functional" examination for anorectal and pelvic floor dysfunction? Abdom Imaging. 2013;38:952–73. https://doi.org/10.1007/s00261-012-9870-x.
Iacobellis F, Brillantino A, Renzi A, Monaco L, Serra N, Feragalli B, et al. MR imaging in diagnosis of pelvic floor descent: supine versus sitting position. Gastroenterol Res Pract. 2016;2016:6594152. https://doi.org/10.1155/2016/6594152.
Friedman B, Stothers L, Lazare D, Macnab A. Positional pelvic organ prolapse (POP) evaluation using open, weight-bearing magnetic resonance imaging (MRI). Can Urol Assoc J. 2015;9:197–200. https://doi.org/10.5489/cuaj.2767.
Abdulaziz M, Kavanagh A, Stothers L, Macnab AJ. Relevance of open magnetic resonance imaging position (sitting and standing) to quantify pelvic organ prolapse in women. Can Urol Assoc J. 2018;12:E453–60. https://doi.org/10.5489/cuaj.5186.
Grob ATM, Olde Heuvel J, Futterer JJ, Massop D, Veenstra van Nieuwenhoven AL, Simonis FFJ, et al. Underestimation of pelvic organ prolapse in the supine straining position, based on magnetic resonance imaging findings. Int Urogynecol J. 2019;30:1939–44. https://doi.org/10.1007/s00192-018-03862-0.
Mouritsen L, Bach P. Ultrasonic evaluation of bladder neck position and mobility: the influence of urethral catheter, bladder volume, and body position. Neurourol Urodyn. 1994;13:637–46.
Dietz HP, Shek C, Clarke B. Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Ultrasound Obstet Gynecol. 2005;25:580–5. https://doi.org/10.1002/uog.1899.
Woodfield CA, Krishnamoorthy S, Hampton BS, Brody JM. Imaging pelvic floor disorders: trend toward comprehensive MRI. AJR Am J Roentgenol. 2010;194:1640–9. https://doi.org/10.2214/AJR.09.3670.
Bushman W. Etiology, epidemiology, and natural history of benign prostatic hyperplasia. Urol Clin North Am. 2009;36:403–415, v. https://doi.org/10.1016/j.ucl.2009.07.003.
Lee SE, Chung JS, Han BK, Moon KH, Hwang SI, Lee HJ, et al. Relationship of prostate-specific antigen and prostate volume in Korean men with biopsy-proven benign prostatic hyperplasia. Urology. 2008;71:395–8. https://doi.org/10.1016/j.urology.2007.10.019.
Howard D, Delancey JO, Tunn R, Ashton-Miller JA. Racial differences in the structure and function of the stress urinary continence mechanism. Obstet Gynecol. 2000;95:713–7.
Funding
This study was supported by the Japan Society for the Promotion of Science (JSPS KAKENHI: Grant Number JP17H04266), Uehara Memorial Foundation, and Canon Medical Systems (Otawara, Japan) for Masahiro Jinzaki.
Author information
Authors and Affiliations
Contributions
K. Narita: data collection, data analysis, manuscript writing; Y. Yamada: protocol development, data collection, manuscript editing; M. Yamada: protocol development, data collection, manuscript editing; Y. Yokoyama: data collection, data analysis, manuscript editing; T. Nakahara: data collection, manuscript editing; M. Jinzaki: project development, manuscript editing.
Corresponding authors
Ethics declarations
Conflicts of interest
Masahiro Jinzaki received a grant from Canon Medical Systems, which loaned the upright CT device to Keio University. The funder was not involved in the design of the study; collection, analysis, and interpretation of the data; or writing of the manuscript. The other authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Narita, K., Yamada, Y., Yamada, M. et al. Pelvic floor morphology in the standing position using upright computed tomography: age and sex differences. Int Urogynecol J 31, 2387–2393 (2020). https://doi.org/10.1007/s00192-020-04335-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04335-z