Abstract
Introduction and hypothesis
Although pelvic floor disorders (PFDs) are a significant public health issue in higher income countries, less is known about these disorders and associated risk factors in low income countries. We aimed to determine prevalence and associated risk factors for stress urinary incontinence (SUI), urge urinary incontinence (UUI), and pelvic organ prolapse (POP) in reproductive age women in Sarlahi District in rural Nepal.
Methods
We conducted a community-based cross-sectional survey of parous, reproductive age women in rural Nepal and screened for pelvic floor disorders using validated screening questions for PFDs. Overall frequency of self-reported symptoms for SUI, UUI, and POP was estimated and compared across demographic and pregnancy history information.
Results
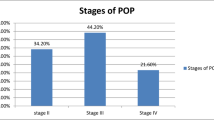
Of 14,469 women available for analysis, the mean (SD, range) age was 33.5 (8.2, 13–52) years, and median (range) number of pregnancies was 4 (1–15). The prevalence of SUI was 24.1% (95% CI: 23.3–24.8), of UUI was 13.5% (95% CI: 13.0–14.1), and of POP was 8.0% (95% CI: 7.5–8.4). Bivariate analysis identified the risk of PFD increased incrementally with age and number of vaginal deliveries; these covariates were highly correlated. Multivariable logistic regression revealed age, vaginal deliveries, and previous pelvic surgeries were independently associated with PFD.
Conclusions
PFDs are common in a community of parous, reproductive age women in rural Nepal. Risk factors for these conditions are similar to risk factors found in higher income countries.


Similar content being viewed by others
References
Sung VW, Hampton BS. Epidemiology of pelvic floor dysfunction. Obstet Gynecol Clin N Am. 2009;36(3):421–43.
2017 World Population Data Sheet [Internet]. [cited 2017 Sept 12]. Available from: http://www.prb.org/pdf17/2017_World_Population.pdf.
Walker GJA, Gunasekera P. Pelvic organ prolapse and incontinence in developing countries: review of prevalence and risk factors. Int Urogynecol J. 2011;22(2):127–35.
The World Bank [Internet]. GNI per capita, Atlas method. [cited 2017 Sep 8]. Available from: http://data.worldbank.org/indicator/NY.GNP.PCAP.CD.
The DHS Program - Quality information to plan, monitor and improve population, health, and nutrition programs [Internet]. [cited 2018 Mar 22]. Available from: https://dhsprogram.com/.
Chen C, Barry D, Khatry SK, Klasen EM, Singh M, LeClerq SC, et al. Validation of an obstetric fistula screening questionnaire in rural Nepal: a community-based cross-sectional and nested case-control study with clinical examination. BJOG. 2017;124(6):955–64.
Tönshoff B. Ethical conduct of clinical research involving children. Marilyn J. field and Richard E. Behrman for the committee on clinical research involving children of the Institute of Medicine, the National Academies Press, Washington, DC, USA, 2004, 425 pp., USD 47.95, ISBN 0-309-09181-0. Qual Assur J. 2005;9(2):146. https://doi.org/10.1002/qaj.330.
McNary A. Consent to treatment of minors. Innov Clin Neurosci. 2014;11(3–4):43–5.
Sandvik H, Hunskaar S, Vanvik A, Bratt H, Seim A, Hermstad R. Diagnostic classification of female urinary incontinence: an epidemiological survey corrected for validity. J Clin Epidemiol. 1995;48:339–43.
Barber MD, Neubauer NL, Klein-Olarte V. Can we screen for pelvicorgan prolapse without a physical examination in epidemiologic studies? Am J Obstet Gynecol. 2006;195:942–8.
Lien Y-S, Chen G-D, Ng S-C. Prevalence of and risk factors for pelvic organ prolapse and lower urinary tract symptoms among women in rural Nepal. Int J Gynaecol Obstet. 2012;119(2):185–8.
Gautam S, Adhikari RK, Dangol A. Associated factors for uterine prolapse. J Nepal Health Res Counc. 2012;10(1):1–4.
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311–6.
Bodner-Adler B, Shrivastava C, Bodner K. Risk factors for uterine prolapse in Nepal. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(11):1343–6.
Thapa S, Angdembe M, Chauhan D, Joshi R. Determinants of pelvic organ prolapse among the women of the western part of Nepal: a case-control study. J Obstet Gynaecol Res. 2014;40(2):515–20.
Onur R, Deveci SE, Rahman S, Sevindik F, Acik Y. Prevalence and risk factors of female urinary incontinence in eastern Turkey. Int J Urol. 2009;16(6):566–9.
Incontinence: 5th International Consultation on Incontinence, Paris, February 2012. 2013. 1981 p. 15–107.
Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the Women’s health initiative: gravity and gravidity. Am J Obstet Gynecol. 2002;186(6):1160–6.
Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, et al. Prevalence and trends of symptomatic pelvic floor disorders in US women. Obstet Gynecol. 2014;123(1):141–8.
Suskind AM, Dunn RL, Morgan DM, DeLancey JOL, Rew KT, Wei JT. A screening tool for clinically relevant urinary incontinence. Neurourol Urodyn. 2015;34(4):332–5.
Lukacz ES, Lawrence JM, Contreras R, Nager CW, Luber KM. Parity, mode of delivery, and pelvic floor disorders. Obstet Gynecol. 2006;107(6):1253–60.
Barber MD, Neubauer NL, Klein-Olarte V. Can we screen for pelvic organ prolapse without a physical examination in epidemiologic studies? Am J Obstet Gynecol. 2006;195(4):942–8.
Bradley CS, Nygaard IE. Vaginal wall descensus and pelvic floor symptoms in older women. Obstet Gynecol. 2005;106(4):759–66.
Swift SE, Tate SB, Nicholas J. Correlation of symptoms with degree of pelvic organ support in a general population of women: what is pelvic organ prolapse? Am J Obstet Gynecol. 2003;189(2):372–7.
Samuelsson EC, Arne Victor FT, Tibblin G, Svärdsudd KF. Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol. 1999;180(2):299–305.
Burgio KL, Ives DG, Locher JL, Arena VC, Kuller LH. Treatment seeking for urinary incontinence in older adults. J Am Geriatr Soc. 1994;42(2):208–12.
Holst K, Wilson PD. The prevalence of female urinary incontinence and reasons for not seeking treatment. N Z Med J. 1988;101(857):756–8.
Funding
This work was funded by the Maren Foundation, the Johns Hopkins University Center for Global Health, and the National Institute of Child Health and Development, United States National Institutes of Health (R01HD060712).
Author information
Authors and Affiliations
Contributions
• Chen: Study design, obtained funding, and oversaw all aspects of the study design and implementation, analysis, and manuscript writing.
• Avondstondt: Data interpretation and manuscript writing.
• Khatry: Study design, project implementation, data analysis, and manuscript writing
• Singh: Study design, project implementation, data analysis, and manuscript writing
• Klasen: Study design, project implementation, data analysis, and manuscript writing
• LeClerq: Study design, project implementation, data analysis, and manuscript writing
• Katz: Study design, project implementation, data analysis, and manuscript writing
• Tielsch: Study design, project implementation, data analysis, and manuscript writing
• Mullany: Study design, project implementation, data analysis, and manuscript writing
Corresponding author
Ethics declarations
Ethics committee approval
IRB approval was obtained both from Johns Hopkins School of Public Health (Baltimore, MD, USA, IRB no. 00002572) and the Institute of Medicine, Tribhuvan University (Kathmandu, Nepal), on 27 January 2010.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, C.C.G., Avondstondt, A.M., Khatry, S.K. et al. Prevalence of symptomatic urinary incontinence and pelvic organ prolapse among women in rural Nepal. Int Urogynecol J 31, 1851–1858 (2020). https://doi.org/10.1007/s00192-019-04129-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04129-y