Abstract
Introduction and hypothesis
This study was aimed at measuring levator ani bowl volume at rest and while straining, comparing women with and without prolapse (controls), and assessing the ability of measures of the mid-sagittal bowl area, levator hiatus (LH), and urogenital hiatus (UGH) to predict bowl volume.
Methods
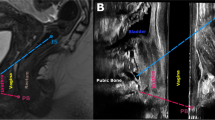
Forty MRI scans previously acquired in case-control prolapse studies, including 20 women with prolapse and 20 women without prolapse, of similar age and parity, were selected. 3D models of rest and strain bowl volumes were made using sagittal scans and 3D Slicer®. Mid-sagittal bowl area, UGH, and LH were measured using ImageJ. Data were analyzed using two sample t tests, effect sizes, and Pearson’s correlation coefficients at the 0.05 significance level.
Results
Data were acquired in a total of 40 total women. Levator bowl volume at strain had a correlation coefficient of 0.5 with bowl volume at rest. During straining, prolapse subjects had a 53% larger bowl volume than control subjects (254 ± 86 cm3 vs 166 ± 44 cm3, p < 0.001), but at rest, the difference was 34% (138 ± 40 cm3 vs 103 ± 25 cm3, p = 0.002). Effect sizes for all parameters were large (d > 0.75). The strongest correlation with straining bowl volume was mid-sagittal straining bowl area (r = 0.86), followed by LH strain (r = 0.80), then UGH strain (r = 0.76).
Conclusions
Straining levator bowl volume is substantially different than measures made at rest, with only a quarter of straining values explained by resting measurements. The bowl area at strain is the best 2D measurement estimating bowl volume and explains 74% of straining bowl volume.



Similar content being viewed by others
References
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300:1311–6.
Nygaard I, Brubaker L, Zyczynski HM, Cundiff G, Richter H, Gantz M, et al. Long-term outcomes following abdominal Sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309:2016–24.
Chen L, Lisse S, Larson K, Berger MB, Ashton-Miller JA, DeLancey JO. Structural failure sites in anterior vaginal wall prolapse: identification of a collinear triad. Obstet Gynecol. 2016;128:853–62.
Rodrigues AA Jr, Bassaly R, McCullough M, Terwilliger HL, Hart S, Downes K, et al. Levator ani subtended volume: a novel parameter to evaluate levator ani muscle laxity in pelvic organ prolapse. Am J Obstet Gynecol. 2012;206:244.e1–9.
Rodrigues Junior AA, Herrera-Hernadez MC, Bassalydo R, McCullough M, Terwilliger HL, Downes K, et al. Estimates of the levator ani subtended volume based on magnetic resonance linear measurements. Neurourol Urodynam. 2016;35:199–205.
Wyman AM, Rodrigues AA Jr, Hahn L, Greene KA, Bassaly R, Hart S, et al. Estimated levator ani subtended volume: a novel assay for predicting surgical failure after uterosacral ligament suspension. Am J Obstet Gynecol. 2016;214:611.e1–6.
Sammarco AG, Nandikanti L, Kobernik EK, Xie B, Jankowski A, Swenson CW, et al. Interactions between pelvic organ protrusion, levator ani descent, and hiatal enlargement in women with and without prolapse. Am J Obstet Gynecol. 2017;217:614.e1–7.
Pannu HK, Genadry R, Gearhart S, Kaufman HS, Cundiff GW, Fishman EK. Focal levator ani eventrations: detection and characterization by magnetic resonance in patients with pelvic floor dysfunction. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:89–93.
DeLancey JO, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM, et al. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol. 2007;109:295–302.
Nandikanti L, Sammarco AG, Kobernik EK, DeLancey JOL. Levator ani defect severity and its association with enlarged hiatus size, levator bowl depth, and prolapse size. Am J Obstet Gynecol. 2018;218:537–9.
Lee SL, Tan E, Khullar V, Gedroyc W, Darzi A, Yang GZ. Physical-based statistical shape modeling of the levator ani. IEEE Trans Med Imaging. 2009;28(6):926–36.
Vaughan MH, Siddiqui NY, Newcomb LK, Weidner AC, Kawasaki A, Visco AG, et al. Surgical alteration of genital Hiatus size and anatomic failure after vaginal vault suspension. Obstet Gynecol. 2018;131:1137–44.
Cundiff GW, Harris RL, Coates K, Low VH, Bump RC, Addison WA. Abdominal sacral colpoperineopexy: a new approach for correction of posterior compartment defects and perineal descent associated with vaginal vault prolapse. Am J Obstet Gynecol. 1997;177:1345–53.
Acknowledgements
Supported by National Institutes of Health grants P50 HD044406 and R01 HD038665. The NIH did not play a role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Nandikanti, L., Sammarco, A.G., Chen, L. et al. Levator bowl volume during straining and its relationship to other levator measures. Int Urogynecol J 30, 1457–1463 (2019). https://doi.org/10.1007/s00192-019-04006-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04006-8