Abstract
Introduction and hypothesis
We compared pre- and postoperative sexual function scores in sexually active women undergoing pelvic organ prolapse (POP) surgery.
Methods
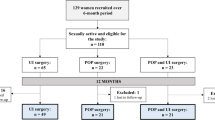
Planned secondary analysis of women enrolled in the Restricted Convalescence: Outcomes Following Urogynecologic Procedures study, a randomized trial of postoperative activity after POP surgery. All participants could return to sexual activity at 6 weeks. Participants completed the Pelvic Floor Distress Inventory (PFDI), the Patient-Reported Outcomes Measurement Information System (PROMIS) profile, and the Golombok Rust Inventory of Sexual Satisfaction (GRISS) questionnaires at baseline and 3 months. GRISS is a validated 28-item survey for heterosexual couples that contains seven subscales to assess sexual function. Higher scores represent worse sexual function.
Results
Thirty-seven sexually active women were assessed. Mean age ± standard deviation (SD) was 56 ± 11, most of whom (92%) were Caucasian; 78% had undergone minimally invasive sacrocolpopexy, and the remainder had native tissue vaginal repairs. GRISS scores improved 3 months after surgery [4.5 ± 2.6 to 3.6 ± 2.2, p < 0.001; mean decrease of 0.9, 95% confidence interval (CI) 0.36–1.36]. PFDI scores improved from 122 ± 53 at baseline to 28 ± 31 at 3 months (p < 0.001). Higher GRISS scores were correlated with higher PFDI scores (Spearman’s rho = 0.35, p = 0.03) at baseline and 3 months (Spearman’s rho = 0.31, p = 0.03). Several GRISS subscales improved after surgery: partner avoidance (p = 0.01), vaginismus (p = 0.02), noncommunication (p = 0.01), dissatisfaction (p = 0.03), and anorgasmia (p = 0.001). However, sexual infrequency (p = 0.08) and nonsensuality (p = 0.4) did not change. Fifty-one percent had sexual dysfunction before surgery, which decreased to 32% after surgery (p = 0.04).
Conclusion
Sexual function and satisfaction are significantly improved 3 months following POP surgery. Improved sexual function is correlated with improved pelvic floor symptoms.

Similar content being viewed by others
References
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311.
Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol. 2014;123(1):141–8.
Smith FJ, Holman CD, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096–100.
Bradley CS, Nygaard IE. Vaginal wall descensus and pelvic floor symptoms in older women. Obstet Gynecol. 2005;106:759.
Swift SE, Tate SB, Nicholas J. Correlation of symptoms with degree of pelvic organ support in a general population of women: what is pelvic organ prolapse? Am J Obstet Gynecol. 2003;189:372.
Pauls RN, Segal JL, Silva WA, Kleeman SD, Karram MM. Sexual function in patients presenting to a urogynecology practice. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(6):576–80.
Rogers GR, Villarreal A, Kammerer-Doak D, Qualls C. Sexual function in women with and without urinary incontinence and/or pelvic organ prolapsed. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12:361–5.
Rogers RG, Kammerer-Doak D, Darrow A, Murray K, Qualls C, Olsen A, et al. Does sexual function change after surgery for stress urinary incontinence and/or pelvic organ prolapse? A multicenter prospective study. Am J Obstet Gynecol. 2006;195(5):e1–4.
Thakar R, Chawla S, Scheer I, Barrett G, Sultan AH. Sexual function following pelvic floor surgery. Int J Gynecol Obstet. 2008;102:110–4.
Pauls RN, Silva WA, Rooney CM, Siddighi S, Kleeman SD, Dryfhout V, et al. Sexual function after vaginal surgery for pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol. 2007;197:622.e1–7.
Occhino JA, Trabuco EC, Heisler CA, Klingele CJ, Gebhart JB. Changes in vaginal anatomy and sexual function after vaginal surgery. Int Urogynecol J. 2011;22:799–804.
Roos AM, Thakar R, Sultan AH, de Leeuw JW, Paulus AT. The impact of pelvic floor surgery on female sexual function: a mixed quantitative and qualitative study. BJOG. 2014;121(1):92–100. discussion 101
Rust J, Golombok S. The Golombok rust inventory of sexual satisfaction (GRISS). Br J Clin Psychol. 1985;24:63–4.
Mueller MG, Lewicky-Gaupp C, Collins SA, Abernethy MG, Alverdy A, Kenton K. Activity restriction recommendations and outcomes after reconstructive pelvic surgery: a randomized controlled trial. Obstet Gynecol. 2017;129(4):608–14.
Lowenstein L, Gamble T, Sanses T, et al. Sexual function is related to body image perception in women with pelvic organ prolapse. J Sex Med. 2010;7(2 Pt 2):1023–8.
Handa VL, Zyczynski HM, Brubaker L, et al. Sexual function before and after Sacrocolpopexy for pelvic organ prolapse. Am J Obstet Gynecol. 2007;197(6):629.e1–6. https://doi.org/10.1016/j.ajog.2007.08.016.
Jelovsek JE, Barber MD. Women seeking treatment for advanced pelvic organ prolapse have decreased body image and quality of life. Am J Obstet Gynecol. 2006;194(5):1455–61.
Zielinski R, Miller J, Low LK, Sampselle C, DeLancey JO. The relationship between pelvic organ prolapse, genital body image and sexual health. Neurourol Urodyn. 2012;31(7):1145–8.
Helstrom L, Nilsson B. Impact of vaginal surgery on sexuality and quality of life in women with urinary incontinence or genital descensus. Acta Obstet Gynecol Scand. 2005;84:79–84.
Holley VR, Gleason B, Apffel L, Scott S. Sexual function after sacrospinous ligament fixation for vaginal vault prolapse. J Reprod Med. 1996;41:355–8.
Kahn M, Stanton S. Posterior colporrhaphy: its effects on bowel and sexual function. Br J Obstet Gynaecol. 1997;104:82–6.
Weber M, Walters M, Piedmonte M. Sexual function and vaginal anatomy in women before and after surgery for pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol. 2000;182:1610–5.
Kahn MA, Stanton SL. Posterior colporrhaphy: its effects on bowel and sexual function. Br J Obstet Gynaecol. 1997;104(1):82–6.
Diwadkar GB, Barber MD, Feiner B, Maher C, Jelovsek JE. Complication and reoperation rates after apical vaginal prolapse surgical repair: a systematic review. Obstet Gynecol. 2009;113(2 Pt 1):367–73.
Sözeri-Varma G, Kalkan-Oğuzhanoğlu N, Karadağ F, Ozdel O. The effect of hysterectomy and/or oophorectomy on sexual satisfaction. Climacteric. 2011;14(2):275–81.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Kimberly Kenton has received research funding from Boston Scientific. Drs. Kenton and Collins are expert witnesses for Ethicon. The remaining authors have no conflicts of interest to report.
Additional information
Presentation
This work was presented orally as a poster at the American Urogynecology Society Meeting in 2017 in Providence, Rhode Island, USA.
Electronic supplementary material
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Geynisman-Tan, J., Kenton, K., Komar, A. et al. Recovering sexual satisfaction after prolapse surgery: a secondary analysis of surgical recovery. Int Urogynecol J 29, 1675–1680 (2018). https://doi.org/10.1007/s00192-018-3690-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3690-7