Abstract
Introduction and hypothesis
The impact of estradiol-based hormone therapy (HT) on the incidence of stress urinary incontinence (SUI) is unknown. Therefore, we compared the use of such HT regimens and tibolone in women with and without SUI.
Methods
The women with a history of SUI operation (N = 15,002) were identified from the Finnish National Hospital Discharge Register, and the control women without such an operation (N = 44,389) from the Finnish Central Population Register. The use of HT was traced from the National Drug Reimbursement Register, and the odd ratios (ORs) with 95% confidence intervals (95% CIs) for SUI were calculated by using the conditional logistic regression analysis.
Results
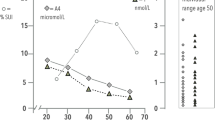
The cases had used any HT more often than the controls. The use of systemic estradiol-only or estradiol–progestin therapy was accompanied by an increased SUI risk (OR 3.8, 95% CI: 3.6–4.0 and OR 2.7, 95% CI: 2.6–2.9 respectively). The use of estradiol with noretisterone acetate showed a higher risk of increase than that with medroxyprogesterone acetate. Age over 55 years at the initiation of systemic HT was accompanied by a higher SUI risk increase than that under 55 years of age. The use of tibolone, an estradiol + levonorgestrel-releasing intrauterine device, or vaginal estradiol also increased the risk.
Conclusions
The use of HT regimens may predispose to the de novo development or worsening of pre-existing SUI. Thus, caution is needed when these regimens are prescribed to women with mild stress-related urine leakage or with established SUI risk factors.
Similar content being viewed by others
References
Minassian VA, Bazi T, Stewart WF. Clinical epidemiological insights into urinary incontinence. Int Urogynecol J. 2017;28:687–96.
Al-Mukhtar Othman J, Akervall S, Milsom I, Gyhagen M. Urinary incontinence in nulliparous women aged 25-64 years: a national survey. Am J Obstet Gynecol. 2017;216:149.e1–149.e11.
Xie Z, Shi H, Zhou C, Dong M, Hong L, Jin H. Alterations of estrogen receptor-alpha and -beta in the anterior vaginal wall of women with urinary incontinence. Eur J Obstet Gynecol Reprod Biol. 2007;134:254–8.
Skala CE, Petry IB, Albrich SB, Puhl A, Naumann G, Koelbl H. The effect of hormonal status on the expression of estrogen and progesterone receptor in vaginal wall and periurethral tissue in urogynecological patients. Eur J Obstet Gynecol Reprod Biol. 2010;153:99–103.
Kobata SA, Girao MJ, Baracat EC, Kajikawa M, Di Bella V Jr, Sartori MG, et al. Estrogen therapy influence on periurethral vessels in postmenopausal incontinent women using Dopplervelocimetry analysis. Maturitas. 2008;61:243–7.
Weber MA, Kleijn MH, Langendam M, Limpens J, Heineman MJ, Roovers JP. Local oestrogen for pelvic floor disorders: a systematic review. PLoS One. 2015;10:e0136265.
Cody JD, Jacobs ML, Richardson K, Moehrer B, Hextall A. Oestrogen therapy for urinary incontinence in post-menopausal women. Cochrane Database Syst Rev. 2012;10:CD001405.
Hendrix SL, Cochrane BB, Nygaard IE, Handa VL, Barnabei VM, Iglesia C, et al. Effects of estrogen with and without progestin on urinary incontinence. JAMA. 2005;293:935–48.
Bhavnani BR, Stanczyk FZ. Pharmacology of conjugated equine estrogens: efficacy, safety and mechanism of action. J Steroid Biochem Mol Biol. 2014;142:16–29.
Grady D, Brown JS, Vittinghoff E, Applegate W, Varner E, Snyder T, et al. Postmenopausal hormones and incontinence: the heart and estrogen/progestin replacement study. Obstet Gynecol. 2001;97:116–20.
Grodstein F, Lifford K, Resnick NM, Curhan GC. Postmenopausal hormone therapy and risk of developing urinary incontinence. Obstet Gynecol. 2004;103:254–60.
Townsend MK, Curhan GC, Resnick NM, Grodstein F. Postmenopausal hormone therapy and incident urinary incontinence in middle-aged women. Am J Obstet Gynecol. 2009;200:86.e1–5.
Ulmsten U, Falconer C, Johnson P, Jomaa M, Lanner L, Nilsson CG, et al. A multicenter study of tension-free vaginal tape (TVT) for surgical treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1998;9:210–3.
Palva K, Rinne K, Aukee P, Kivela A, Laurikainen E, Takala T, et al. A randomized trial comparing tension-free vaginal tape with tension-free vaginal tape-obturator: 36-month results. Int Urogynecol J. 2010;21:1049–55.
Savolainen-Peltonen H, Tuomikoski P, Korhonen P, Hoti F, Vattulainen P, Gissler M, et al. Cardiac death risk in relation to the age at initiation or the progestin component of hormone therapies. J Clin Endocrinol Metab. 2016;101:2794–801.
Lyytinen H, Pukkala E, Ylikorkala O. Breast cancer risk in postmenopausal women using estradiol-progestogen therapy. Obstet Gynecol. 2009;113:65–73.
Lumsden MA, Davies M, Sarri G, Guideline Development Group for Menopause. Diagnosis and management (NICE clinical guideline no. 23). Diagnosis and management of menopause: the national institute of health and care excellence (NICE) guideline. JAMA Intern Med. 2016;176:1205–6.
Formoso G, Perrone E, Maltoni S, Balduzzi S, Wilkinson J, Basevi V, et al. Short-term and long-term effects of tibolone in postmenopausal women. Cochrane Database Syst Rev. 2016;10:CD008536.
Jackson S, James M, Abrams P. The effect of oestradiol on vaginal collagen metabolism in postmenopausal women with genuine stress incontinence. BJOG. 2002;109:339–44.
Moalli PA, Talarico LC, Sung VW, Klingensmith WL, Shand SH, Meyn LA, et al. Impact of menopause on collagen subtypes in the arcus tendineous fasciae pelvis. Am J Obstet Gynecol. 2004;190:620–7.
Nilsson CG, Palva K, Aarnio R, Morcos E, Falconer C. Seventeen years' follow-up of the tension-free vaginal tape procedure for female stress urinary incontinence. Int Urogynecol J. 2013;24:1265–9.
Kudish BI, Shveiky D, Gutman RE, Jacoby V, Sokol AI, Rodabough R, et al. Hysterectomy and urinary incontinence in postmenopausal women. Int Urogynecol J. 2014;25:1523–31.
Schreiber Pedersen L, Lose G, Hoybye MT, Elsner S, Waldmann A, Rudnicki M. Prevalence of urinary incontinence among women and analysis of potential risk factors in Germany and Denmark. Acta Obstet Gynecol Scand. 2017;96:939–48.
Cobin RH, Goodman NF, AACE Reproductive Endocrinology Scientific Committee. American Association of Clinical Endocrinologists and American College of Endocrinology position statement on menopause—2017 update. Endocr Pract. 2017;23:869–80.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
PR-S has received funding for congress attendance from Johnson & Johnson and Astellas Pharma. HS-P has been a speaker for Mylan and received funding for congress attendance from Mylan and MSD. TM has been a speaker and/or received consulting fees from Mylan and Astellas Pharma.
MG and OY have nothing to disclose. FH and PV work for EPID Research. EPID Research is a company that performs financially supported studies for several pharmaceutical companies.
Rights and permissions
About this article
Cite this article
Rahkola-Soisalo, P., Savolainen-Peltonen, H., Gissler, M. et al. Increased risk for stress urinary incontinence in women with postmenopausal hormone therapy. Int Urogynecol J 30, 251–256 (2019). https://doi.org/10.1007/s00192-018-3682-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3682-7