Abstract
Introduction and hypothesis
Pelvic organ prolapse (POP) commonly presents with a “vaginal lump or bulge” and/or a “dragging sensation.” The first symptom correlates strongly with clinical and imaging data. However, a “dragging sensation” may be less specific. Hence, we investigated the predictive value of both symptoms for POP.
Methods
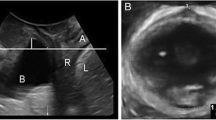
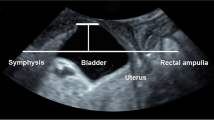
This was a retrospective study involving archived data sets of women seen between November 2013 and May 2014. All underwent a clinical interview, POPQ examination, and 4D translabial ultrasound (TLUS). The main outcome measure was organ descent on clinical examination and TLUS. Offline analysis for organ descent was undertaken blinded against all other data.
Results
A total of 224 women were assessed. Mean age was 57 (23–84) years. Median parity was 3 (0–7). Ninety-three percent (n=208) were vaginally parous. Fifty-eight percent (n=129) complained of symptoms of prolapse: 49% (n=110) of a vaginal lump, 27% (n=61) of a dragging sensation. Clinically, mean point B anterior (Ba) was −0.86 (−3 to +7.5) cm, mean cervical station (C) was −4.1 (−9 to +8) cm, mean point B posterior (Bp) was −1.1 (−3 to +5) cm. On imaging, mean bladder, uterine, and rectal descent were −8.3 (−68.0 to 34) mm, +18.6 (−56.4 to 46.3) mm, and −5.3 (−39.8 to 36) mm respectively. On univariate analysis, both symptoms were strongly associated with objective prolapse clinically and on TLUS, with “vaginal lump” consistently the stronger predictor.
Conclusions
The symptom of a “vaginal lump or bulge” was consistently a stronger predictor of objective POP than “dragging sensation.” This finding was insensitive to adjustments for potential confounders. However, a “dragging sensation” is clearly a symptom of prolapse.
Similar content being viewed by others
References
Smith F, Holman D, Moorin R, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116:1096–100.
Wu J, Hundley A, Fulton R, Myers E. Forecasting the prevalence of pelvic floor disorders in U.S. women: 2010 to 2050. Obstet Gynecol. 2009;114:1278–83.
FDA. Urogynecologic surgical mesh: update on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse. FDA 2011.http://www.fda.gov/downloads/MedicalDevices/Safety/AlertsandNotices/UCM262760.pdf
Barber M, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783–90. doi:10.1007/s00192-013-2169-9.
Cooper J, Annappa M, Dracocardos D, Cooper W, Muller S, Mallen C. Prevalence of genital prolapse symptoms in primary care: a cross-sectional survey. Int Urogynecol J. 2015;26:505–10.
Hagen S, Stark D. Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2011;7(12):CD003882. doi:10.1002/14651858. CD003882.pub4.
Dietz H. Female pelvic organ prolapse—a review. Aust Fam Physician. 2015;44(7):446–52.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Dietz HP, Haylen BT, Broome J. Ultrasound in the quantification of female pelvic organ prolapse. Ultrasound Obstet Gynecol. 2001;18(5):511–4.
Dietz H. Pelvic floor ultrasound. Curr Surg Rep. 2013;1:167–81.
Ulrich D, Guzman Rojas R, Dietz H, Trutnovsky G. Use of a visual analog scale for evaluation of bother from pelvic organ prolapse. Ultrasound Obstet Gynecol. 2014;43(6):693–7.
Tan L, Shek K, Kamisan Atan I, Guzman Rojas R, Dietz H. The repeatability of sonographic measures of functional pelvic floor anatomy. Int Urogynecol J. 2015;26(11):1667–72.
Shek KL, Dietz HP. Assessment of pelvic organ prolapse: a review. Ultrasound Obstet Gynecol. 2016;48:681–92.
Dietz HP. Pelvic floor ultrasound in prolapse: what’s in it for the surgeon? Int Urogynecol J. 2011;22:1221–32.
Dietz HP, Wong V, Shek KL. A simplified method for the determination of levator hiatal dimensions. Aust N Z J Obstet Gynaecol. 2011;51:540–3.
Dietz HP, Bernardo MJ, Kirby A, Shek KL. Minimal criteria for the diagnosis of avulsion of the puborectalis muscle by tomographic ultrasound. Int Urogynecol J. 2011;22:699–705.
Digesu A, Khullar V, Cardozo L, Robinson D, Salvatore S. P-QOL: a validated questionnaire to assess the symptoms and quality of life of women with urogenital prolapse. Int Urogynecol J. 2005;16:176–81.
Swift SE, Tate SB, Nicholas J. Correlation of symptoms with degree of pelvic organ support in a general population of women: what is pelvic organ prolapse? Am J Obstet Gynecol. 2003;189:372–9.
Barber MD, Kuchibhatla MN, Pieper CF, Bump RC. Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol. 2001;185:1388–95.
Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE. Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol. 2001;185(6):1332–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
H.P. Dietz has received unrestricted educational grants and honoraria from GE Medical. The other authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Dietz, H.P., Chatel, C. & Atan, I.K. Is a “dragging sensation” a symptom of female pelvic organ prolapse?. Int Urogynecol J 29, 703–707 (2018). https://doi.org/10.1007/s00192-017-3410-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3410-8