Abstract
Introduction and hypothesis
We compared persistence on overactive bladder (OAB) pharmacotherapy in patients treated in the Female Pelvic Medicine and Reconstructive Surgery (FPMRS) department compared with patients treated in the Internal Medicine (IM) and General Urology (GU) departments within an integrated health-care system. We hypothesized that persistence would be higher among FPMRS patients.
Methods
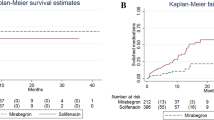
This was a retrospective cohort study. Patients with at least one prescription for OAB between January 2003 and July 2014 were identified. Demographic, prescription and treatment specialty data and data on the use of third-line therapies were collected. The primary outcome was persistence, defined as days on continuous pharmacotherapy. Discontinuation was defined as a treatment gap of ≥45 days. Discontinuation-free probabilities were calculated using the Kaplan-Meier method and compared among the specialties. Predictors of persistence were estimated using logistic regression with adjustment for covariates. Pearson correlation coefficients were calculated to identify risk associations.
Results
A total of 252 subjects were identified. At 12 weeks, 6 months and 1 year, FPMRS patients had the highest persistence rates of 93 %, 87 % and 79 % in contrast to 72 %, 68 % and 50 % in GU patients, and 83 %, 71 % and 63 % in IM patients (p = 0.006, p = 0.007, p = 0.001, respectively). The median persistence in FPMRS patients was 738 days, in GU patients 313 days and in IM patients 486 days (p = 0.006). Of the FPMRS patients, 61 % switched to at least a second medication, as compared to 27 % of IM patients and 14 % of GU patients (p < 0.0001).
Conclusions
Persistence on OAB pharmacotherapy was higher among FPMRS patients than among GU and IM patients in this community setting. These results suggest that persistence is higher under subspecialist supervision.


Similar content being viewed by others
References
Basra RK, Wagg A, Chapple C, Cardozo L, Castro-Diaz D, Pons ME et al (2008) A review of adherence to drug therapy in patients with overactive bladder. BJU Int 102:774–779.
Stewart W, Rooyen JV, Cundiff F, Abrams P, Herzog AR, Corey R et al (2003) Prevalence and burden of overactive bladder in the United States. World J Urol 20:327–336.
Coyne KS, Sexton CC, Vats V, Thompson C, Kopp ZS, Milsom I (2011) National community prevalence of overactive bladder in the United States stratified by sex and age. Urology 77(5):1081–1087.
Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S et al (2006) Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 50:1306–1315.
Cheung WW, Khan NH, Choi KK, Bluth MH, Vincent MT (2009) Prevalence, evaluation and management of overactive bladder in primary care. BMC Fam Pract 10:8.
Cheung WW, Borawski D, Abulafia O, Vincent MT, Harel M, Bluth MH (2011) Characterization of overactive bladder in women in a primary car setting. Open Access J Urol 3:29–34.
Staskin DR, MacDiarmid SA (2006) Pharmacologic management of overactive bladder: practical options for the primary care physician. Am J Med 119(3 Suppl 1):24–8.
Siu JY (2015) Communicating with mismatch and tension: treatment provision experiences of primary care doctors treating patients with overactive bladder in Hong Kong. BMC Fam Pract 16:160.
Jirschele K, Ross R, Goldberg G, Botros S (2015) Physician attitudes toward urinary incontinence identification. Female Pelvic Med Reconstr Surg 21(5):273–276.
Finkelstein K, Glosner S, Sanchez RJ, Uddin N (2008) Prevalence of probable overactive bladder in private obstetrics and gynecology group practice. Curr Med Res Opin 24(4):1083–1090.
Nguyen K, Hunter K, Wagg A (2013) Knowledge and understanding of urinary incontinence: survey of family practitioners in northern Alberta. Can Fam Physician 59:e330–e337.
Rosenberg M, Witt ES, Barkin J, Miner M (2014) A practical primary care approach to overactive bladder. Can J Urol 31 Suppl 2:2–11.
Gormley EA, Lightner DJ, Burgio KL, Chai TC, Clemens JQ, Culkin DJ et al (2012) Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline. J Urol 188(6 Suppl):2455–2463.
Kalder M, Pantazis K, Dinas K, Albert US, Heilmaier C, Kostev K (2014) Discontinuation and treatment using anticholinergic medications in patients with urinary incontinence. Obstet Gynecol 124:794–800.
Malinar AS, Rejas J, Navarro-Artieda R, Aguado-Jodar A, Ruiz-Torrejon A, Ibanez-Nolla J et al (2014) Antimuscarinic persistence patterns in newly treated patients with overactive bladder: a retrospective comparative analysis. Int Urogynecol J 25:485–492.
Kobelt G (1997) Economic considerations and outcome measurement in urge incontinence. Urology 50(6A Suppl):100–107.
Wagg A, Compion G, Fahey A, Siddiquui E (2012) Persistence with prescribed antimuscarinic therapy for overactive bladder: a UK experience. BJU Int 110:1767–1774.
Sexton CC, Notte S, Maroulis C, Dmochowski RR, Cardozo L, Subramanian D et al (2011) Persistence and adherence in the treatment of overactive bladder syndrome with anticholinergic therapy: a systemic review of the literature. Int J Clin Pract 65:567–585.
Chancellor MB, Migliaccio-Walle K, Bramley T, Chaudhari SL, Corbell C, Globe D (2013) Long-term patterns of use and treatment failure with anticholinergic agents for overactive bladder. Clin Ther 25:1744–1751.
Shaya FT, Blume S, Gu A, Zyczynski T, Jumadilova Z (2005) Persistence with overactive bladder pharmacotherapy in a Medicaid population. Am J Manag Care 11:S121–S129.
Yu TF, Nichol MB, Yu AP, Ahn J (2005) Persistence and adherence of medication for chronic overactive bladder/urinary incontinence in the California Medicaid program. Value Health 8:495–504.
Echols K, Verma U, Policaro F, Medina CA (2000) Idiopathic hyperactivity and ditropan: an efficacy and compliance issue. Obstet Gynecol 95(4 Suppl 1):S24.
Kelleher CJ, Cardozo LD, Khullar V, Salvatore S (1997) A medium-term analysis of the subjective efficacy of treatment of women with detrusor instability and low bladder compliance. Br J Obstet Gynaecol 104:988–993.
Visco AG, Brubaker L, Jelovsek E, Wilson TS, Norton P, Zyczynski HM et al (2016) Adherence to oral therapy for urgency urinary incontinence: results from the Anticholinergic versus Botox Comparison (ABC) trial. Female Pelvic Med Reconstr Surg 22:24–28.
Equator network: Enhancing the QUality and Transparency Of Health Research (2016) The STOBE guidelines. http://www.equator-network.org. Accessed 7 August 2016.
Johnston BJ (2013) The role of patient experience and its influence on adherence to anti-depressant treatment. J Psychosoc Nurs Ment Health Serv 51(12):29–37.
Smith AL, Nissim HA, Le TX, Khan A, Maliski SL, Litwin MS et al (2011) Misconceptions and miscommunication among aging women with overactive bladder symptoms. Urology 77(1):55–59.
Grimes D (2010) Epidemiologic research using administrative databases. Obstet Gynecol 116:1018–1019.
Yeaw J, Benner JS, Walt JG, Siams S, Smith DB (2009) Comparing adherence and persistence across 6 chronic medication classes. J Manag Care Pharm 15:728–740.
World Health Organization (2003) Adherence to long-term therapies: evidence for action. World Health Organization, Geneva. http://www.who.int/chp/knowledge/publications/adherence_report/en/index.html. Accessed 7 August 2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Tran, A.M., Sand, P.K., Seitz, M.J. et al. Does physician specialty affect persistence to pharmacotherapy among patients with overactive bladder syndrome?. Int Urogynecol J 28, 409–415 (2017). https://doi.org/10.1007/s00192-016-3118-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-3118-1