Abstract
Introduction and hypothesis
To determine the indications and risk factors for needing midurethral sling revision in a cohort of women undergoing midurethral sling placement.
Methods
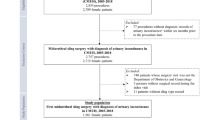
This was a case–control study of all women undergoing midurethral sling placement for stress urinary incontinence (SUI) between January 2003 and December 2013. Cases were patients who underwent midurethral sling placement followed by sling revision (incision, partial or complete excision). Controls were patients who underwent sling placement only. Once all subjects had been identified, the electronic medical record was queried for demographic and perioperative and postoperative data.
Results
Of 3,307 women who underwent sling placement, 89 (2.7 %, 95 % CI 1.9 – 3.4) underwent sling revision for one or more of the following indications: urinary retention (43.8 %), voiding dysfunction (42.7 %), recurrent urinary tract infection (20.2 %), mesh erosion (21.3 %), vaginal pain/dyspareunia (7.9 %), and groin pain (3.4 %). The median time from the index to the revision surgery was 7.8 months (2.3 – 17.9 months), but was significantly shorter in patients with urinary retention. The type of sling placed (retropubic or transobturator) was not associated with indication for revision. Patients who underwent revision surgery were more likely to have had previous SUI surgery (adjusted odds ratio 4.4, 95 % CI 1.7 – 6.5) and to have undergone concomitant vaginal apical suspension (adjusted odds ratio 2.4, 95 % CI 1.4 – 4.5).
Conclusions
The rate of sling revision after midurethral sling placement was 2.7 %. Urinary retention and voiding dysfunction were the most common indications. Patients with a history of previous SUI surgery and concomitant apical suspension at the time of sling placement may be at higher risk of requiring revision surgery.
Similar content being viewed by others
References
Shamliyan T, Wyman J, Bliss DZ, Kane RL, Wilt TJ (2007) Prevention of urinary and fecal incontinence in adults. Evid Rep Technol Assess (Full Rep) 161:1–379
Tennstedt SL, Fitzgerald MP, Nager CW et al (2007) Quality of life in women with stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 18:543–549
Erekson EA, Lopes VV, Raker CA, Sung VW (2010) Ambulatory procedures for female pelvic floor disorders in the United States. Am J Obstet Gynecol 203:497.e1–497.e5
Oliphant SS, Wang L, Bunker CH (2009) Trends in stress urinary incontinence inpatient procedures in the United States 1979–2004. Am J Obstet Gynecol 200:521.e1–521.e6
Wu JM, Gandhi MP, Shah AD, Shah JY, Fulton RG, Weidner AC (2011) Trends in inpatient urinary incontinence surgery in the USA, 1998–2007. Int Urogynecol 22:1437–1443
Jonsson Funk M, Levin P, Wu JM (2012) Trends in the surgical management of stress urinary incontinence. Obstet Gynecol 119(4):854–851
Nguyen JN, Jakus-Waldman SM, Walter AJ, White T, Menefee SA (2012) Perioperative complications and reoperations after incontinence and prolapse surgeries using prosthetic implants. Obstet Gynecol 3(119):539–546
Unger CA, Abbott S, Evans JM et al (2014) Outcomes following treatment for pelvic floor mesh complications. Int Urogynecol 25(6):745–749
Abbott S, Unger CA, Evans JM et al (2014) Evaluation and management of complications from synthetic mesh after pelvic reconstructive surgery: a multicenter study. Am J Obstet Gynecol 210(2):163.e1–163.e8
Danford JM, Osborn DJ, Reynolds WS, Biller DH, Dmochowski RR (2015) Postoperative pain outcomes after transvaginal mesh revision. Int Urogynecol J 26(1):65–69
Crosby EC, Abernathy M, Berger MB, DeLancey JO, Fenner DE, Morgan DM (2014) Symptom resolution after operative management of complications from transvaginal mesh. Obstet Gynecol 123(1):134–139
Molden S, Bracken J, Nguyen A et al (2010) A retrospective multicenter study on outcomes after midurethral polypropylene sling revision for voiding dysfunction. Female Pelvic Med Reconstr Surg 16(6):340–344
Molden S, Patterson D, Tarr M et al (2010) Risk factors leading to midurethral sling revision: a multicenter case–control study. Int Urogynecol J 21(10):1253–1259
Ridgeway B, Walters MD, Paraiso M et al (2008) Early experience with mesh excision for adverse outcomes after transvaginal mesh placement using prolapse kits. Am J Obstet Gynecol 199:703.e1–703.e7
Haylen BT, de Ridder D, Freeman RM et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 29:4–20
Brubaker L, Norton PA, Albo ME et al (2011) Adverse events over 2 years after retropubic or transobturator midurethral sling surgery: findings from the Trial of Midurethral Slings (TOMUS) study. Am J Obstet Gynecol 205(5):498.e1–498.e6
Schimpf MO, Rahn DD, Wheeler TL et al (2014) Sling surgery for stress urinary incontinence in women: a systematic review and metaanalysis. Am J Obstet Gynecol 211(1):71.e1–71.e27
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Unger, C.A., Rizzo, A.E. & Ridgeway, B. Indications and risk factors for midurethral sling revision. Int Urogynecol J 27, 117–122 (2016). https://doi.org/10.1007/s00192-015-2769-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2769-7