Abstract
Introduction and hypothesis
This study was designed to evaluate clinical outcomes ≥2 years following surgery with polypropylene mesh and vaginal support device (VSD) in women with vaginal prolapse, in a prospective, multi-center setting.
Methods
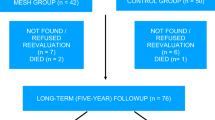
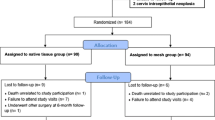
Patients re-consented for this extended follow-up (n = 110), with anatomic evaluation using Pelvic Organ Prolapse Quantification (POP-Q) and validated questionnaires to assess pelvic symptoms and sexual function. Complications were recorded (safety set; n = 121).
Results
Median length of follow-up was 29 months (range 24–34 months). The primary anatomic success, defined as POP-Q 0–I, was 69.1%; however, in 84.5% of the cases, the leading vaginal edge was above the hymen. Pelvic symptoms and sexual function improved significantly from baseline (p < 0.01). Mesh exposure rate was 9.1%. Five percent reported stress urinary incontinence and 3.3% required further prolapse surgery.
Conclusion
These results indicate this non-anchored mesh repair is a safe and effective treatment for women with symptomatic vaginal prolapse in the medium term.

Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- DRI:
-
Device run-in
- ICS POP-Q:
-
International Continence Society Pelvic Organ Prolapse Quantification
- PGI-C:
-
Patient Global Impression of Change
- PFDI-20:
-
Pelvic Floor Distress Inventory
- PFIQ-7:
-
Pelvic Floor Impact Questionnaire
- PISQ-12:
-
Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire
- QoL:
-
Quality of life
- SD:
-
Standard deviation
- US:
-
United States
- VSD:
-
Vaginal support device
References
Shah AD, Kohli N, Rajan S, Hoyte L (2008) The age distribution, rates and types of surgery for pelvic organ prolapse surgery in the USA. Int urogynaecol J 19:421–428
Smith F, Holman C, Moorin RE, Tsoko N (2010) Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol 116:1096–1100
Nygaard I, Barber MD, Burgio KL et al (2008) Prevalence of symptomatic pelvic floor disorders in US women. JAMA 300(11):1311–1316
Luber KM, Boero S, Choe JY (2001) The demographics of pelvic floor disorders: current observations and future projections. Am J Obstet Gynecol 184:1496–1503
Denman MA, Gregory WT, Boyles SH, Smith V, Edwards SR, Clark AL (2008) Reoperation 10 years after surgically managed pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 198(5):555.e1–555.e5
Withagen M, Milani AL, den Boon J, Hervest HA, Vierhout ME (2011) Trocar-guided mesh compared with conventional vaginal repair in recurrent prolapse: a randomized controlled trial. Obstet Gynecol 117:242–250
Carey M, Higgs P, Goh J et al (2009) Vaginal repair with mesh versus colporrhaphy for prolapse: a randomized controlled trial. BJOG 116(10):1380–1386
Altman D, Vayrynen T, Ellstrom-Engh M, Axelsen S, Falconer C (2011) Anterior colporrhaphy versus transvaginal mesh for pelvic organ prolapse. NEJM 364:1826–1836
Margulies RU, Lewicky-Gaupp C, Fenner DE, McGuire EJ, Clemens JQ, Delancey JO (2008) Complications requiring reoperation following vaginal mesh kit procedures for prolapse. Am J Obstet Gynecol 199(6):678.e1–678.e4
Jia X, Glazener C, Mowatt G, MacLennan G, Bain C, Fraser C, Burr J (2008) Efficacy and safety of using mesh or grafts in surgery for anterior and/or posterior vaginal wall prolapse: systematic review and meta-analysis. BJOG 115(11):1350–1361
Jacquetin B, Fatton B, Rosenthal C et al (2010) Total Trans-Vaginal-Mesh (TVM) technique for treatment of pelvic organ prolapse: a 3 year prospective follow up study. Int urogynaecol J 21:1455–1462
Miller D, Lucente V, Babin E, Beach P, Jones P, Robinson D (2011) Prospective clinical assessment of the trans-vaginal mesh (TVM) technique for treatment of pelvic organ prolapse—5 year results. Female Pelvic Med Reconstr Surg 17:139–143
Nieminen K, Hiltunen R, Takala T et al (2010) Outcomes after anterior vaginal wall repair with mesh: a randomized, controlled trial with a 3 year follow-up. Am J Obstet Gynecol 203:235.e1–235.e8
Carey M, Slack M, Higgs P, Wynn-Williams M, Cornish A (2008) Vaginal surgery for pelvic organ prolapse using mesh and a vaginal support device. BJOG 115:391–397
Reisenauer C, Shiozawa T, Huebner M, Slack M, Carey M (2010) Anatomic study of prolapse surgery using non-anchored mesh and vaginal support device. Am J Obstet Gynecol 203:590.e1–590.e7
Zyczynski HM, Carey MP, Smith ARB, Gauld JM, Robinson D, Sikirica V, Reisenauer C, Slack M (2010) One-year clinical outcomes after prolapse surgery with nonanchored mesh and vaginal support device. Am J Obstet Gynecol 203:587.e1–587.e8
Bump RC, Mattiasson A, Bo K et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Barber MD, Walters MD, Bump RC (2005) Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol 193(1):103–113
Wren PA, Janz NK, Brubaker L et al (2005) Reliability of health-related quality of life measures 1 year after surgical procedures for pelvic floor disorders. Am J Ob Gyn 192:780–788
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C (2003) A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Int urogynaecol J 14:164–168
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C (2004) Erratum: a short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Int urogynaecol J 15:219
Wild D, Grove A, Martin M et al (2005) Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health 2(8):94–104
Swift SE, Tate S, Nicholas J (2003) Correlation of symptoms with degree of pelvic organ support in a general population of women: what is pelvic organ prolapse? Am J Obstet Gynecol 189:372–379
Barber MD, Brubaker L, Nygaard I et al (2009) Defining success after surgery for pelvic organ prolapse. Obstet Gynecol 114:600–609
Boukerrou M, Rubod C, Debet B, Boodhum R, Nayama M, Cosson M (2008) Tissue resistance of the tension-free procedure: what about healing? Int urogynaecol J 19:397–400
Handa VL, Zyczynski HM, Brubaker L et al (2007) Sexual function before and after sacrocolpopexy for pelvic organ prolapse. Am J Obst Gynecol 197:629.e1–629.e6
Blandon RE, Gebhart JB, Trabuco EC, Klingele CJ (2009) Complications from vaginally placed mesh in pelvic reconstructive surgery. Int Urogynecol J Pelvic Floor Dysfunct 20:523–531
Lowman JK, Jones LA, Woodman PJ et al (2008) Does the prolift system cause dyspareunia? Am J Obstet Gynecol 199:707.e1–707.e6
Iglesia CB, Solok AI, Solok ER et al (2010) Vaginal mesh for prolapse: a randomized controlled trial. Obstet Gynecol 116:293–303
Maher CF, Feiner B, DeCuyper EM et al (2011) Laparoscopic sacral colpopexy versus total vaginal mesh for vaginal vault prolapse: a randomized trial. Am J Obstet Gynecol 204(4):360.e1–360.e7
Acknowledgments
Investigators of the Prosima Study Group are Jeanette Lim, Melbourne, Australia; Nick Franco, Naples, FL; Christian Goepel, Halle, Germany; Miles Murphy, Allentown, PA; Salil Khandwala, Dearborn, MI; Christl Reisenauer, Tübingen, Germany; Tim Sayer, Basingstoke, UK; Mark Slack, Cambridge, UK; Tony Smith, Manchester, UK; Douglas VanDrie, Grand Rapids, MI; Halina Zyczynski, Pittsburgh, PA. Members of the Clinical Development team at Ethicon who contributed to study design and implementation and the analysis of data: David Robinson, MD (Medical Director); Patricia Beach, MBA, MA (Clinical Project Manager); Colin Urquhart, BSc (Clinical Project Manager); Chris McEleney (Data Manager); David Shah (Data Manager); Linda Lin, MS (Programmer); Ailie Smith, BSc (Quality Compliance Manager).
Conflicts of interest
T. Sayer, J. Lim, D. Van Drie, M. Slack and P. Jones all have consultancy positions with Ethicon. P. Hinoul and J. Gauld are employed by Ethicon.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Sayer, T., Lim, J., Gauld, J.M. et al. Medium-term clinical outcomes following surgical repair for vaginal prolapse with tension-free mesh and vaginal support device. Int Urogynecol J 23, 487–493 (2012). https://doi.org/10.1007/s00192-011-1600-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-011-1600-3