Abstract
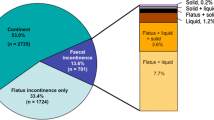
The aim of this study was to determine the prevalence of, and the changes in, anorectal symptoms following different modes of vaginal delivery in primiparous women. Six hundred and seventeen questionnaires were distributed to primiparous women 3–4 years after delivery. The questionnaires were designed to obtain information regarding the development of anorectal symptoms, including the type of symptoms experienced, their severity and their impact on lifestyle. A total of 479 questionnaires were returned, representing a response rate of 77.6%. Women included in the study were divided into three groups on the basis of the mode of delivery (normal vaginal, vacuum extraction and forceps). Any episode of fecal incontinence was considered to be abnormal. Following delivery, de novo incontinence developed in 22%. There was no significant difference between the three modes of vaginal delivery in terms of the development of fecal incontinence (normal vaginal delivery 22%, vacuum extraction 20%, forceps delivery 26%). Furthermore, analysis of obstetric variables could not identify one significant independent risk factor for anorectal incontinence. The results of this study suggest that instrumental vaginal deliveries are as safe as a normal vaginal delivery in terms of the development of anorectal symptoms.
Similar content being viewed by others
Abbreviations
- PNTML:
-
Pudendal nerve terminal motor latencies
- EMG:
-
Electromyography
References
Kamm M (1994) Obstetric damage and fecal incontinence. Lancet 344:730–772
Parks AG, Swash M, Urich H (1977) Sphincter denervation in anorectal incontinence and rectal prolapse. Gut 18:656–665
Sultan MA, Kamm MA (1997) Faecal incontinence after childbirth Br J Obstet Gynaecol 104:979–982
Sørensen M, Tetzschner T, Rasmussen OO, Bjarnesen J, Christiansen J (1993) Sphincter rupture in childbirth. Br J Surg 80:392–394
Sultan AH, Kamm MA, Hudson CN, Bartram CI (1994) Third degree obstetric anal sphincter tears: risk factors and outcome of primary repair. Br Med J 308:887–891
Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI (1993) Anal sphincter disruption during vaginal delivery. N Engl J Med 329:1905–1911
Smith ARB, Hosker GL, Warrel DW (1998) The role of partial denervation of the pelvic floor in etiology genitourinary prolapse and stress incontinence of urine. A neurophysiological study. Br J Obstet Gynaecol 96:24–28
Bek KM, Laurberg S (1992) Risk of anal incontinence from subsequent vaginal delivery after a complete obstetric anal sphincter tear. Br J Obstet Gynaecol 99: 742–726
Snooks SJ, Swash M, Sechell M, Henry MM (1984) Injury to innervation of pelvic floor sphincter musculature in childbirth. Lancet 2:546–550
Parks AG (1975) Anorectal incontinence. J Roy Soc Med 68:21–30
MacArthur C, Bick DE, Keighley MRB (1997) Faecal incontinence after childbirth. Br J Obstet Gynaecol 104:44–50
Fynes M, Donnolly V, Behan M, Oçonnoll PR, O'Herlihy C (1999) Effect of second vaginal delivery on anorectal physiology and faecal incontinence: a prospective study. Lancet 345:983–986
Poen AC, Felt-Bersma RJF, Dekker GA, Devillé W, Cuesta MA, Meuwissen SGM (1997) Third degree obstetric perineal tears: risk factors and the preventive role of mediolateral episiotomy. Br J Obstet Gynaecol 104:563–566
Hadeem K, Ohrlander S, Lingman G (1988) Long-term ailments due to anal sphincter rupture caused by delivery – a hidden problem. Eur J Obstet Gynaecol Reprod Biol 27:27–32
Zetterström JP, López A, Anzén B, Dolk A, Norman M, Mellgren A (1999) Anal incontinence after vaginal delivery: a prospective study in primiparous women. Br J Obstet Gynaecol 106:324–330
Leeuw de JW, Struijck PC, Vierhout ME, Wallenburg HCS (2001) Risk factors for third degree perineal ruptures during delivery. Br J Obstet Gynaecol 108:383–387
Acknowledgements
We wish to thank Dr. R. Euser (clinical data), Dr. H.J.A. Wijnne (statistical analysis, Department of Epidemiology, University of Utrecht ) and Mrs. Y. Farinazo-van der Put for assisting in the preparation of this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Editorial Comment: This is a well-written article that addresses an important issue in obstetrics and gynecology, i.e. the likely consequences of defective anal sphincter function after pregnancy and delivery. As the authors emphasize, the article suffers from the fact that this was a retrospective study. Furthermore, it would have been very interesting to know the differences between patients undergoing cesarean section and those giving birth vaginally. In two recently published investigations there were no differences between cesarean section and normal vaginal delivery in terms of fecal and urinary incontinence post partum. We still do not know how to identify patients who are at risk of developing incontinence after pregnancy and delivery.
Rights and permissions
About this article
Cite this article
Schraffordt Koops, S.E., Vervest, H.A.M. & Oostvogel, H.J.M. Anorectal symptoms after various modes of vaginal delivery. Int Urogynecol J 14, 244–249 (2003). https://doi.org/10.1007/s00192-003-1040-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-003-1040-9