Abstract
Purpose
Due to low incidence of isolated lateral osteoarthritis (OA), there are limited data on whether a fixed-bearing (FB) or a mobile-bearing (MB) design is superior for lateral unicompartmental knee replacement (UKR). The aim of this matched-pairs analysis was to compare both designs in terms of implant survival and clinical outcome.
Methods
Patients who received MB-UKR (Group A) and FB-UKR (Group B) at a single centre were matched according to gender, age at time of surgery and body mass index (BMI). Survivorship analysis was performed with the endpoint set as “revision for any reason”. Clinical outcome was assessed using the Oxford knee score (OKS), visual analogue scale for pain (VAS), patients’ satisfaction, University of California Los Angeles activity scale (UCLA) and the Tegner activity score (TAS).
Results
A total of 60 matched pairs were included with a mean follow-up (FU) of 3.4 ± 1.3 (range 1.2–5.0) years in Group A and 2.7 ± 1.2 (range 1.0–5.0) years in Group B. Survivorship between both groups differed significantly (Group A: 78.7%; Group B: 98.3%, p = 0.003) with bearing dislocation being the most common reason for revision in Group A (46.2%). The relative and absolute risk reduction were 92.2% and 20%, respectively, with 5 being the number needed to treat. There were no differences in OKS (Group A: 41.6 ± 6.5; Group B: 40.4 ± 7.7), VAS (Group A: 2.9 ± 3.2; Group B: 1.6 ± 2.2), UCLA (Group A: 5.7 ± 1.3; Group B: 5.9 ± 1.8) and TAS (Group A: 3.0 ± 1.0; Group B: 3.1 ± 1.2) between both groups on follow-up.
Conclusion
Despite modern prosthesis design and surgical technique, implant survival of lateral MB-UKR is lower than that of FB-UKR on the short- to mid-term due to bearing dislocation as the most common cause of failure. Since clinical results are equivalent in both groups, FB-UKR should be preferred in treatment of isolated lateral OA.
Level of evidence
Retrospective case–control study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
After failure of joint-preserving methods, unicompartmental knee replacement (UKR) is recognised as a safe treatment option in end-stage unicompartimental knee osteoarthritis (OA) [29]. The indications for UKR have been extended to younger patients since initially introduced by Kozinn and Scott in 1989 [19, 30]. Due to several advantages compared to total knee replacement (TKR), such as a greater range-of-motion (ROM), faster recovery and lower perioperative morbidity, usage of UKR has increased over the last decades and is expected to increase even more [16, 20]. While many studies reported high survivorship and good clinical outcomes for mobile-bearing (MB) UKR in the medial compartment [8, 25, 27], initial results for lateral MB-UKR were disappointing with a survival rate of only 82% after 5 years [12]. The main cause of failure was dislocation of the bearing [12]. Further studies have attributed this contrast to the different anatomy and biomechanics of the lateral compared to the medial compartment [26, 37]. Therefore, the Oxford domed lateral (ODL) was introduced with a modified surgical technique to account for the aforementioned differences [28, 43]. However, bearing dislocation remains a recurrent complication with dislocation rates up to 8.5% [17, 34, 41]. As an alternative to the ODL prosthesis, the Oxford fixed lateral (OFL) prosthesis was developed as a fixed-bearing (FB) design, which also allows the use of a minimally invasive surgical technique [40]. To date, there are only few studies reporting the use of lateral FB-UKR with small cohorts and wide variations in clinical outcome and survivorship [22, 31, 33, 35]. Recent systematic analyses showed lowest revision rates for metal-backed FB-UKR in lateral UKR [9, 36]. However, these studies report on a variety of different prosthesis designs as well as register-based studies, that are known to include results from low-volume surgeons. Hence, there is a high risk that these results may be confounded by prosthesis choice as well as surgical technique, and experience. Additionally, there are currently no studies comparing clinical outcome of both designs in contemporary lateral UKR. To provide more evidence on the influence of bearing choice in lateral UKR, the aim of this study was to compare survivorship and clinical outcome in matched patients who underwent lateral UKR with either MB- or FB-UKR for isolated lateral OA at one institution using the same prosthesis and surgical technique.
The authors hypothesised that FB-UKR for isolated lateral OA would be superior to MB-UKR in terms of survivorship while demonstrating similar clinical outcome.
Materials and methods
Ethical approval was obtained from the institutional review boards of the University of Heidelberg (S-265-2014, S-293-2021) and the study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013. Informed consent was obtained from all participating patients.
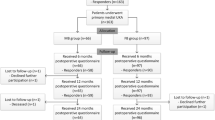
The present study retrospectively analyses prospectively collected data from a series of patients who underwent UKR for isolated lateral OA in one institution. A total 258 UKR were implanted, subdivided into 115 MB-UKR (Group A) between 2006 and 2014 and 143 FB-UKR (Group B) between 2014 and 2020. In group A, the ODL (Zimmer Biomet Inc., Warsaw, Indiana, USA) was used as the MB-UKR and in group B, the OFL (Zimmer Biomet Inc., Warsaw, Indiana, USA) was used as the FB-UKR. Patients were assigned based on the timing of surgery, as the use of the ODL was discontinued in favour of the OFL in 2014 due to recurrent bearing dislocations at the authors institution.
To improve comparability, patients in groups A and B were matched according to gender, age at time of surgery and body mass index (BMI) in a 1:1 ratio. Patients were divided into six age groups (< 50, 50–54, 55–59, 60–64, 65–70, > 70 years) and three BMI groups (< 25, 25–30, > 30 kg/m2). To form matched pairs, patients had to be the same gender, in the same age and BMI group [39]. If more than two patients from both groups matched all three parameters, the pair with the closest age at the time of surgery was selected [1]. Matching was performed blinded with respect to outcome parameters and independently by two different authors (MH, TW), resulting in the same matched pairs.
To minimise a possible influence of large differences in follow-up (FU) duration between matches, only patients with a FU of at least 1 year and at most 5 years were included. Patients with missing postoperative data were excluded from the study.
In both groups, the primary indication for surgery was severe osteoarthritis of the lateral compartment with full thickness articular cartilage loss (“bone-on-bone”) or avascular necrosis of the femoral condyle. In all cases, the anterior cruciate ligament (ACL) as well as the medial (MCL) and lateral collateral ligaments (LCL) were functionally intact, the valgus deformity was manually correctable to ensure that no ligaments were rigid and there was no evidence of OA in the medial compartment on varus stress radiographs. OA of the patellofemoral joint was not considered a contraindication unless there was a deep eburnation or bone grooving on the medial facet of the patella. Rheumatoid arthritis, fixed valgus deformity, previous osteotomy, or a flexion deformity > 15° were considered contraindications [40].
All surgeries were performed using a minimally invasive surgical technique (MIS) through a lateral parapatellar approach without dislocation of the patella. Internal rotation of the tibial plateau and anatomical positioning of the femoral component were considered to avoid elevation of the joint line. Bearing thickness was selected in full extension. Depending on the bone quality, the use of a cemented or uncemented fixation of the femoral component was chosen, whereas the tibial component was always cemented in both groups [40, 41]. An intravenous single-shot antibiotic (1.5 g cefuroxime) was administered perioperatively. Postoperative rehabilitation was standardised for all patients. From the first postoperative day, immediate full weight bearing was possible. No restriction in active and passive knee movement was set. Discharge was followed by 3 weeks of inpatient or outpatient rehabilitation.
All procedures were performed by or under supervision of 8 senior surgeons with high experiences in unicompartmental knee replacement (≥ 15 UKR/year).
Survivorship analysis was performed with the endpoint “revision for any reason” defined as any operation in which at least one of the components was replaced.
The Oxford knee score (OKS) was obtained at the regular follow-up examination. These regular FU examinations are routinely performed at 1, 3 and 5 years postoperatively in all patients receiving an arthroplasty at our institution. Pain level was assessed using a visual analogue scale (VAS) ranging from 0 to 10 (0 = no pain, 10 = worst pain experienced). Postoperative satisfaction was evaluated using a numeric scale ranging from 1 (highly satisfied) to 5 (unsatisfied). The University of California Los Angeles activity scale (UCLA) and the Tegner activity score (TAS) were used to assess patients’ physical activity after surgery [5, 44]. Patients who were unable to attend the clinical FU were contacted by telephone for a structured interview to assess the aforementioned questionaries.
Statistical analysis
Data were collected and analysed using SPSS version 29.0 (SPSS Inc., Chicago, IL). The primary endpoint was implant survivorship and secondary endpoints were clinical outcomes.
The empirical distribution of continuous variables was described using mean and standard deviation (SD), possible differences between the two groups were examined with the Mann–Whitney-U Test and differences between preoperative and postoperative values were analysed with the Wilcoxon signed rank test. Survivorship analysis was performed with the Kaplan–Meier estimator. Survival rates between the two groups were compared using the log-rank test. For all tests, the significance level was set at p < 0.05. A priori power analysis for medium effect size with a type 1 error (two sided) of 0.05 and a power of 80% yielded a minimum number of 45 cases for each group.
Results
A total of 60 matched pairs were included in the analysis after matching with gender, age at time of surgery and BMI (Fig. 1). These matching parameters showed no significant differences between both groups. In addition, the mean preoperative OKS between both groups showed no significant difference (p < 0.05, Table 1). Patient demographics are shown in Table 1.
Survivorship analysis
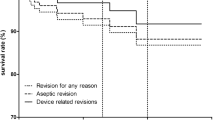
There were 14 revision surgeries in the present study, of which 13 (21.7%) were in group A and one (1.7%) in group B. Considering these event rates in both groups, we calculated a relative risk reduction of 92.2% and an absolute risk reduction of 20.0% resulting in a number needed to treat of 5, which means that 5 patients have to be treated with lateral FB-UKR to prevent one patient from having revision surgery. This results in a survival rate of 78.7% at 3.4 years (number at risk: 28) for group A and a survival rate of 98.3% at 2.7 years (number at risk: 26) for group B. Survival rates between both groups showed a significant difference (p = 0.003) (Fig. 2).
The different reasons for revision are demonstrated in Table 2.
Treatment options in Group A included revision to TKR (7 cases/53.8%), bearing exchange (3 cases/23.1%), revision to the FB design (2 cases/ 15.4%) and screw insertion into the intercondylar notch (1 case/ 7.7%). In group B, revision to TKR was performed.
Clinical outcome
While there was a significant improvement in the OKS from pre- to postoperative values in both groups, there were no significant differences in the postoperative patient-reported outcome measurements (PROMs) between the two groups at final FU (Table 3, Fig. 3).
There was no significant difference in patients’ satisfaction between the two groups (p = 0.078, Fig. 4).
Discussion
The main finding of the present study is that implant survival with the endpoint “revision for any reason” following lateral FB-UKR is significantly better than following lateral MB-UKR while demonstrating similar clinical results.
This is the first comparative study to analyse the influence of bearing choice in lateral UKR on survivorship and clinical outcome in a single high-volume institution using the same prosthesis.
The findings of this study are consistent with the aforementioned systematic analyses, in which metal-backed FB-UKR showed lowest revision rates for lateral UKR [9, 36].
Almost half of the revisions in group A were due to bearing dislocation despite the use of the modified surgical technique described earlier [28, 32]. The dislocation rate of 10% is noticeable higher than in previous reports, even if all surgeries were performed by well-experienced senior surgeons who were familiar with the modified surgical technique [41, 42]. In contrast, survivorship of FB-UKR for the endpoint “revision for any reason” was significantly higher with 98.3% at 2.7 years than for MB-UKR and is in line with other recent studies of lateral FB-UKR [3, 35].
A common reason for revision in both groups was persistence of pain. Objective causes of revision such as aseptic loosening, infection, instability, or OA progression could not be identified in any of the present cases. Treatment of these patients remains challenging since the threshold for revision surgery in UKR is lower than in TKR, even in patients with similar OKS scores [21] and the outcome after revision surgery for unexplained pain is worse than revision for an identified reason [18].
OA progression and aseptic loosening are usually causes of failure in late years, so the FU period in the present study may not be representative. Still, there was one case of each in group A in early years. Overcorrection of valgus malalignment is associated with a higher risk of OA progression and may be considered as a possible explanation in this case [2]. Burger et al. demonstrated higher revision rates due to OA progression in lateral MB-UKR than in lateral FB-UKR and concluded that there is a tendency to overstuff the lateral compartment to prevent bearing dislocation [7]. In contrast, overstuffing may also lead to knee laxity due to soft tissue stretching, which increases the risk of bearing dislocation [11]. This highlights the importance of precise component alignment and ligamentous balancing in MB-UKR, suggesting that this design is more prone to surgeon related errors [14]. Since bearing dislocation is not possible with a FB design, the requirements for ligamentous balancing are not as crucial as for MB-UKR. In recent years, robotic-assisted UKR has emerged and has shown improved implant positioning compared with the conventional technique [4] as well as good clinical outcome and survivorship [10, 15]. However, an advantage of robotic-assisted lateral UKR over conventional technique in terms of survivorship and clinical outcome has not yet been demonstrated [23]. To what extent robotics can optimise intraoperative balancing to decrease bearing dislocations remains unclear and needs to be further investigated.
There were no significant differences between the two groups in the clinical results. Both achieved high mean OKS scores postoperatively consistent with previous results for lateral MB-UKR [28, 34, 42], lateral FB-UKR [3, 35] as well as medial UKR [24]. Furthermore, no significant differences were found in postoperative pain level and patients’ satisfaction between both groups demonstrating equivalent clinical results for both designs despite the theoretical biomechanical advantages of MB-UKR. Similar results were demonstrated by Burger et al. in a systematic analysis of 28 studies involving 2265 lateral UKRs [6].
One aim of UKR is to restore patients’ activity level, which is not always consistent with clinical outcomes [44]. The current literature provides limited data on patient’s activity level after lateral UKR, but shows that moderate activity levels are possible, especially in low impact activities such as cycling, swimming, and hiking [13, 38, 45]. This study shows no differences in the activity rating scales assessed between both groups and, therefore, suggests that both designs enable good activity levels after UKR.
This study has several limitations. First, a small sample size was reported in a retrospective study design with a well-known risk of selection bias. Randomised controlled studies are generally preferable, but because of the rare surgical indications of isolated lateral OA, they are unlikely to be practically feasible with good power.
Second, the FU period is limited to a short- to mid-term period, so causes of failure in late years, such as OA progression and aseptic loosening, may be not representative in this study and a longer FU is necessary. Third, PROMs were collected at different time points, ranging from 1 to 5 years. Collecting data at the same timepoint would have strengthened the data.
Fourth, radiographic analysis of alignment and implant positioning was not reported because it was not the purpose this study. Nevertheless, this could lead to a better understanding in patients who need revision surgery or whose clinical outcome is worse and should be further investigated in the future. Fifth, the number of patients who received different treatment because of concomitant patellofemoral OA during the study period is unknown. Since the extent of patellofemoral OA is not always clear, the decision may have varied from surgeon to surgeon in some cases. However, it is not expected to have had a significant influence on the results of this study. Finally, this multi-surgeon study comprises results from a single centre with high experience in UKR. Multicenter or registry-based studies would constitute more generalised data. Nevertheless, lateral UKR may never be a widely used treatment option since its indication is very rare and surgical procedure is different than for medial UKR.
Conclusion
Despite modern prosthesis design and surgical technique, implant survival of lateral MB-UKR is lower than that of FB-UKR on the short- to mid-term due to bearing dislocation as the most common cause of failure. Since clinical results are equivalent in both groups, FB-UKR should be preferred in treatment of isolated lateral OA.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- FB:
-
Fixed bearing
- FU:
-
Follow-up
- LCL:
-
Lateral collateral ligament
- MB:
-
Mobile bearing
- MCL:
-
Medial collateral ligament
- MIS:
-
Minimally invasive surgical technique
- OA:
-
Osteoarthritis
- ODL:
-
Oxford domed lateral
- OFL:
-
Oxford fixed lateral
- OKS:
-
Oxford knee score
- PROM:
-
Patient-reported outcome measurements
- ROM:
-
Range-of-motion
- TAS:
-
Tegner activity score
- TKR:
-
Total knee replacement
- UCLA:
-
The University of California Los Angeles activity scale
- UKR:
-
Unicompartmental knee replacement
- VAS:
-
Visual analogue scale for pain
References
Afghanyar Y, Klug A, Rehbein P, Dargel J, Drees P, Kutzner KP (2021) One-stage bilateral versus unilateral short-stem total hip arthroplasty: a matched-pair analysis of 216 hips. J Orthop 27:130–136
Argenson JN, Parratte S, Bertani A, Flecher X, Aubaniac JM (2008) Long-term results with a lateral unicondylar replacement. Clin Orthop Relat Res 466:2686–2693
Asadollahi S, Wilson HA, Thomson FR, Vaz K, Middleton R, Jenkins C et al (2022) Early results of fixed-bearing unicompartmental knee replacement designed for the lateral compartment. J Orthop Surg Res 17:146
Batailler C, White N, Ranaldi FM, Neyret P, Servien E, Lustig S (2019) Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 27:1232–1240
Briggs KK, Steadman JR, Hay CJ, Hines SL (2009) Lysholm score and Tegner activity level in individuals with normal knees. Am J Sports Med 37:898–901
Burger JA, Kleeblad LJ, Sierevelt IN, Horstmann WG, Nolte PA (2019) Bearing design influences short- to mid-term survivorship, but not functional outcomes following lateral unicompartmental knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 27:2276–2288
Burger JA, Kleeblad LJ, Sierevelt IN, Horstmann WG, van Geenen RCI, van Steenbergen LN et al (2020) A comprehensive evaluation of lateral unicompartmental knee arthroplasty short to mid-term survivorship, and the effect of patient and implant characteristics: an analysis of data from the Dutch arthroplasty register. J Arthroplast 35:1813–1818
Burnett RS, Nair R, Hall CA, Jacks DA, Pugh L, McAllister MM (2014) Results of the Oxford Phase 3 mobile bearing medial unicompartmental knee arthroplasty from an independent center: 467 knees at a mean 6-year follow-up: analysis of predictors of failure. J Arthroplast 29:193–200
Fratini S, Meena A, Alesi D, Cammisa E, Zaffagnini S, MarcheggianiMuccioli GM (2022) Does implant design influence failure rate of lateral unicompartmental knee arthroplasty? A meta-analysis. J Arthroplast 37(985–992):e983
Gaudiani MA, Samuel LT, Diana JN, DeBattista JL, Coon TM, Moore RE et al (2023) Robotic-arm assisted lateral unicompartmental knee arthroplasty: 5-Year outcomes & survivorship. J Orthop Surg (Hong Kong) 31:10225536221138986
Gulati A, Weston-Simons S, Evans D, Jenkins C, Gray H, Dodd CA et al (2014) Radiographic evaluation of factors affecting bearing dislocation in the domed lateral Oxford unicompartmental knee replacement. Knee 21:1254–1257
Gunther TV, Murray DW, Miller R, Wallace DA, Carr AJ, O’Connor JJ et al (1996) Lateral unicompartmental arthroplasty with the Oxford meniscal knee. Knee 3:33–39
Hariri M, Hagemann M, Mick P, Deisenhofer J, Panzram B, Innmann M et al (2023) Physical activity of young patients following minimally invasive lateral unicompartmental knee replacement. J Clin Med 12:635
Hariri M, Hauer G, Smolle M, Sadoghi P, Leithner A, Panzram B et al (2022) Mobile bearing versus fixed bearing medial unicompartmental knee replacement: an independent two center matched-pairs analysis. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04629-5
Heckmann ND, Antonios JK, Chen XT, Kang HP, Chung BC, Piple AS et al (2022) Midterm survivorship of robotic-assisted lateral unicompartmental knee arthroplasty. J Arthroplast 37:831–836
Kahlenberg CA, Richardson SS, Gruskay JA, Cross MB (2021) Trends in utilization of total and unicompartmental knee arthroplasty in the United States. J Knee Surg 34:1138–1141
Kennedy JA, Mohammad HR, Yang I, Mellon SJ, Dodd CAF, Pandit HG et al (2020) Oxford domed lateral unicompartmental knee arthroplasty. Bone Jt J 102-B:1033–1040
Kerens B, Boonen B, Schotanus MG, Lacroix H, Emans PJ, Kort NP (2013) Revision from unicompartmental to total knee replacement: the clinical outcome depends on reason for revision. Bone Jt J 95-B:1204–1208
Kozinn SC, Scott R (1989) Unicondylar knee arthroplasty. J Bone Jt Surg Am 71:145–150
Liddle AD, Judge A, Pandit H, Murray DW (2014) Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet 384:1437–1445
Liddle AD, Pandit H, Judge A, Murray DW (2015) Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Jt J 97-B:793–801
Lustig S, Lording T, Frank F, Debette C, Servien E, Neyret P (2014) Progression of medial osteoarthritis and long term results of lateral unicompartmental arthroplasty: 10 to 18 year follow-up of 54 consecutive implants. Knee 21(Suppl 1):S26-32
Maritan G, Franceschi G, Nardacchione R, Furlan E, Mariani I, Ursino N et al (2023) Similar survivorship at the 5-year follow-up comparing robotic-assisted and conventional lateral unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 31:1063–1071
Mohammad HR, Kennedy JA, Mellon SJ, Judge A, Dodd CA, Murray DW (2020) Ten-year clinical and radiographic results of 1000 cementless Oxford unicompartmental knee replacements. Knee Surg Sports Traumatol Arthrosc 28:1479–1487
Mohammad HR, Strickland L, Hamilton TW, Murray DW (2018) Long-term outcomes of over 8000 medial Oxford phase 3 Unicompartmental knees-a systematic review. Acta Orthop 89:101–107
Nakagawa S, Kadoya Y, Todo S, Kobayashi A, Sakamoto H, Freeman MA et al (2000) Tibiofemoral movement 3: full flexion in the living knee studied by MRI. J Bone Jt Surg Br 82:1199–1200
Pandit H, Hamilton TW, Jenkins C, Mellon SJ, Dodd CA, Murray DW (2015) The clinical outcome of minimally invasive phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. Bone Jt J 97-B:1493–1500
Pandit H, Jenkins C, Beard DJ, Price AJ, Gill HS, Dodd CA et al (2010) Mobile bearing dislocation in lateral unicompartmental knee replacement. Knee 17:392–397
Pandit H, Jenkins C, Gill HS, Barker K, Dodd CA, Murray DW (2011) Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Jt Surg Br 93:198–204
Pandit H, Jenkins C, Gill HS, Smith G, Price AJ, Dodd CA et al (2011) Unnecessary contraindications for mobile-bearing unicompartmental knee replacement. J Bone Jt Surg Br 93:622–628
Pennington DW, Swienckowski JJ, Lutes WB, Drake GN (2006) Lateral unicompartmental knee arthroplasty: survivorship and technical considerations at an average follow-up of 12.4 years. J Arthroplast 21:13–17
Robinson BJ, Rees JL, Price AJ, Beard DJ, Murray DW, McLardy Smith P et al (2002) Dislocation of the bearing of the Oxford lateral unicompartmental arthroplasty. A radiological assessment. J Bone Jt Surg Br 84:653–657
Sah AP, Scott RD (2007) Lateral unicompartmental knee arthroplasty through a medial approach. Study with an average five-year follow-up. J Bone Jt Surg Am 89:1948–1954
Schelfaut S, Beckers L, Verdonk P, Bellemans J, Victor J (2013) The risk of bearing dislocation in lateral unicompartmental knee arthroplasty using a mobile biconcave design. Knee Surg Sports Traumatol Arthrosc 21:2487–2494
Smith JR, Robinson JR, Porteous AJ, Murray JR, Hassaballa MA, Artz N et al (2014) Fixed bearing lateral unicompartmental knee arthroplasty–short to midterm survivorship and knee scores for 101 prostheses. Knee 21:843–847
Tay ML, Matthews BG, Monk AP, Young SW (2022) Disease progression, aseptic loosening and bearing dislocations are the main revision indications after lateral unicompartmental knee arthroplasty: a systematic review. J ISAKOS 7:132–141
Tokuhara Y, Kadoya Y, Nakagawa S, Kobayashi A, Takaoka K (2004) The flexion gap in normal knees. An MRI study. J Bone Jt Surg Br 86:1133–1136
Walker T, Gotterbarm T, Bruckner T, Merle C, Streit MR (2015) Return to sports, recreational activity and patient-reported outcomes after lateral unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23:3281–3287
Walker T, Gotterbarm T, Bruckner T, Merle C, Streit MR (2014) Total versus unicompartmental knee replacement for isolated lateral osteoarthritis: a matched-pairs study. Int Orthop 38:2259–2264
Walker T, Hariri M, Eckert J, Panzram B, Reiner T, Merle C et al (2020) Minimally invasive lateral unicompartmental knee replacement: early results from an independent center using the Oxford fixed lateral prosthesis. Knee 27:235–241
Walker T, Zahn N, Bruckner T, Streit MR, Mohr G, Aldinger PR et al (2018) Mid-term results of lateral unicondylar mobile bearing knee arthroplasty: a multicentre study of 363 cases. Bone Jt J 100-B:42–49
Weston-Simons JS, Pandit H, Kendrick BJ, Jenkins C, Barker K, Dodd CA et al (2014) The mid-term outcomes of the Oxford Domed Lateral unicompartmental knee replacement. Bone Jt J 96-B:59–64
Yang I, Hamilton TW, Mellon SJ, Murray DW (2021) Systematic review and meta-analysis of bearing dislocation in lateral meniscal bearing unicompartmental knee replacement: Domed versus flat tibial surface. Knee 28:214–228
Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC (1998) Assessing activity in joint replacement patients. J Arthroplast 13:890–895
Zimmerer A, Navas L, Kinkel S, Weiss S, Hauschild M, Miehlke W et al (2021) Sports activity and patient-related outcomes after fixed-bearing lateral unicompartmental knee arthroplasty. Knee 28:64–71
Funding
Open Access funding enabled and organized by Projekt DEAL. Open Access funding enabled and organised by Projekt DEAL. The authors have not received specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. MH contributed to acquisition, analysis and interpretation of data and drafted the manuscript and figures. NZ, PM and AJ performed data collection, and revised the manuscript critically. TW performed the statistical analysis and revised the manuscript critically. MI and TR (Tobias Reiner) participated in the study design and helped to draft the manuscript. TR (Tobias Renkawitz) drafted the manuscript and revised it critically.
Corresponding author
Ethics declarations
Conflict of interest
The author TR (Tobias Renkawitz) has received research support and personal fees from Arbeitsgemeinschaft Endoprothetik (AE), DGOU, DGOOC; BVOU, DePuy International, Otto Bock Foundation, Deutsche Arthrose Hilfe, Aesculap, Zimmer, Stiftung Oskar Helene Heim Berlin, VielberthFoundation Regensburg, the German Ministry of Education and Research as well as the German Federal Ministry of Economic Cooperation and Development. He is Medical Director and Chair at the Orthopaedic Department at Heidelberg University Hospital, board member of the German Society for Orthopaedics and Trauma (DGOOC) and vice president of the Professional Association of Orthopaedic Specialists and Trauma Surgeons (BVOU). The other authors declare that they have no competing interests.
Ethical approval
Ethical approval was obtained from the institutional review boards of the University of Heidelberg (S-265-2014, S-293-2021) and the study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013. Informed consent was obtained from all participating patients.
Informed consent
Informed consent was obtained from all participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hariri, M., Zahn, N., Mick, P. et al. Fixed-bearing is superior to mobile-bearing in lateral unicompartmental knee replacement: a retrospective matched-pairs analysis. Knee Surg Sports Traumatol Arthrosc 31, 3947–3955 (2023). https://doi.org/10.1007/s00167-023-07417-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07417-9