Abstract
Purpose
Valgus knees have inferior outcomes compared to varus knees. There is little data regarding soft-tissue balance in flexion which may influence outcome in valgus knees undergoing TKA. The purpose of this study was to evaluate whether there is imbalance between medial and lateral flexion gaps in valgus deformity. A secondary aim was to compare soft-tissue balance in knees with valgus deformity less than 10° with those exceeding 10°. The null hypothesis was that there was no soft-tissue imbalance in 90° of flexion irrespective of magnitude of deformity.
Methods
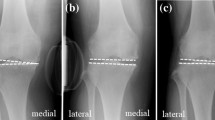
64 valgus knees (52 female and 12 male) with deformity from 0.5 to 27.5° (mean 188.77, SD 6.21) were studied in 54 patients (mean age 67.81 y, SD 8.69) undergoing navigated TKA. Medial and lateral gaps in extension and at 90° of flexion were compared (using Independent-samples t test) between knees with valgus < 10° with those > 10° using a validated dynamic method after resection of cruciates, menisci and osteophytes, and then after final trialling.
Results
Mean initial medial–lateral (ML) gap difference in extension was 2.63 mm (SD 2.63) and 2.09 mm (SD 3.78) in flexion, being tighter laterally. Initial ML gap differences in extension and flexion correlated with valgus deformity (R = − 0.514; p = 0.00001; R = − 0.325; p = 0.01, respectively). Initial ML gap differences in extension correlated with those in flexion (R = 0.42; p = 0.0005). Mean ML flexion and extension gap differences were 1.30 mm (SD 3.67) and 1.26 mm (SD 1.92) in knees with < 10° valgus, and 3.17 mm (SD 3.71) and 4.29 mm (SD 2.45) in those > 10° valgus; p values were 0.026 and < 0.001 respectively.
Conclusion
The lateral flexion gap in valgus knees may be narrower than the medial flexion gap, especially in knees with > 10° deformity. This contrasts with native and varus knees, in which it exceeds the medial gap. This novel study indicates the need to identify valgus knees with lateral flexion gap tightness by distracting the posterior femoral condyles from the proximal tibia by dynamic stressing of the soft-tissues after resection of cruciates, menisci, and osteophytes, with the knee flexed to 90°. These findings, highlighting the need for restoring flexion gap balance, may improve the inferior outcomes in valgus knees.
Level of evidence
IV.






Similar content being viewed by others
References
Aunan E, Kibsgard T, Clarke-Jenssen J, Rohrl SM (2012) A new method to measure ligament balancing in total knee arthroplasty: laxity measurements in 100 knees. Arch Orthop Trauma Surg 132:1173–1181
Azukizawa M, Kuriyama S, Nakamura S, Nishitani K, Lyman S, Morita Y, Furu M, Ito H, Matsuda S (2018) Intraoperative medial joint laxity in flexion decreases patient satisfaction after total knee arthroplasty. Arch Orthop Trauma Surg 138:1143–1150
Baier C, Benditz A, Koeck F, Keshmiri A, Grifka J, Maderbacher G (2018) Different kinematics of knees with varus and valgus deformities. J Knee Surg 31:264–269
Bellemans J, Vandenneucker H, Vanlauwe J, Victor J (2010) The influence of coronal plane deformity on mediolateral ligament status: an observational study in varus knees. Knee Surg Sport Traumatol Arthrosc 18:152–156
Blakeney W, Beaulieu Y, Puliero B, Kiss M-O, Vendittoli P-A (2020) Bone resection for mechanically aligned total knee arthroplasty creates frequent gap modifications and imbalances. Knee Surg Sport Traumatol Arthrosc 28:1532–1541
Creaby MW, Wrigley TV, Lim BW, Bowles KA, Metcalf BR, Hinman RS, Bennell KL (2010) Varus-valgus laxity and passive stiffness in medial knee osteoarthritis. Arthritis Care Res 62:1237–1243
Delport H, Labey L, De CR, Innocenti B, Vander J, Bellemans J (2013) Collateral ligament strains during knee joint laxity evaluation before and after TKA. Clin Biomech 28:777–782
Golladay GJ, Bradbury TL, Gordon AC, Fernandez-Madrid IJ, Krebs VE, Patel PD, Suarez JC, Higuera Rueda CA, Barsoum WK (2019) Are patients more satisfied with a balanced total knee arthroplasty? J Arthroplasty 34:S195–S200
Graichen H, Lekkreusuwan K, Eller K, Grau T, Hirschmann MT, Scior W (2021) A single type of varus knee does not exist: morphotyping and gap analysis in varus OA. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06688-4
Gu Y, Howell SM, Hull ML (2017) Simulation of total knee arthroplasty in 5° or 7° valgus: a study of gap imbalances and changes in limb and knee alignments from native. J Orthop Res 35:2031–2039
Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR (2014) Primary TKA patients with quantifiably balanced soft-tissue achieve significant clinical gains sooner than unbalanced patients. Adv Orthop. https://doi.org/10.1155/2014/628695
Heesterbeek PJC, Verdonschot N, Wymenga AB (2008) In vivo knee laxity in flexion and extension: a radiographic study in 30 older healthy subjects. Knee 15:45–49
Lee DS, Song EK, Seon JK, Park SJ (2011) Effect of balanced gap total knee arthroplasty on intraoperative laxities and femoral component rotation. J Arthroplasty 26:699–704
Mazzotti A, Perna F, Golinelli D, Quattrini I, Stea S, Bordini B, Faldini C (2019) Preoperative valgus deformity has twice the risk of failure as compared to varus deformity after total knee arthroplasty. Knee Surg Sport Traumatol Arthrosc 27:3041–3047
McAuliffe MJ, Connor PBO, Garg G, Whitehouse SL, Crawford RW, Phty B (2018) Highly satisfied total knee arthroplasty patients display a wide range of soft tissue balance. J Knee Surg 33:247–254
McAuliffe MJ, Roe J, Garg G, Whitehouse SL, Crawford R (2016) The varus osteoarthritic knee has no coronal contractures in 90 degrees of flexion. J Knee Surg 30:297–303
McEwen P, Balendra G, Doma K (2019) Medial and lateral gap laxity differential in computer-assisted kinematic total knee arthroplasty. Bone Jt J 101B:331–339
Mehliß V, Leira MS, Olaizola AS, Scior W, Graichen H (2018) Proven accuracy for a new dynamic gap measurement in navigated TKA. Knee Surg Sport Traumatol Arthrosc 27:1189–1195
Minoda Y, Iwaki H, Ikebuchi M, Yoshida T, Nakamura H (2012) The flexion gap preparation does not disturb the modified gap technique in posterior stabilized total knee arthroplasty. Knee 19:832–835
Moon Y, Kim H, Ahn H, Park C, Lee D (2016) Comparison of soft tissue balancing, femoral component rotation, and joint line change between the gap balancing and measured resection techniques in primary total knee arthroplasty: a meta-analysis. Med 95:1–7
Mullaji A (2020) Can isolated removal of osteophytes achieve correction of varus deformity and gap-balance in computer-assisted total knee arthroplasty? An analysis of navigation data. Bone Jt J 102B:49–58
Niki Y, Takeda Y, Kanagawa H, Iwamoto W, Matsumoto H, Enomoto H, Toyama Y, Suda Y (2012) Effects of four different surgical approaches on intra-operative joint gap in posterior-stabilized total knee arthroplasty. Knee Surg Sport Traumatol Arthrosc 20:2026–2031
Nodzo SR, Franceschini V, Cruz DS, Gonzalez Della Valle A (2018) The flexion space is more reliably balanced when using the transepicondylar axis as compared to the posterior condylar line. Knee Surg Sport Traumatol Arthrosc 26:3265–3271
Nodzo SR, Staub TM, Jancuska JM, Cobler-Lichter MD, Boyle KK, Rachala S (2020) Flexion space balancing through component positioning and its relationship to traditional anatomic rotational landmarks in robotic total knee arthroplasty. J Arthroplasty 35:1569–1575
Mullaji AB, Bhoskar R, Singh A, Haidermota M (2021) Valgus arthritic knees can be classified into nine phenotypes. Knee Surg Sport Traumatol Arthros. https://doi.org/10.1007/s00167-021-06796-1
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AM conceived the study, wrote and reviewed the manuscript: AS collected the data, analysed the data, and reviewed the manuscript; MH helped collect the data, help analyse the data, and reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
Institutional Ethics Committee approval: Number P8/2016.
Informed consent
Informed consent was taken from all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mullaji, A., Singh, A. & Haidermota, M. Arthritic knees with more than 10° valgus can have soft-tissue imbalance in flexion. Knee Surg Sports Traumatol Arthrosc 30, 2905–2914 (2022). https://doi.org/10.1007/s00167-021-06798-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06798-z