Abstract
Purpose
Simulator arthroscopy training has gained popularity in recent years. However, it remains unclear what level of competency surgeons may achieve in what time frame using virtual training. It was hypothesized that 10 h of training would be sufficient to reach the target level defined by experts based on the Diagnostic Arthroscopic Skill Score (DASS).
Methods
The training concept was developed by ten instructors affiliated with the German-speaking Society of Arthroscopy and Joint Surgery (AGA). The programme teaches the basics of performing arthroscopy; the main focus is on learning and practicing manual skills using a simulator. The training was based on a structured programme of exercises designed to help users reach defined learning goals. Initially, camera posture, horizon adjustment and control of the direction of view were taught in a virtual room. Based on these skills, further training was performed with a knee model. The learning progress was assessed by quantifying the exercise time, camera path length and instrument path length for selected tasks. At the end of the course, the learners’ performance in diagnostic arthroscopy was evaluated using DASS. Participants were classified as novice or competent based on the number of arthroscopies performed prior to the assessment.
Results
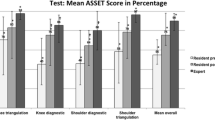
Except for one surgeon, 131 orthopaedic residents and surgeons (29 women, 102 men) who participated in the seven courses agreed to anonymous data analysis. Fifty-eight of them were competents with more than ten independently performed arthroscopies, and 73 were novices, with fewer than ten independently performed arthroscopies. There were significant reductions in exercise time, camera path length and instrument path length for all participants after the training, indicating a rapid increase in performance. No difference in camera handling between the dominant and non-dominant sides was found in either group. The competents performed better than the novices in various tasks and achieved significantly better DASS values on the final performance test.
Conclusions
Our data have demonstrated that arthroscopic skills can be taught effectively on a simulator, but a 10-h course is not sufficient to reach the target level set by experienced arthroscopists. However, learning progress can be monitored more objectively during simulator training than in the operating room, and simulation may partially replace the current practice of arthroscopic training.
Level of evidence
III.






Similar content being viewed by others
References
Aïm F, Lonjon G, Hannouche D, Nizard R (2016) Effectiveness of virtual reality training in orthopaedic surgery. Arthroscopy 32:224–232
Akhtar K, Sugand K, Wijendra A, Standfield NJ, Cobb JP, Gupte CM (2015) Training safer surgeons: How do patients view the role of simulation in orthopaedic training? Patient Saf Surg 9:11. https://doi.org/10.1186/s13037-015-0058-5
Anetzberger H, Becker R, Eickhoff H, Seibert FJ, Döring B, Haasters F, Mohr M, Reppenhagen S (2021) The Diagnostic Arthroscopy Skill Score (DASS) – a reliable and suitable assessment tool for arthroscopic skill training. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06554-3
Anetzberger H, Mohr M, Eickhoff HJ, Seibert FJ, Döring B, Reppenhagen S (2021) Drei Jahre AGA Simulator Training Arthroskopie. Ein Erfahrungsbericht. Arthroskopie. https://doi.org/10.1007/s00142-020-00428-5
Bartlett JD, Lawrence JE, Stewart ME, Nakano N, Khanduja V (2018) Does virtual reality simulation have a role in training trauma and orthopaedic surgeons? Bone Jt J 100-B:559–565
Baumann Q, Hardy A, Courage O, Lacombes P, Accadbled F (2019) Lessons taught by a knee arthroscopy simulator about participants in a European arthroscopy training programme. Orthop Traumatol Surg Res 105:287–291
Bouaicha S, Epprecht S, Jentzsch T, Ernstbrunner L, El Nashar R, Rahm S (2020) Three days of training with a low-fidelity arthroscopy triangulation simulator box improves task performance in a virtual reality high-fidelity virtual knee arthroscopy simulator. Knee Surg Sports Traumatol Arthrosc 28:862–868
Boutefnouchet T, Laios T (2016) Transfer of arthroscopic skills from computer simulation training to the operating theatre: a review of evidence from two randomised controlled studies. SICOT J 2:4. https://doi.org/10.1051/sicotj/2015039
Camp CL (2018) Editorial Commentary: “Virtual Reality” simulation in orthopaedic surgery: realistically helpful, or virtually useless? Arthroscopy 34:1678–1679
Camp CL, Krych AJ, Stuart MJ, Regnier TD, Mills KM, Turner NS (2016) Improving resident performance in knee arthroscopy: a prospective value assessment of simulators and cadaveric skills laboratories. J Bone Jt Surg Am 98:220–225
Cannon WD, Garrett WE Jr, Hunter RE, Sweeney HJ, Eckhoff DG, Nicandri GT, Hutchinson MR, Johnson DD, Bisson LJ, Bedi A, Hill JA, Koh JL, Reinig KD (2014) Improving residency training in arthroscopic knee surgery with use of a virtual-reality simulator. A randomized blinded study. J Bone Jt Surg Am 96:1798–1806
Cychosz CC, Tofte JN, Johnson A, Gao Y, Phisitkul P (2018) Fundamentals of arthroscopic surgery training program improves knee arthroscopy simulator performance in arthroscopic trainees. Arthroscopy 34:1543–1549
Fitts PM, Posner MI (1967) Human performance. Brooks/Cole Pub. Co, Belmont
Garfjeld Roberts P, Guyver P, Baldwin M, Akhtar K, Alvand A, Price AJ, Rees JL (2017) Validation of the updated ArthroS simulator: face and construct validity of a passive haptic virtual reality simulator with novel performance metrics. Knee Surg Sports Traumatol Arthrosc 25:616–625
Jung K, Kang DJ, Kekatpure AL, Adikrishna A, Hong J, Jeon IH (2016) A new wide-angle arthroscopic system: a comparative study with a conventional 30° arthroscopic system. Knee Surg Sports Traumatol Arthrosc 24:1722–1729
Kagerer FA, Contreras-Vidal IL, Stelmach GE (1997) Adaptation to gradual as compared with sudden visuo-motor distortions. Exp Brain Res 115:537–561
Magill RA, Hall KG (1990) A review of the contextual interference effect in motor skill acquisition. Hum Mov Sci 9:241–289
Pedowitz RA (2017) Virtual reality surgical simulation for arthroscopy training. J Med Educ Train 1:008
Rahm S, Wieser K, Bauer DE, Waibel FW, Meyer DC, Gerber C, Fucentese SF (2018) Efficacy of standardized training on a virtual reality simulator to advance knee and shoulder arthroscopic motor skills. BMC Musculoskelet Disord 16(19):150. https://doi.org/10.1186/s12891-018-2072-0
Rashed S, Ahrens PM, Maruthainar N, Garlick N, Saeed MZ (2018) The role of arthroscopic simulation in teaching surgical skills: a systematic review of the literature. JBJS Rev 6:e8. https://doi.org/10.2106/JBJS.RVW.17.00201
Shea JB, Morgan RL (1979) Contextual interference effects on the acquisition, retention, and transfer of a motor skill. J Exp Psychol Learn Mem Cogn 5:179–187
St. Pierre P (2018) Editorial Commentary: proficiency-based training: are we ready for a new way to train and test orthopaedic surgeons? Arthroscopy 34:2199–2200
Stunt JJ, Kerkhoffs GM, van Dijk CN, Tuijthof GJM (2015) Validation of the ArthroS virtual reality simulator for arthroscopic skills. Knee Surg Sports Traumatol Arthrosc 23:3436–3442
Thut G, Cook ND, Regard M, Leenders KL, Halsband U, Landis T (1996) Intermanual transfer of proximal and distal motor engrams in humans. Exp Brain Res 108:321–327
Tofte JN, Westerlind BO, Martin KD, Guetschow BL, Uribe-Echevarria B, Rungprai C, Phisitkul P (2017) Knee, shoulder, and fundamentals of arthroscopic surgery training: validation of a virtual arthroscopy Simulator. Arthroscopy 33:641–646
Walbron P, Common H, Thomazeau H, Hosseini K, Peduzzi L, Bulaid Y, Sirveaux F (2020) Virtual reality simulator improves the acquisition of basic arthroscopy skills in first-year orthopedic surgery residents. Orthop Traumatol Surg Res 106:717–724
Wang KC, Bernardoni ED, Cotter EJ, Cole BJ, Verma NN, Romeo AA, Bush-Joseph CA, Bach BR, Frank RM (2019) Impact of simulation training on diagnostic arthroscopy performance: a randomized controlled trial. Arthrosc Sports Med Rehabil 1:e47–e57. https://doi.org/10.1016/j.asmr.2019.07.002
Wittmann M, Kagerer F, Poeppel E (1999) Wie, wann und was können wir lernen? Zeitlichen und räumliche Merkmale sensomotorischer Koordination. Zentralbl Chir 124:876–883
Yari SS, Jandhyala CK, Sharareh B, Athiviraham A, Shybut TB (2018) Efficacy of a virtual arthroscopic simulator for orthopaedic surgery residents by year in training. Orthop J Sports Med. https://doi.org/10.1177/2325967118810176
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the ethical committee of the Bavarian State Chamber of Physicians (BLÄK) (approval number: 2021-1033).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anetzberger, H., Reppenhagen, S., Eickhoff, H. et al. Ten hours of simulator training in arthroscopy are insufficient to reach the target level based on the Diagnostic Arthroscopic Skill Score. Knee Surg Sports Traumatol Arthrosc 30, 1471–1479 (2022). https://doi.org/10.1007/s00167-021-06648-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06648-y