Abstract
Purpose
To compare the clinical outcomes of patients who underwent successful nonoperative treatment for type III-V acromioclavicular joint (ACJ) injuries to those who eventually required conversion to anatomic coracoclavicular ligament reconstruction (ACCR) at a minimum 5-year follow-up.
Methods
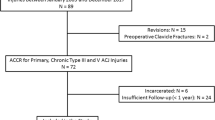
Patients with primary, chronic type III-V ACJ injuries who either underwent successful conservative treatment or conversion to ACCR after failing a trail of conservative management between 2003 and 2014 with a minimum 5-year follow-up were included in the study. Clinical outcome measures comprised the American Shoulder and Elbow Surgeons (ASES) and Simple Shoulder Test (SST) score, collected preoperatively and at final visit for the ACCR group. Outcome scores for patients with successful conservative treatment were only collected at final visit. A Self- Assessment Numeric Evaluation (SANE) score was obtained at terminal follow-up for both groups.
Results
Twenty-two patients (mean age: 40.1 ± 15.6 years) with successful nonoperative treatment and twenty-one patients (mean age: 43.6 ± 12.0 years) who required conversion to ACCR were included in the study. At final follow-up, patients with successful non-operative treatment achieved similar ASES (93.0±12.0NonOP vs. 86.1±16.8ACCR), SST (11.2±1.4NonOP vs. 10.7±2.0ACCR) and SANE scores (80.9±19.7NonOPvs. 90.5±14.7ACCR) compared to those who were converted to ACCR. Additionally, patients who underwent conversion to ACCR showed significant improvement in ASES (49.8±18.1pre vs. 86.1±16.8post; Δ36.3±19.7) and SST scores (6.5±3.2prevs. 10.7±2.0post; Δ4.2±4.0) from pre- to postoperative.
Conclusion
At a minimum 5-year follow-up, patients with successful non-operative treatment for type III-V ACJ injuries achieved similar clinical outcomes compared to those who were converted to ACCR. In patients with chronic severe ACJ dislocation a trial of conservative treatment may be attempted, astime from injuryto eventual conversion to ACCR had no significant influence on postoperative clinical outcomes.
Level of evidence
Level IV.



Similar content being viewed by others
References
Beitzel K, Cote MP, Apostolakos J, Solovyova O, Judson CH, Ziegler CG et al (2013) Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy 29:387–397
Beitzel K, Mazzocca AD, Bak K, Itoi E, Kibler WB, Mirzavan R et al (2014) ISAKOS upper extremity committee consensus statement on the need for diversification of the Rockwood classification for acromioclavicular joint injuries. Arthroscopy 30:271–278
Berthold DP, Muench LN, Dyrna F, Uyeki CL, Cote MP, Imhoff AB et al (2020) Radiographic alterations in clavicular bone tunnel width following anatomic coracoclavicular ligament reconstruction (ACCR) for chronic acromioclavicular joint injuries. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-05980-z
Carbone S, Postacchini R, Gumina S (2015) Scapular dyskinesis and SICK syndrome in patients with a chronic type III acromioclavicular dislocation. Results of rehabilitation. Knee Surg Sports Traumatol Arthrosc 23:1473–1480
Carofino BC, Mazzocca AD (2010) The anatomic coracoclavicular ligament reconstruction: surgical technique and indications. J Shoulder Elbow Surg 19:37–46
Cote MP, Wojcik KE, Gomlinski G, Mazzocca AD (2010) Rehabilitation of acromioclavicular joint separations: operative and nonoperative considerations. Clin Sports Med 29(213–228):vii
Dunphy TR, Damodar D, Heckmann ND, Sivasundaram L, Omid R, Hatch GF 3rd (2016) Functional outcomes of type V acromioclavicular injuries with nonsurgical treatment. J Am Acad Orthop Surg 24:728–734
Dyrna F, Berthold DP, Feucht MJ, Muench LN, Martetschlager F, Imhoff AB et al (2019) The importance of biomechanical properties in revision acromioclavicular joint stabilization: a scoping review. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05742-6
Frank RM, Cotter EJ, Leroux TS, Romeo AA (2019) Acromioclavicular joint injuries: evidence-based treatment. J Am Acad Orthop Surg. https://doi.org/10.5435/JAAOS-D-17-00105
Gowd AK, Liu JN, Cabarcas BC, Cvetanovich GL, Garcia GH, Manderle BJ et al (2019) Current concepts in the operative management of acromioclavicular dislocations: a systematic review and meta-analysis of operative techniques. Am J Sports Med 47:2745–2758
Gumina S, Carbone S, Postacchini F (2009) Scapular dyskinesis and SICK scapula syndrome in patients with chronic type III acromioclavicular dislocation. Arthroscopy 25:40–45
Izadpanah K, Weitzel E, Honal M, Winterer J, Vicari M, Maier D et al (2012) In vivo analysis of coracoclavicular ligament kinematics during shoulder abduction. Am J Sports Med 40:185–192
Kibler WB, Sciascia A (2010) Current concepts: scapular dyskinesis. Br J Sports Med 44:300–305
Korsten K, Gunning AC, Leenen LP (2014) Operative or conservative treatment in patients with Rockwood type III acromioclavicular dislocation: a systematic review and update of current literature. Int Orthop 38:831–838
Lippitt SB, Harryman DT, Matsen FA (1993) A practical tool for evaluating function: the simple shoulder test. In: Matsen FA, Fu FH, Hawkins RJ (eds) The shoulder: a balance of mobility and stability. American Academy of Orthopaedic Surgeons, Rosemont, IL, pp 501–518
Mazzocca AD, Arciero RA, Bicos J (2007) Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med 35:316–329
Mazzocca AD, Conway JE, Johnson S, Rios CG, Dumonski ML, Santangelo SA et al (2004) The anatomic coracoclavicular ligament reconstruction. Oper Tech Sports Med 12:56–61
Millett PJ, Horan MP, Warth RJ (2015) Two-year outcomes after primary anatomic coracoclavicular ligament reconstruction. Arthroscopy 31:1962–1973
Moatshe G, Kruckeberg BM, Chahla J, Godin JA, Cinque ME, Provencher MT et al (2018) Acromioclavicular and coracoclavicular ligament reconstruction for acromioclavicular joint instability: a systematic review of clinical and radiographic outcomes. Arthroscopy 34(1979–1995):e1978
Muench LN, Kia C, Jerliu A, Murphy M, Berthold DP, Cote MP et al (2019) Functional and radiographic outcomes after anatomic coracoclavicular ligament reconstruction for type III/V acromioclavicular joint injuries. Orthop J Sports Med 7:2325967119884539
Nissen CW, Chatterjee A (2007) Type III acromioclavicular separation: results of a recent survey on its management. Am J Orthop (Belle Mead NJ) 36:89–93
Petri M, Warth RJ, Greenspoon JA, Horan MP, Abrams RF, Kokmeyer D et al (2016) Clinical results after conservative management for grade III acromioclavicular joint injuries: does eventual surgery affect overall outcomes? Arthroscopy 32:740–746
Richards R, An KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG et al (1994) A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg 3:347–352
Rockwood CA (1984) Injuries to the acromioclavicular joint: subluxations and dislocations about the shoulder. In: RC A, Green DP (eds) Fractures in adults. J. B. Lippincott, Philadelphia, pp 860–910
Seo Y-J, Yoo Y-S, Noh K-C, Song S-Y, Lee Y-B, Kim H-J et al (2012) Dynamic function of coracoclavicular ligament at different shoulder abduction angles: a study using a 3-dimensional finite element model. Arthroscopy 28:778–787
Smith TO, Chester R, Pearse EO, Hing CB (2011) Operative versus non-operative management following Rockwood grade III acromioclavicular separation: a meta-analysis of the current evidence base. J Orthop Traumatol 12:19–27
Tamaoki MJ, Lenza M, Matsunaga FT, Belloti JC, Matsumoto MH, Faloppa F (2019) Surgical versus conservative interventions for treating acromioclavicular dislocation of the shoulder in adults. Cochrane Database Syst Rev 10:CD007429
Tischer T, Salzmann GM, El-Azab H, Vogt S, Imhoff AB (2009) Incidence of associated injuries with acute acromioclavicular joint dislocations types III through V. Am J Sports Med 37:136–139
Trainer G, Arciero RA, Mazzocca AD (2008) Practical management of grade III acromioclavicular separations. Clin J Sport Med 18:162–166
Verstift DE, Welsink CL, Spaans AJ, van den Bekerom MPJ (2019) Return to sport after surgical treatment for high-grade (Rockwood III–VI) acromioclavicular dislocation. Knee Surg Sports Traumatol Arthrosc 27:3803–3812
Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC (1999) Comparison of the single assessment numeric evaluation method and two shoulder rating scales. Am J Sports Med 27:214–221
Xará-Leite F, Andrade R, Moreira PS, Coutinho L, Ayeni OR, Sevivas N et al (2019) Anatomic and non-anatomic reconstruction improves post-operative outcomes in chronic acromio-clavicular instability: a systematic review. Knee Surg Sports Traumatol Arthrosc 27:3779–3796
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declare that they have no conflict of interest.
Funding
ADM receives research support and consulting fees from Arthrex Inc. (Naples, FL). KB is a consultant for Arthrex Inc. (Naples, FL). MPC receives personal fees from the Arthroscopy Association of North America (AANA) for the Arthroscopy Journal. The authors LNM, DPB, CU, CK, ABI, and SC have nothing to disclose.
Ethical approval
Ethical approval was not required for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Muench, L.N., Berthold, D.P., Uyeki, C. et al. Conversion to anatomic coracoclavicular ligament reconstruction (ACCR) shows similar clinical outcomes compared to successful non-operative treatment in chronic primary type III to V acromioclavicular joint injuries. Knee Surg Sports Traumatol Arthrosc 29, 2264–2271 (2021). https://doi.org/10.1007/s00167-020-06159-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06159-2