Abstract
Purpose
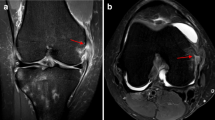
To determine the prevalence of a deep lateral femoral notch sign (LFNS) in magnetic resonance imaging (MRI) in patients with anterior cruciate ligament (ACL) and concomitant posterior root tears of the lateral meniscus (PLRT).
Methods
A retrospective chart review was conducted to identify all patients undergoing ACL reconstruction between 2016 and 2018. Based on the arthroscopic appearance of the lateral meniscus, patients were assorted to one of three groups: isolated ACL tear (ACL-Group), ACL tear with concomitant lateral meniscus tear not involving the posterolateral root (Meniscus-Group), and ACL tear with concomitant PLRT (PLRT-Group). Incidence and depth of a LFNS on preoperative MRI was compared between the three cohorts.
Results
115 patients (mean age: 29.5 ± 11.3 years) were included in the study, with 58 patients (50.4%) assorted to the ACL-Group, 24 patients (20.9%) to the Meniscus-Group, and 33 patients (28.7%) to the PLRT-Group. The prevalence of a LFNS was significantly higher in the PLRT-Group (39.4%), when compared to the ACL- (5.2%) or Meniscus-Groups (25.0%; p < 0.001, respectively). Additionally, logistic regression analysis demonstrated that patients with PLRT were 5.3 times more likely to have a LFNS as compared to those without a lateral root tear (p < 0.001).
Conclusion
In patients with ACL tears, the presence of a LFNS on preoperative MRI may be predictive for a PLRT. As the LFNS occurs in almost 40% of the patients with combined ACL tears and PLRT, the LFNS may be a useful secondary diagnostic finding in early MRI diagnostic. Identifying PLRT on MRI is clinically relevant, as it prevents misdiagnosis and facilitates surgical decision-making, thus avoiding subsequent delayed treatment.
Level of evidence
Level IV.



Similar content being viewed by others
References
Anderson L, Watts M, Shapter O, Logan M, Risebury M, Duffy D et al (2010) Repair of radial tears and posterior horn detachments of the lateral meniscus: minimum 2-year follow-up. Arthroscopy 26:1625–1632
Bhatia S, LaPrade CM, Ellman MB, LaPrade RF (2014) Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med 42:3016–3030
Brody JM, Lin HM, Hulstyn MJ, Tung GA (2006) Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology 239:805–810
Chhadia AM, Inacio MCS, Maletis GB, Csintalan RP, Davis BR, Funahashi TT (2011) Are meniscus and cartilage injuries related to time to anterior cruciate ligament reconstruction? Am J Sports Med 39:1894–1899
Choi S-H, Bae S, Ji SK, Chang MJ (2012) The MRI findings of meniscal root tear of the medial meniscus: emphasis on coronal, sagittal and axial images. Knee Surg Sports Traumatol Arthrosc 20:2098–2103
Cobby M, Schweitzer M, Resnick D (1992) The deep lateral femoral notch: an indirect sign of a torn anterior cruciate ligament. Radiology 184:855–858
De Smet AA, Blankenbaker DG, Kijowski R, Graf BK, Shinki K (2009) MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. AJR Am J Roentgenol 192:480–486
De Smet AA, Mukherjee R (2008) Clinical, MRI, and arthroscopic findings associated with failure to diagnose a lateral meniscal tear on knee MRI. AJR Am J Roentgenol 190:22–26
Feucht MJ, Bigdon S, Mehl J, Bode G, Muller-Lantzsch C, Sudkamp NP et al (2015) Risk factors for posterior lateral meniscus root tears in anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 23:140–145
Forkel P, Herbort M, Sprenker F, Metzlaff S, Raschke M, Petersen W (2014) The biomechanical effect of a lateral meniscus posterior root tear with and without damage to the meniscofemoral ligament: efficacy of different repair techniques. Arthroscopy 30:833–840
Frank JM, Moatshe G, Brady AW, Dornan GJ, Coggins A, Muckenhirn KJ et al (2017) Lateral meniscus posterior root and meniscofemoral ligaments as stabilizing structures in the ACL-deficient knee: a biomechanical study. Orthop J Sports Med 5:2325967117695756
Garth WP Jr, Greco J, House MA (2000) The lateral notch sign associated with acute anterior cruciate ligament disruption. Am J Sports Med 28:68–73
Granan L-P, Bahr R, Lie SA, Engebretsen L (2009) Timing of anterior cruciate ligament reconstructive surgery and risk of cartilage lesions and meniscal tears: a cohort study based on the Norwegian National Knee Ligament Registry. Am J Sports Med 37:955–961
Herbst E, Hoser C, Tecklenburg K, Filipovic M, Dallapozza C, Herbort M et al (2015) The lateral femoral notch sign following ACL injury: frequency, morphology and relation to meniscal injury and sports activity. Knee Surg Sports Traumatol Arthrosc 23:2250–2258
Hodel S, Kabelitz M, Tondelli T, Vlachopoulos L, Sutter R, Fucentese SF (2019) Introducing the lateral femoral condyle index as a risk factor for anterior cruciate ligament injury. Am J Sports Med 47:2420–2426
Hoffelner T, Pichler I, Moroder P, Osti M, Hudelmaier M, Wirth W et al (2015) Segmentation of the lateral femoral notch sign with MRI using a new measurement technique. BMC Musculoskelet Disord 16:217
Kanakamedala AC, Burnham JM, Pfeiffer TR, Herbst E, Kowalczuk M, Popchak A et al (2018) Lateral femoral notch depth is not associated with increased rotatory instability in ACL-injured knees: a quantitative pivot shift analysis. Knee Surg Sports Traumatol Arthrosc 26:1399–1405
Keene GC, Bickerstaff D, Rae PJ, Paterson RS (1993) The natural history of meniscal tears in anterior cruciate ligament insufficiency. Am J Sports Med 21:672–679
Kim JH, Chung JH, Lee DH, Lee YS, Kim JR, Ryu KJ (2011) Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy 27:1644–1653
Knapik DM, Salata MJ, Voos JE, Greis PE, Karns MR (2020) Role of the meniscofemoral ligaments in the stability of the posterior lateral meniscus root after injury in the ACL-deficient knee. JBJS Rev 8:e0071
Koenig JH, Ranawat AS, Umans HR, DiFelice GS (2009) Meniscal root tears: diagnosis and treatment. Arthroscopy 25:1025–1032
Kohn D, Moreno B (1995) Meniscus insertion anatomy as a basis for meniscus replacement: a morphological cadaveric study. Arthroscopy 11:96–103
Krych AJ, Wu IT, Desai VS, Murthy NS, Collins MS, Saris DBF et al (2018) High rate of missed lateral meniscus posterior root tears on preoperative magnetic resonance imaging. Orthop J Sports Med 6:2325967118765722–2325967118765722
LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF (2014) Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am 96:471–479
LaPrade RF, Ho CP, James E, Crespo B, LaPrade CM, Matheny LM (2015) Diagnostic accuracy of 3.0 T magnetic resonance imaging for the detection of meniscus posterior root pathology. Knee Surg Sports Traumatol Arthrosc 23:152–157
LaPrade RF, Matheny LM, Moulton SG, James EW, Dean CS (2017) Posterior meniscal root repairs: outcomes of an anatomic transtibial pull-out technique. Am J Sports Med 45:884–891
Laundre BJ, Collins MS, Bond JR, Dahm DL, Stuart MJ, Mandrekar JN (2009) MRI accuracy for tears of the posterior horn of the lateral meniscus in patients with acute anterior cruciate ligament injury and the clinical relevance of missed tears. AJR Am J Roentgenol 193:515–523
Lee YG, Shim J-C, Choi YS, Kim JG, Lee GJ, Kim HK (2008) Magnetic resonance imaging findings of surgically proven medial meniscus root tear: tear configuration and associated knee abnormalities. J Comput Assist Tomogr 32:452–457
Lodewijks P, Delawi D, Bollen TL, Dijkhuis GR, Wolterbeek N, Zijl JAC (2019) The lateral femoral notch sign: a reliable diagnostic measurement in acute anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc 27:659–664
Mall NA, Chalmers PN, Moric M, Tanaka MJ, Cole BJ, Bach BR Jr et al (2014) Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 42:2363–2370
Matheny LM, Ockuly AC, Steadman JR, LaPrade RF (2015) Posterior meniscus root tears: associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc 23:3127–3131
Novaretti JV, Lian J, Patel NK, Chan CK, Cohen M, Musahl V et al (2020) Partial lateral meniscectomy affects knee stability even in anterior cruciate ligament-intact knees. J Bone Joint Surg Am. https://doi.org/10.2106/jbjs.19.00712
Pao DG (2001) The lateral femoral notch sign. Radiology 219:800–801
Patel SA, Hageman J, Quatman CE, Wordeman SC, Hewett TE (2014) Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: a systematic review. Sports Med 44:281–293
Petersen W, Forkel P, Feucht MJ, Zantop T, Imhoff AB, Brucker PU (2014) Posterior root tear of the medial and lateral meniscus. Arch Orthop Trauma Surg 134:237–255
Schillhammer CK, Werner FW, Scuderi MG, Cannizzaro JP (2012) Repair of lateral meniscus posterior horn detachment lesions: a biomechanical evaluation. Am J Sports Med 40:2604–2609
Seo HS, Lee SC, Jung KA (2011) Second-look arthroscopic findings after repairs of posterior root tears of the medial meniscus. Am J Sports Med 39:99–107
Shelbourne KD, Roberson TA, Gray T (2011) Long-term evaluation of posterior lateral meniscus root tears left in situ at the time of anterior cruciate ligament reconstruction. Am J Sports Med 39:1439–1443
Shybut TB, Vega CE, Haddad J, Alexander JW, Gold JE, Noble PC et al (2015) Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament–deficient knee. Am J Sports Med 43:905–911
Smith JP III, Barrett GR (2001) Medial and lateral meniscal tear patterns in anterior cruciate ligament-deficient knees: a prospective analysis of 575 tears. Am J Sports Med 29:415–419
Warren R (1990) The lateral notch sign of anterior cruciate ligament insufficiency. Am J Knee Surg 1:119–124
West RV, Kim JG, Armfield D, Harner CD (2004) Lateral meniscal root tears associated with anterior cruciate ligament injury: classification and management (SS-70). Arthroscopy 20:e32–e33
Funding
No funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. BDP, MF, MLN, CV. were responsible for acquisition of data and writing of the manuscript. BDP, FMJ, H E. and MN. contributed to analysis and interpretation of data. IAB and HE contributed as important reviewers of the manuscript. All authors approved the final version of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors Berthold DP., Muench LN, Herbst E, Mayr F, Chadayammuri, V Imhoff AB, Feucht MJ declare that they have no conflict of interest.
Ethical approval
Ethical approval was obtained via Human Research Determination Form to the institutional review board (IRB) of the Technical University of Munich (IRB #606/19S).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Berthold, D.P., Muench, L.N., Herbst, E. et al. High prevalence of a deep lateral femoral notch sign in patients with anterior cruciate ligament (ACL) and concomitant posterior root tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc 29, 1018–1024 (2021). https://doi.org/10.1007/s00167-020-06071-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06071-9